
u
DME Procedure Codes &
Coverage Guidelines
New York State Medicaid, Durable Medical Equipment,
Prosthetics, and Orthotics
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
2
New York State Medicaid
Office of Health Insurance Programs
Department of Health
CONTACTS:
eMedNY URL
https://www.emedny.org/
ePACES Reference Guide
https://www.emedny.org/selfhelp/ePACES/PDFS/5010_ePACES_Professional_Real_Time_Claim_Reference_Guide.pdf
GDIT
(800) 343-9000
Billing Questions, Remittance Clarification, Request for Claim Forms, ePACES Enrollment, Electronic Claim
Submission Support (eXchange, FTP), Provider Enrollment
Bureau of Medical Review
(800) 342-3005
OHIPMEDPA@health.ny.gov
Prior Approval; Policies and Procedures concerning Durable Medical Equipment, Prosthetics, Orthotics, and Medical
Supplies
All eMedNY Contact Information
eMedNY Contacts PDF
NYRx Medicaid Helpline
(800) 541-2831
Pharmacy Benefits and Coverage website
https://member.emedny.org/pharmacy/benefits

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
3
Table of Contents
Document Control Properties .......................................................................................................................................................................... 6
DMEPOS Policy Manual ..................................................................................................................................................................................... 6
3.0 NEW FOR 2024 .............................................................................................................................................................................................. 6
Procedure Codes .............................................................................................................................................................................................. 6
Deleted/Replacement Codes ........................................................................................................................................................................ 7
Criteria/Guidelines ........................................................................................................................................................................................... 8
Frequency ........................................................................................................................................................................................................... 8
Fees ...................................................................................................................................................................................................................... 8
Change in Authorization Type ..................................................................................................................................................................... 8
4.0 General Information and Instructions ..................................................................................................................................................... 9
Fees ...................................................................................................................................................................................................................... 9
Standards ........................................................................................................................................................................................................... 9
Federal Law ........................................................................................................................................................................................................ 9
Purchases............................................................................................................................................................................................................ 9
Brand Names ..................................................................................................................................................................................................... 9
Modifiers ............................................................................................................................................................................................................. 9
Quantity ............................................................................................................................................................................................................. 11
Frequency .......................................................................................................................................................................................................... 11
Dispensing ......................................................................................................................................................................................................... 11
4.1, 4.2, 4.3 Medical Supplies, Enteral Therapy, Hearing Aid Battery................................................................................................... 11
4.4 Durable Medical Equipment .................................................................................................................................................................... 12
Hospital Beds and Accessories .................................................................................................................................................................. 12
Pressure Reducing Support Surfaces ....................................................................................................................................................... 15
IPPB Machines ................................................................................................................................................................................................. 16
Oxygen Systems ............................................................................................................................................................................................. 16
Respiratory Care ............................................................................................................................................................................................. 18
Ventilators ........................................................................................................................................................................................................20
Positive Airway Pressure Devices ..............................................................................................................................................................22
RESPIRATORY ASSIST DEVICES .................................................................................................................................................................23
Airway Clearance Devices ............................................................................................................................................................................23
Traction Equipment, Various ..................................................................................................................................................................... 24
Walkers (Any Width) .....................................................................................................................................................................................25
Pediatric Gait Trainers ................................................................................................................................................................................... 27

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
4
Wheeled Mobility Equipment (WME), Seating And Positioning Components (SPC) ................................................................28
Codes and descriptions: .............................................................................................................................................................................. 34
Back-up Manual Wheelchair ....................................................................................................................................................................... 37
Codes, Descriptions, and Code Specific Criteria .................................................................................................................................. 48
Miscellaneous Durable Medical Equipmen ............................................................................................................................................62
Hospital Grade Breast Pump ......................................................................................................................................................................63
Apnea Monitor............................................................................................................................................................................................... 64
Seat Lift Mechanism ..................................................................................................................................................................................... 64
E1399 Examples: .............................................................................................................................................................................................65
Home Standing Systems ..............................................................................................................................................................................66
Pneumatic Compression Device (PCD) ....................................................................................................................................................68
Safety Equipment ........................................................................................................................................................................................... 70
TENS and Osteogenesis Stimulator .......................................................................................................................................................... 70
Infusion Pumps ............................................................................................................................................................................................... 72
Topical Hyperbaric Oxygen Chamber ...................................................................................................................................................... 73
Negative Pressure Wound Therapy .......................................................................................................................................................... 75
Speech Generating Devices ........................................................................................................................................................................ 78
External Infusion Pump Batteries...............................................................................................................................................................85
Automatic External Defibrillator ................................................................................................................................................................85
Vacuum Erection Device ..............................................................................................................................................................................85
Larynx and Trachea Prosthetics and Accessories .................................................................................................................................85
Enuresis Alarm ................................................................................................................................................................................................85
Positioning Car Seat ......................................................................................................................................................................................85
SERVICING, PARTS, REPAIRS ......................................................................................................................................................................86
4.5 Orthotics ........................................................................................................................................................................................................ 87
Orthotic Devices Spinal ................................................................................................................................................................................88
Cervical ..............................................................................................................................................................................................................88
Cranial Remolding Orthosis ........................................................................................................................................................................88
Multiple Post Collar .......................................................................................................................................................................................89
Thoracic ............................................................................................................................................................................................................90
Thoracic-Lumbar-Sacral Orthosis (TLSO) ...............................................................................................................................................90
Cervical-Thoracic-Lumbar-Sacral Orthosis (CTLSO) ............................................................................................................................92
Lumbar Orthosis .............................................................................................................................................................................................93
Lumbar-Sacral Orthosis ...............................................................................................................................................................................93
Anterior-Posterior-Lateral Control ............................................................................................................................................................95

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
5
Halo Procedure ...............................................................................................................................................................................................96
Additions to Spinal Orthoses ......................................................................................................................................................................96
Orthotic Devices-Scoliosis Procedures ....................................................................................................................................................96
Cervical-Thoracic-Lumbar-Sacral Orthosis (CTLSO) ............................................................................................................................96
Thoracic-Lumbar-Sacral Orthosis (TLSO) (Low Profile) ...................................................................................................................... 97
Orthotic Devices-Lower Limb ..................................................................................................................................................................... 97
Fracture Orthoses ........................................................................................................................................................................................ 102
Orthotic Devices: Upper Limb .................................................................................................................................................................. 105
Shoulder-Elbow–Wrist–Hand Orthosis (SEWHO) Abduction Position: Custom Fitted ............................................................ 108
Repairs, Replacements and Maintenance to Existing Orthoses ..................................................................................................... 109
4.6 Prescription Footwear ...............................................................................................................................................................................110
Orthopedic Footwear ...................................................................................................................................................................................110
Diabetic Shoes, Fitting, and Modifications ............................................................................................................................................112
4.7 Prosthetics ....................................................................................................................................................................................................113
Lower Limb .................................................................................................................................................................................................... 114
Immediate Post-Surgical or Early Fitting Procedures .........................................................................................................................116
Upper Limb .................................................................................................................................................................................................... 124
Additions: Upper Limb ............................................................................................................................................................................... 126
Terminal Devices .......................................................................................................................................................................................... 127
External Power .............................................................................................................................................................................................. 128
Myoelectric .................................................................................................................................................................................................... 129
Breast And Hair Prosthesis .........................................................................................................................................................................131
Lower Extremity Compression Supports ................................................................................................................................................131
Trusses ............................................................................................................................................................................................................. 133
Burn Garments .............................................................................................................................................................................................. 133
Definitions .......................................................................................................................................................................................................... 134
Appendix A ........................................................................................................................................................................................................ 141
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
6
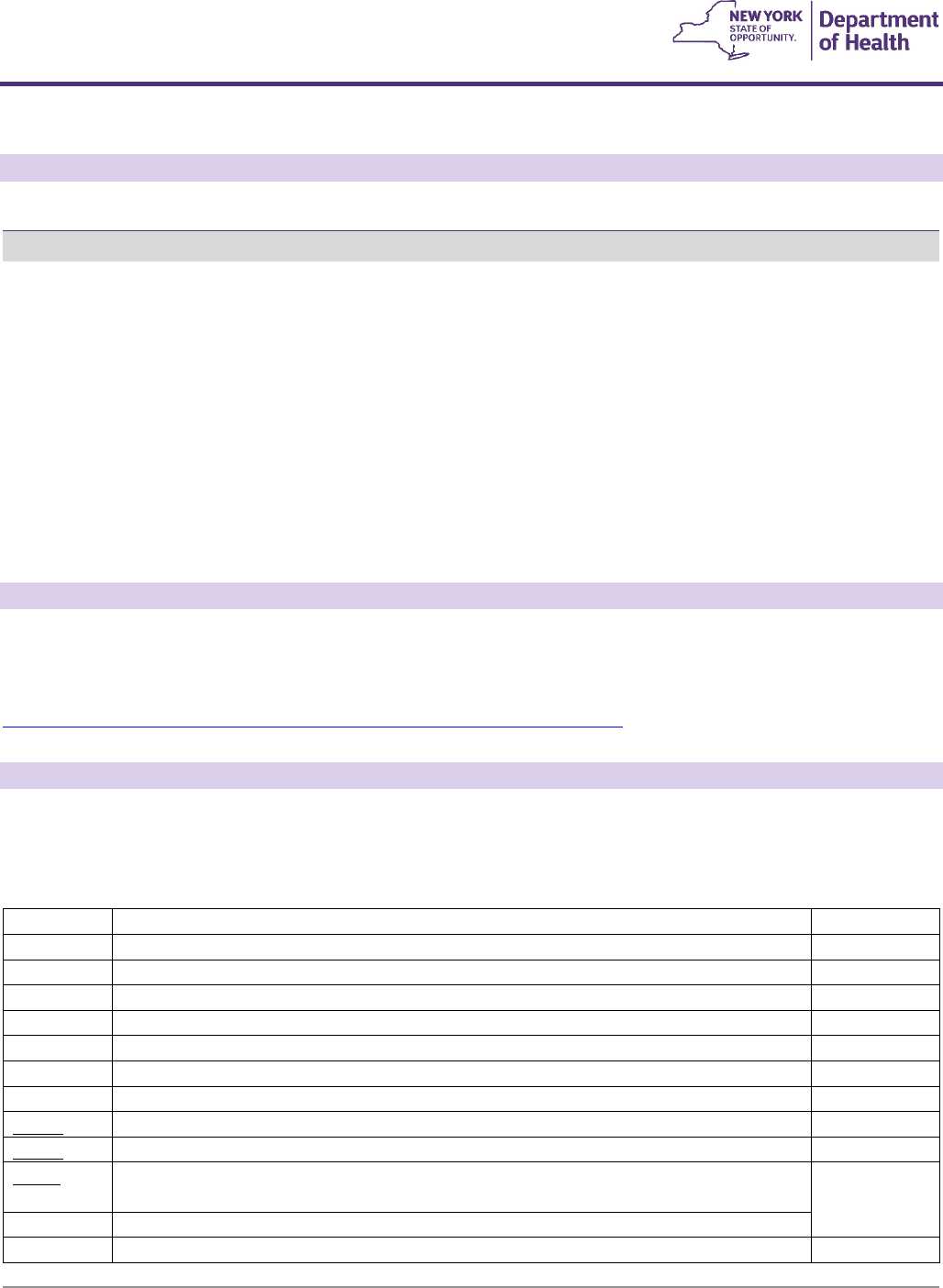
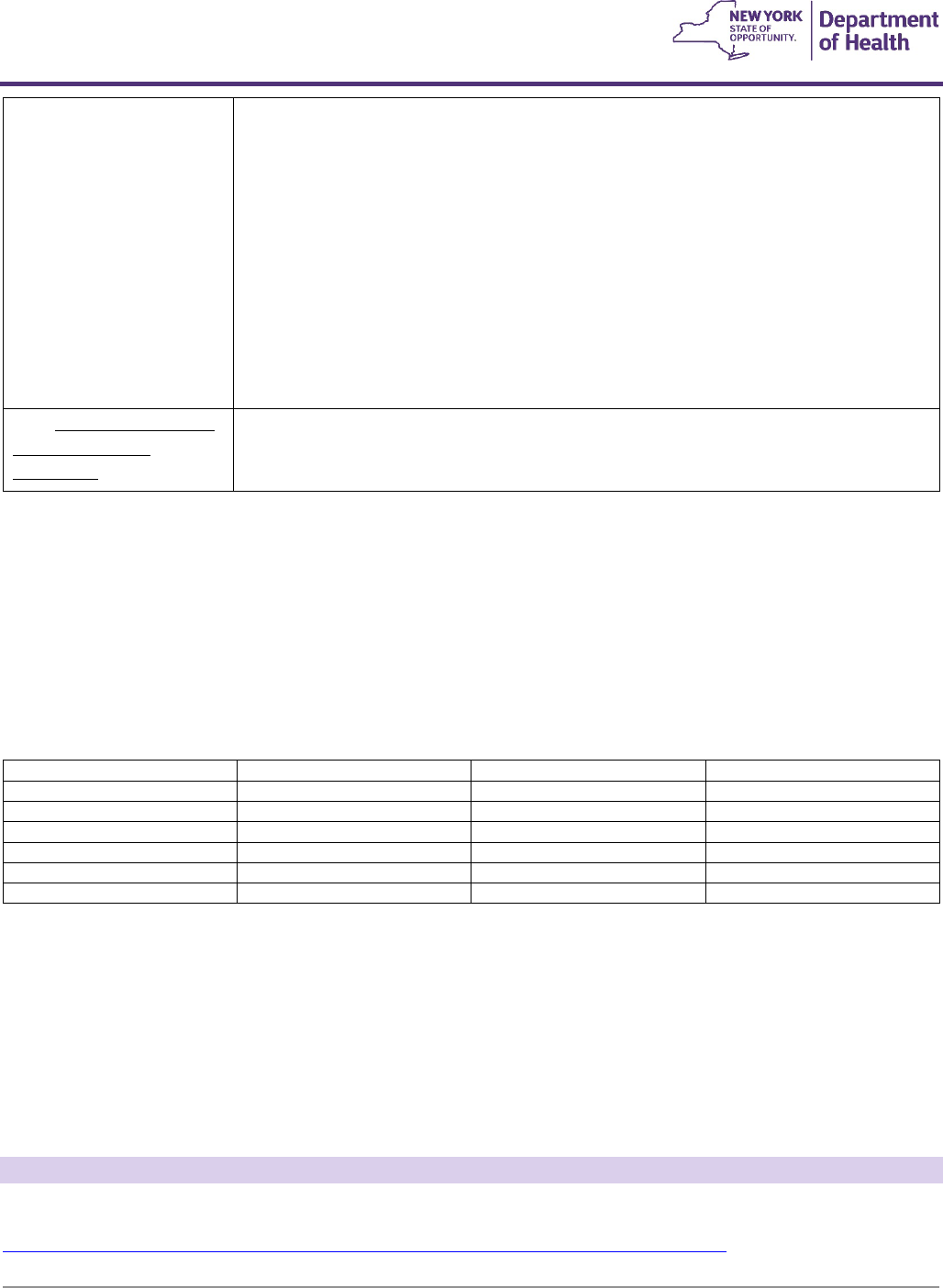
Document Control Properties
Control Item
Value
Document Name
Durable Medical Equipment, Prosthetics, and Orthotics Procedure
Codes and Coverage Guidelines
Document Control Number
DME 2024
Document Type
Coverage Guidelines
Document Version
1.0
Document Status
Published
Published
04/01/2024
DMEPOS Policy Manual
The DMEPOS policy manual can be found on eMedNY.org which includes definitions, requirements for participation in
Medicaid, and basis of payment for services provided.
https://www.emedny.org/ProviderManuals/DME/PDFS/DME_Policy_Section.pdf
3.0 NEW FOR 2024
Procedure Codes
Please note the following changes to the Procedure Codes section of the Durable Medical Equipment, Prosthetics,
Orthotics and Supplies manual.
New Code
Description
Fee
A6552
F7
#Gradient compression stocking, below knee, 30-40 mmhg, each
$43.85
A6553
F7
#Gradient compression stocking, below knee, 30-40 mmhg, custom, each
$171.21
A6554
F7
#Gradient compression stocking, below knee, 40 mmhg or greater, each
$60.29
A6555
F7
#Gradient compression stocking, below knee, 40 mmhg or greater, custom, each
$171.21
A6556
F7
#Gradient compression stocking, thigh length, 18-30 mmhg, custom, each
$234.63
A6557
F7
#Gradient compression stocking, thigh length, 30-40 mmhg, custom, each
$234.63
A6558
F7
#Gradient compression stocking, thigh length, 40 mmhg or greater, custom, each
$242.14
A6559
F7
Gradient compression stocking, full length/chap style, 18-30 mmhg, custom, each
Cost+51%
A6560
F7
Gradient compression stocking, full length/chap style, 30-40 mmhg, custom, each
Cost +51%
A6561
F7
Gradient compression stocking, full length/chap style, 40 mmhg or greater, custom,
each
Cost+51%
A6562
F7
#Gradient compression stocking, waist length, 18-30 mmhg, custom, each
$767.90
A6563
F7
#Gradient compression stocking, waist length, 30-40 mmhg, custom, each
$767.90
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
7
A6564
F7
#Gradient compression stocking, waist length, 40 mmhg or greater, custom, each
$827.20
A6565
F7
#Gradient compression gauntlet, custom, each
$132.69
A6568
F7
#Gradient compression garment, torso and shoulder, each
$125.74
A6569
F7
#Gradient compression garment, torso/shoulder, custom, each
$716.00
A6572
F7
#Gradient compression garment, toe caps, each
$79.50
A6573
F7
#Gradient compression garment, toe caps, custom, each
$188.64
A6574
F7
#Gradient compression arm sleeve and glove combination, custom, each
$240.05
A6575
F7
#Gradient compression arm sleeve and glove combination, each
$77.94
A6576
F7
#Gradient compression arm sleeve, custom, medium weight, each
$147.60
A6577
F7
#Gradient compression arm sleeve, custom, heavy weight, each
$122.16
A6578
F7
#Gradient compression arm sleeve, each
$58.00
A6579
F7
#Gradient compression glove, custom, medium weight, each
$236.91
A6580
F7
#Gradient compression glove, custom, heavy weight, each
$235.17
A6581
F7
#Gradient compression glove, each
$55.20
A6582
F7
#Gradient compression gauntlet, each
$36.82
A6583
F7
#Gradient compression wrap with adjustable straps, below knee, 30-50 mmhg, each
$121.10
A6584
F7
Gradient compression wrap with adjustable straps, not otherwise specified
Cost +51%
A6585
F7
#Gradient pressure wrap with adjustable straps, above knee, each
$143.39
A6586
F7
#Gradient pressure wrap with adjustable straps, full leg, each
$422.45
A6587
F7
#Gradient pressure wrap with adjustable straps, foot, each
$55.34
A6588
F7
#Gradient pressure wrap with adjustable straps, arm, each
$184.43
A6610
F7
#Gradient compression stocking, below knee, 18-30 mmhg, custom, each
$171.21
E0651
F2
Pneumatic compressor, segmental home model without calibrated gradient pressure
$830.53
E0652
F2
Pneumatic compressor, segmental home model with calibrated gradient pressure
$3,807.53
E0656
F3
#Segmental pneumatic appliance for use with pneumatic compressor, trunk
$614.80
E0657
F3
#Segmental pneumatic appliance for use with pneumatic compressor, chest
$577.52
E0667
F3
#Segmental pneumatic appliance for use with pneumatic compressor, full leg
$344.46
E0668
F3
#Segmental pneumatic appliance for use with pneumatic compressor, full arm
$399.59
E0669
F3
#Segmental pneumatic appliance for use with pneumatic compressor, half leg
$194.45
E0670
F3
#Segmental pneumatic appliance for use with pneumatic compressor, integrated, two
full legs and trunk
$1,337.38
E0671
F3
#Segmental gradient pressure pneumatic appliance, full leg
$441.90
E0672
F3
#Segmental gradient pressure pneumatic appliance, full arm
$343.34
E0673
F3
#Segmental gradient pressure pneumatic appliance, half leg
$285.30
E2298
F3
Complex rehabilitative power wheelchair accessory, power seat elevation system, any
type
$1600.27
L5615
F4
Addition, endoskeletal knee-shin system, 4 bar linkage or multiaxial, fluid swing and
stance phase control
$5,770.75
L5926
F4
#Addition to lower extremity prosthesis, endoskeletal, knee disarticulation, above
knee, hip disarticulation, positional rotation unit, any type
$534.18
Deleted/Replacement Codes
Please note the following codes that have been deleted and replaced
Deleted Code
Code Description
Replacement Code
Fee
E2300
F3
Wheelchair accessory, power seat elevator system, any type
E2298
F3
$1,600.27
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
8
K1022
F4
#Addition to lower extremity prosthesis, endoskeletal, knee
disarticulation, above knee, hip disarticulation, positional
rotation unit, any type
L5926
F4
#
Please note replacement
code requires DVS auth
$534.18
S8421
F21
#Gradient pressure aid (sleeve and glove combination),
ready made
See new prefabricated
codes for upper
extremity compression
garments (above)
S8424
F21
#Gradient pressure aid (sleeve), ready made
See new prefabricated
codes for upper
extremity compression
garments (above)
S8427
F21
#Gradient pressure aid (glove), ready made
See new prefabricated
codes for upper
extremity compression
garments (above)
S8428
F21
#Gradient pressure aid (gauntlet), ready made
See new prefabricated
codes for upper
extremity compression
garments (above)
Criteria/Guidelines
Please note the following changes to the Criteria/Guidelines section of the Durable Medical Equipment, Prosthetics,
Orthotics and Supplies manual.
Code or Category
Code and/or Description
Page
Pneumatic Compression Device
E0650-E0673
68
Breast Prosthesis custom
L8035
131
Power Seat Elevation
E2300(deleted)/E2298 (see first two bullets)
53
Frequency
Please note the following changes to the frequency listed on the Durable Medical Equipment, Prosthetics, Orthotics
and Supplies Fee Schedule.
Code
Previous Frequency
New Frequency
L8035
4 times/year
1 time/year
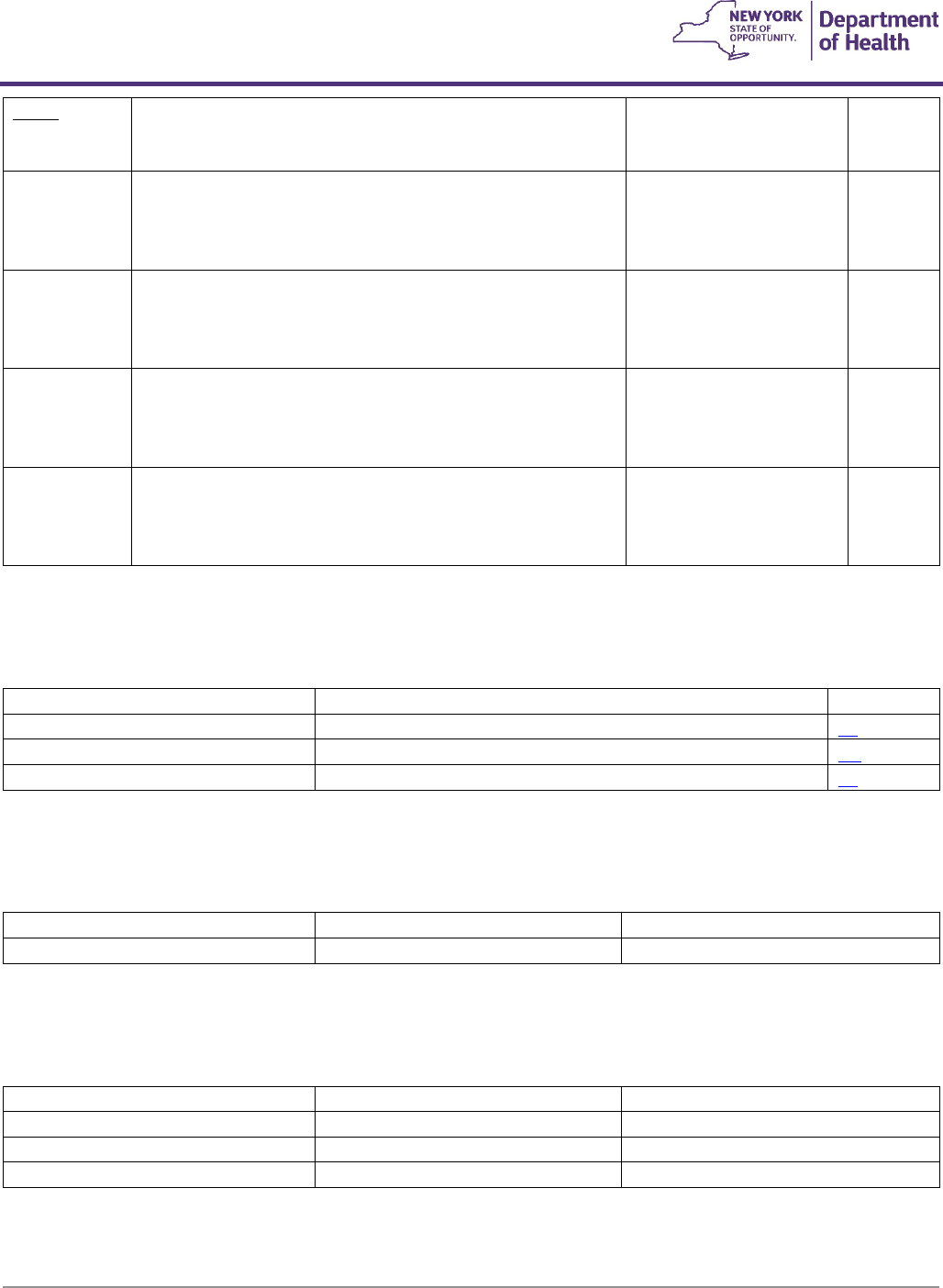
Fees
Please note the following changes to the fees listed on the Durable Medical Equipment, Prosthetics, Orthotics and
Supplies Fee Schedule.
Code/Description
Previous Fee
New Fee
L5781
$3726.78
Cost+51%
L5782
$3912.02
Cost+51%
L8035
$182.44
$3,287.02
Change in Authorization Type
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
9
Code
Previous Auth Type
New Auth Type
L8035
DVS Required (#)
Prior Approval Required (L8035)
4.0 General Information and Instructions
Fees
Fees are published in the Fee Schedule section of the DME Manual located at
https://www.emedny.org/ProviderManuals/DME/index.aspx
.
Standards
Standards of coverage are included for high utilization items to clarify conditions under which Medicaid will reimburse
for these items. Also see section 2 of the DME Policy Guidelines
.
Federal Law
Any item dispensed in violation of Federal, State or Local Law is not reimbursable by New York State Medicaid.
Purchases
An underlined procedure code indicates the item/service requires prior approval. When the procedure code’s
description is preceded by a “#”, the item/service requires an authorization via the dispensing validation system (DVS).
When the procedure code's description is preceded by an asterisk (*), the item/service requires an authorization via the
Interactive Voice Response (IVR) system. When none of the above-described circumstances exist, the procedure code is
a direct bill item. Please refer to the DME manual, Policy Guidelines, for additional information.
Brand Names
Where brand names and model numbers appear in the DME manual, they are intended to identify the type and quality
of equipment expected and are not exclusive of any comparable product by the same or another manufacturer.
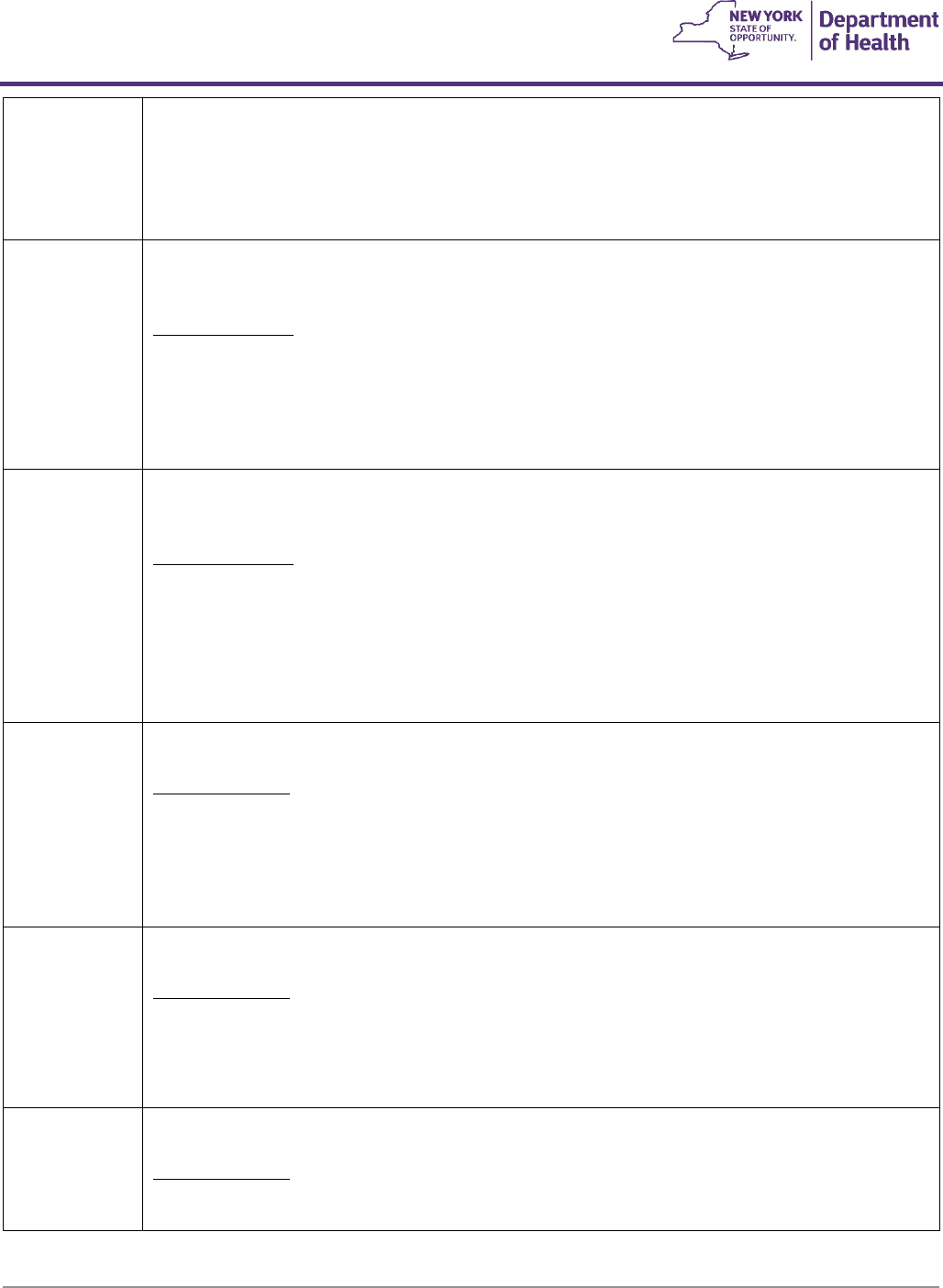
Modifiers
The following modifiers should be added to the five-character Healthcare Common Procedure Coding System (HCPCS)
code when appropriate.
‘-K0’ through ‘-K4’
modifiers, used to
describe
functional
classification levels of
ambulation
Must be used for all lower extremity prosthetic procedure codes. The modifier relates
to the specific functional classification level of the member. A description of the
functional classification levels can be found in
section 4.7 of this manual
‘-LT’ Left side and ‘-RT’
Right side
modifiers
Must be used when the orthotic, prescription footwear or prosthetic device is side-
specific. Do not use these modifiers with procedure codes for devices which are not
side-specific or when the code description is a pair. LT and/or RT should also be used
when submitted for replacement or repair of an item using the ‘-RB’ modifier
‘-RB' Replacement and
Repair
- Allowed twice per year (365 days) per device for patient-owned devices only.
More frequent repairs to the device require prior approval.
- Bill with the most specific code available with the modifier for the equipment
or part being repaired.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
10
- Use of “-RB” is not needed when a code is available for a specific replacement
part: use the specific code only when billing.
- A price must be listed for the code in the fee schedule in order for ‘-RB’ to be
reimbursable without prior approval.
- ‘-RB’ is not to be billed in combination with A9900, L4210 or L7510 for repair or
replacement of the same device.
- Indicates replacement and repair of
Orthotic and Prosthetic Devices
which
have been in use for some time.
Prior approval is not required when the charge is over $35.00 and is less
than 25% of the price listed on the code for the device.
For charges $35.00 and under use L4210 or L7510.
- Indicates replacement and repair of
Durable Medical Equipment
which has
been in use for some time and is outside of warranty.
Prior approval is not required when the repair charge is less than 25% of
the price listed on the code for the device.
If the charge is greater than 25% of the price, prior approval is required.
If no code is available (i.e. unlisted equipment) to adequately describe the
repair or replacement of the equipment or part, use A9900 and report
K0739 for labor component.
When repair and replacement is performed by a manufacturer, the
Medicaid provider will be paid the line-item labor cost on the
manufacturer’s invoice and the applicable Medicaid fee on the parts. If
labor and parts charges are not separately itemized on the invoice as
required by 18NYCRR 505.5, the Medicaid provider is not entitled to a
markup on the cost of parts and will only be paid the manufacturer
invoice cost of parts and labor.
‘-RR’ Rental
- Use the ‘-RR’ modifier when DME is to be rented.
- Rentals require DVS authorization for each month of rental. All DVS
authorization requests must include the ‘-RR’ modifier, including continuous
rentals.
- Prior Approval is required for rental only when no rental fee is listed in the
DME Fee Schedule or the items HCPCS code in this manual is underlined.
- Refer to the DME Fee Schedule for rental fees.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
11
- Rental is available up to maximum of 10 months. Monthly rental fee is
calculated at 10% of purchase price, with the exception of continuous rentals
(frequency listed as F26 in the Procedure Code section).
- The Length of Need must be specified by the ordering practitioner on the
fiscal order. If the order specifies a Length of Need of less than 10 months, the
equipment must be rented initially. If Length of Need is 10 months or greater,
the equipment may be initially rented or purchased.
- All rental payments must be deducted from the purchase price, with the
exception of continuous rentals. Utilization Review (UR) claims editing limits
the sum of all rental payments to the code’s purchase price.
‘-U3’ Repair/Replacement
of Patient Owned
Equipment
- Is required when billing for repairs to patient owned equipment when the
member is in a hospital or skilled nursing facility.
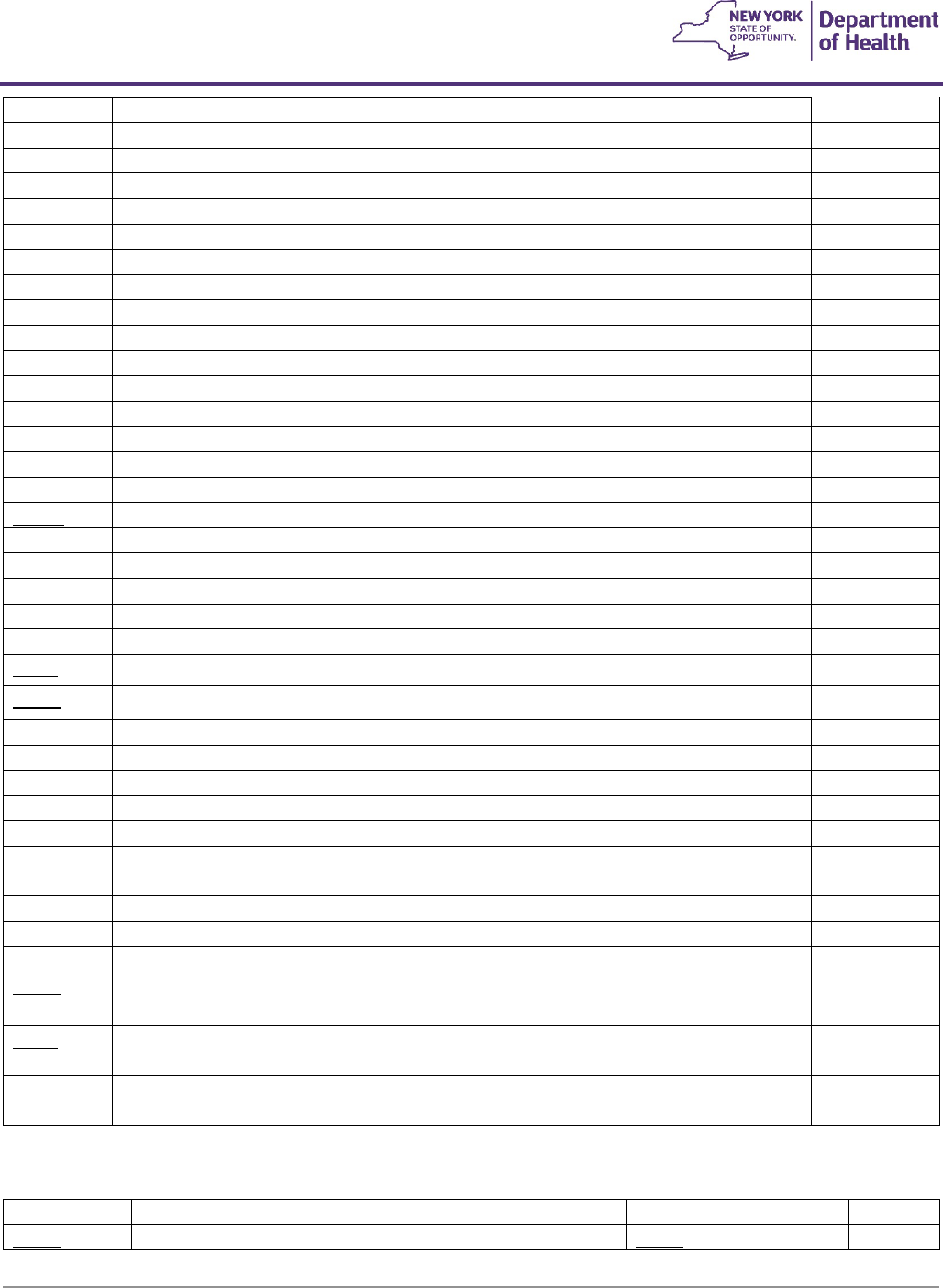
Quantity
The max units listed on the DME Fee Schedule is the maximum allowed according to the frequency limitations set for
that code (see below). If the fiscal order exceeds this amount, the provider must obtain prior approval.
Frequency
Durable Medical Equipment, Orthotics, Prosthetics and Supplies have limits on the frequency that items can be
dispensed to an eligible member. If a member exceeds the limit on an item, prior approval must be requested with
accompanying medical documentation as to why the limit needs to be exceeded. The frequency for each item is listed
by a superscript notation next to the procedure code. The following table lists the meaning of each notation:
F1=once/lifetime
F2-twice/lifetime
F3=once/5years
F4=once/3 years
F5=once/2 years
F6=once/year
F7=twice/year
F8=three/2 months
F9=once/month
F10=twice/month
F11=four/month
F12=once/day
F13=once/3 months
F14=four/lifetime
F15=six/lifetime
F16=once/6 months
F17=twelve/lifetime
F18=three/lifetime
F19=twice/3years
F20=two/2 years
F21=two/6 months
F22=four/year
F23=six/2 years
F24=eight/year
F25=eight/lifetime
F26=continuous monthly rental
Dispensing
This manual specifies when accessories or components are included in the maximum reimbursement amount (MRA) of
certain base codes (i.e., wheelchairs, standers, speech generating devices). These accessories or components should be
included at the time of initial dispensing of the equipment. No additional reimbursement will be made for these
accessories or components within 90 days of dispensing the base item. If an included accessory is required within 90
days of dispensing the original item, the equipment provider should supply the accessory or component at no
additional charge to the member.
4.1, 4.2, 4.3 Medical Supplies, Enteral Therapy, Hearing Aid Battery
Please see separate Medical Supply Procedure Code manual:
https://www.emedny.org/ProviderManuals/DME/PDFS/MedicalSupply_Procedure_Codes.pdf

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
12
4.4 Durable Medical Equipment
Hospital Beds and Accessories
General Guidelines:
- A hospital bed is covered if the member is bed-confined (not necessarily 100 percent of the time) and the
member's condition necessitates positioning of the body in a way not feasible in an ordinary bed, or
attachments are required which cannot be used on an ordinary bed.
- Hospital beds must be Durable Medical Equipment (DME) and used in the home.
- The manufacturer of a hospital bed must be registered with the United States Food and Drug
Administration (FDA).
- The hospital bed itself must be listed or cleared to market by the FDA.
- In no instance will an ordinary bed be covered by the Medicaid Program. An ordinary bed is one which is
typically sold as furniture and does not meet the definition of DME or a hospital bed.
- A hospital bed as defined must include bed ends with casters, IV sockets, side rails (any type) and can
accommodate/support a trapeze bar, overhead frame and/or other accessories.
- Side rail pads and shields (E1399) are covered when there is a documented need to reduce the risk of
entrapment or injury.
- If a member's condition requires a replacement innerspring mattress (E0271), foam rubber mattress (E0272)
and/or side rails (E0305 or E0310); it will be covered for a member owned hospital bed.
- When the extent and duration of the medical need is not known at the time of ordering, hospital beds and
related accessories should be rented.
E0251
F3
‘-RR’
#Hospital bed, fixed height, with any type side rails, without mattress
A standard hospital bed is one with manual head and leg elevation adjustments but no height
adjustment, which conforms to accepted industry standards, consisting of a modified latch spring
assembly, bed ends with casters, two manually operated foot end cranks, is equipped with IV
sockets, and can accommodate/support a trapeze bar, side rails (any type), an overhead frame and
other accessories.
Coverage Criteria:
A fixed height hospital bed (E0251) is covered if one or more of the following criteria (1-4) are met:
1. The member has a medical condition which requires positioning of the body in ways
not feasible with an ordinary bed. Elevation of the head/upper body less than 30
degrees does not usually require the use of a hospital bed; or
2. The member requires positioning of the body in ways not feasible with an ordinary bed
in order to alleviate pain; or
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
13
3. The member requires the head of the bed to be elevated more than 30 degrees most of
the time due to congestive heart failure, chronic pulmonary disease, or problems with
aspiration. Pillows or wedges must have been considered and ruled out; or
4. The member requires traction equipment, which can only be attached to a hospital bed.
E0256
F3
‘-RR’
#Hospital bed, variable height, hi-lo, with any type side rails, without mattress
A variable height hospital bed is one with manual height adjustment and with manual head and
leg elevation adjustments.
Coverage Criteria:
A variable height hospital bed (E0256) is covered if the member meets one of the criteria 1-4
above and:
5. The member requires a bed height different than a fixed height hospital bed to permit
transfers to chair, wheelchair or standing position.
E0261
F3
‘-RR’
#Hospital bed, semi-electric (head and foot adjustment) with any type side rails, without mattress
A semi-electric hospital bed is one with manual height adjustment and with electric head and leg
elevation adjustments.
Coverage Criteria:
A semi-electric hospital bed (E0261) is covered if the member meets one of the criteria 1-4 above
and:
6. The member requires frequent changes in body position and/or has an immediate need
for a change in body position (i.e., no delay in change can be tolerated) and the
member can independently affect the adjustment by operating the controls.
E0266
F3
‘-RR’
#Hospital bed, total electric (head, foot and height adjustments), with any type side rails, without
mattress
Coverage Criteria:
A total electric hospital bed (E0266) is covered if the member meets one of the criteria 1-4 and
both criteria 5 and 6 above, and:
7. The member can adjust the bed height by operating the controls to effect independent
transfers.
E0301
F3
‘-RR’
#Hospital bed, heavy duty, extra wide, with weight capacity greater than 350 pounds, but less than
or equal to 600 pounds, with any type side rails, without mattress (up to 48” width)
Coverage Criteria:
A heavy duty extra wide (E0301) hospital bed is covered if the member meets one of the criteria 1-
4 above and:
8. The member's weight is more than 350 pounds but does not exceed 600 pounds.
E0302
F2
‘-RR’
#Hospital bed, extra heavy duty, extra wide, with weight capacity greater than 600 pounds, with
any type side rails, without mattress
Coverage Criteria:
An extra heavy-duty hospital bed (E0302) is covered if the member meets one of the criteria 1-4
above and:
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
14
9. The member's weight exceeds 600 pounds.
E0328
F3
‘-RR’
#Hospital bed, pediatric, manual, 360 degree side enclosures, top of headboard, footboard and
side rails up to 24 inches above the spring, includes mattress
(prior approval required for ages less
than 3 or over 20. Includes manual articulation and manual height adjustment)
Coverage Criteria:
A Pediatric hospital bed is covered when the member meets one of the criteria 1-4 above and:
10. The patient has a diagnosis-related cognitive or communication impairment or a severe
behavioral disorder that results in risk for safety in bed; and
11. There is evidence of mobility that puts the patient at risk for injury while in bed (more
than standing at the side of the bed), or the patient has had an injury relating to bed
mobility; and
12. Less costly alternatives have been tried and were unsuccessful or contraindicated (e.g.,
putting a mattress on the floor, padding added to ordinary beds or hospital beds,
transparent plastic shields, medications, helmets); and
13. The ordering practitioner has ruled out physical and environmental factors as reasons
for patient behavior, such as hunger, thirst, restlessness, pain, need to toilet, fatigue due
to sleep deprivation, acute physical illness, temperature, noise levels, lighting,
medication side effects, over- or under-stimulation, or a change in caregivers or routine.
Please note: For patients with a behavioral disorder, a behavioral management plan is required.
E0271
F5
‘-RR’
#Mattress, inner spring
E0272
F5
‘-RR’
#Mattress, foam rubber
E0274
F3
#Over-bed table
E0305
F5
#Bedside rails, half-length (telescoping per pair, replacement only)
E0310
F5
#Bedside rails, full-length (telescoping per pair, replacement only)
E0316
F3
‘-RR’
Safety enclosure frame/canopy for use with hospital bed, any type
Coverage Criteria:
A hospital bed safety enclosure frame/canopy is covered when criteria 10-15 are met, and 16 and
17, if applicable:
14. The member’s bed mobility results in risk for safety in bed that cannot be accommodated
by an enclosed pediatric manual hospital bed; and
15. A written monitoring plan approved by the ordering and all treating practitioners has
been completed which describes when the bed will be used, how the member will be
monitored at specified time intervals, how all of the member’s needs will be met while
using the enclosed bed (including eating, hydration, skin care, toileting, and general
safety), identification by relationship of all caregivers providing care to the member and
an explanation of how any medical conditions (e.g., seizures) will be managed while the
member is in the enclosed bed; and
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
15
16. In the absence of injury relating to bed mobility, a successful trial in the home or facility;
and
17. For members residing in an OMRDD certified residence, approval as a restraint with the
agency’s Human Rights Committee.
Pressure Reducing Support Surfaces
General Guidelines:
- Covered benefit when a member is bedridden or wheelchair-bound and/or has a documented history of
decubitus where conventional cushioning methods have failed.
- Air fluidized beds are not covered for the home setting.
- Medicaid reimbursement for pressure reducing support surfaces is based on the following coding assignments
and coverage criteria.
For Group 1 surfaces (codes A4640, E0181, E0182, E0184, E0185, E0186, E0187, E0188, E0196, E0197, E0198, E0199 {see
Section 4.1 for E0188}):
- Completely immobile, i.e. member cannot make changes in body position, or
- Limited mobility, i.e. member cannot independently make changes in body position significant enough to
alleviate pressure and
- Has any stage pressure ulcer on the trunk or pelvis and
- One or more of the following:
1. Impaired nutritional status
2. Fecal or urinary incontinence
3. Altered sensory perception
4. Compromised circulatory status
For Group 2 surfaces (codes E0193, E0277, E0371, E0372):
- Multiple Stage II pressure ulcers located on trunk or pelvis and the member has been on a comprehensive
ulcer treatment program for at least the past month which has included the use of an appropriate Group 1
support surface and the ulcers have worsened or remained the same over the past month or
- Large or multiple Stage III or IV pressure ulcers on the trunk or pelvis or
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
16
- Recent myocutaneous flap or skin graft surgery (past 60 days) for a pressure ulcer on the trunk or pelvis and
the member has been on at least a Group 2 support surface immediately prior to a recent discharge (past 30
days) from a hospital or nursing home.
A4640
F6
#Replacement pad for use with medically necessary alternating pressure pad owned by patient
E0181
F3
#Powered pressure reducing mattress overlay/pad, alternating, with pump, includes heavy duty
E0182
F3
#Pump for alternating pressure pad, for replacement only
E0184
F6
‘-RR’
#Dry pressure mattress
E0185
F6
#Gel or gel-like pressure pad for mattress, standard mattress length and width
E0186
F6
‘-RR’
#Air pressure mattress
E0187
F6
‘-RR’
#Water pressure mattress
E0190
F5
#Positioning cushion/pillow/wedge, any shape or size, includes all components and accessories
E0193
F2
‘-RR-‘
#Powered air flotation bed (low air loss therapy)
E0196
F6
‘-RR’
#Gel pressure mattress
E0197
F6
#Air pressure pad for mattress, standard mattress length and width
E0198
F6
#Water pressure pad for mattress, standard mattress length and width
E0199
F6
#Dry pressure pad for mattress, standard mattress length and width
E0277
F2
‘-RR-‘
#Power pressure reducing air mattress
E0371
F2
‘-RR’
#Non-powered advance pressure reducing overlay for mattress, standard mattress length and
width
E0372
F2
‘-RR’
#Powered air overlay for mattress, standard mattress length and width
IPPB Machines
A4618
F11
Breathing Circuits
E0500
F6
IPPB machine, all types, with built-in nebulization; manual or automatic valves; internal or external
power source
Intermittent Positive Pressure Breathing Machines are covered if the member's ability to breathe
is severely impaired and medical necessity is supported by diagnosis. The level of sophistication
of the machine should be compatible with the member's need and be appropriate for home use.
Oxygen Systems
Coverage Guidelines:
- Oxygen therapy is covered by the New York State Medicaid Program under the following conditions:

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
17
1. The oxygen therapy must be an integral component of a documented medical treatment plan and ordered in
writing by an authorized practitioner.
2. The practitioner has determined that the member suffers from a severe lung disease or hypoxia-related
symptoms that might be expected to improve with oxygen therapy, the member's blood gas levels indicate
the need for oxygen therapy, the alternative treatment measures have been tried or considered and been
deemed clinically ineffective.
3. Coverage is provided for members with significant hypoxia evidenced by any of the following blood gas
levels/oxygen saturation levels:
a. An arterial PO2 at or below 55 mm Hg or an oxygen saturation at or below 88 percent taken at rest
(awake), or
b. An arterial PO2 at or below 55 mm Hg, or an oxygen saturation at or below 88 percent, for at least 5
minutes taken during sleep for a patient who demonstrates an arterial PO2 at or above 56 mm Hg or
an oxygen saturation at or above 89% while awake, or
c. A decrease in arterial PO2 more than 10 mm Hg, or a decrease in oxygen saturation more than 5
percent, for at least 5 minutes taken during sleep associated with symptoms or signs reasonable
attributable to hypoxemia (e.g., cor pulmonale, “P” pulmonale or EKG, documented pulmonary
hypertension and erythrocytosis), or
d. An arterial PO2 at or below 55 mm Hg or an oxygen saturation at or below 88 percent, taken during
exercise for a patient who demonstrates an arterial PO2 at or above 56 mm Hg or an oxygen
saturation at or above 89 percent during the day while at rest. (In this case, oxygen is provided for
during exercise if it is documented that the use of oxygen improves the hypoxemia that was
demonstrated during exercise when the patient was breathing room air).
4. Coverage is available for PO2 56 to 59 mm Hg or oxygen saturation is 89% if any of the following are documented:
a. Dependent edema suggesting congestive heart failure; or
b. Pulmonary hypertension or cor pulmonale, determined by measurement of pulmonary artery
pressure, gated blood pool scan, echocardiogram, or "P" pulmonale of EKG (P wave greater than 3mm
in Standard Leads II, III, or AVF); or
c. Erythrocythemia with a hematocrit greater than 56%.
5. Liquid oxygen therapy coverage is limited to the following conditions:
a. Member requires constant (24 hours per day) liter flow greater than 5LPM; or
b. Member must be away from the home for long periods of time on a daily basis (e.g., school);
c. Members who qualify for coverage of liquid oxygen will not receive coverage for any other delivery
system during the same time period.
- Oxygen and related supplies are covered when prescribed for home oxygen therapy to treat a demonstrated
severe breathing impairment. For many high-volume oxygen users an oxygen concentrator represents a less
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
18
expensive, medically appropriate alternative to containerized oxygen, quantity consumed should be a
consideration in the type of equipment dispensed.
- Portable oxygen systems are covered when the practitioner's order specifies that the portable system is
medically necessary.
- E0431 and E0434 may not be billed in combination.
- The DMEPOS provider must maintain the practitioner's documentation of medical necessity on file with the
written order.
- Oxygen therapy must be re-ordered once every 365 days or more frequently if the member's need for oxygen
changes, as well as all medical documentation to substantiate coverage criteria.
- All home oxygen therapy services are reimbursed on an all-inclusive rate that may be billed once per 30 days.
- A “spot check” pulse oximeter for intermittently checking oxygen levels is included in the monthly rental
reimbursement for all oxygen systems.
- As with all rentals the 30-day fee includes all necessary equipment (e.g. oxygen tank holder).
E0424
F26
#Stationary compressed gaseous oxygen system, rental; includes container, contents, regulator,
flowmeter, humidifier, nebulizer, cannula or mask and tubing
E0431
F26
#Portable gaseous oxygen system, rental; includes portable container, regulator, flowmeter,
humidifier, cannula or mask, and tubing (includes contents)
E0434
F26
#Portable liquid oxygen systems, rental; includes portable container, supply reservoir, humidifier,
flowmeter, refill adaptor, contents gauge, cannula or mask, and tubing
E0439
F26
#Stationary liquid oxygen system, rental; includes container, contents, regulator, flowmeter,
humidifier, nebulizer, cannula or mask, and tubing (per unit) (one unit= one liter per minute) (up
to six units)
E1390
F26
#Oxygen concentrator, single delivery port, capable of delivering 85 percent or greater oxygen
concentration at prescribed flow rate
The 30-day rate for code E1390 includes portable/emergency gaseous supply. This supply would
be in place for a power outage, malfunction of the concentrator, etc. for the homebound
member, and is included in the 30-day rate. However
,
portable oxygen can be billed in addition
to the concentrator when the member requires portable oxygen (E0431) to go out of the house
for normal (non-emergency) activities such as appointments or grocery shopping, etc.
E1392
F26
#Portable oxygen concentrator, rental
- The 30-day rate includes all oxygen needs: stationary, portable, and emergency
gaseous supply in place for a power outage, malfunction of the concentrator, or other
emergency situations.
- Code E1392 is not reimbursable in conjunction with any other oxygen system (codes
E1390, E0424, E0431, E0434 or E0439).
Respiratory Care
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
19
A7027
F7
#Combination oral/nasal mask, used with continuous positive airway pressure device, each
A7028
F7
#Oral cushion for combination oral/nasal mask, replacement only, each
A7029
F7
#Nasal pillows for combination oral/nasal mask, replacement only, pair
A7030
F6
#Full face mask used with positive airway pressure device, each
A7031
F7
#Face mask interface, replacement for full face mask, each
A7032
F7
#Cushion for use on nasal mask interface, replacement only, each
A7033
F7
#Pillow for use on nasal cannula type interface, replacement only, pair
A7034
F6
#Nasal interface (mask or cannula type) used with positive airway pressure device, with or without
head strap
A7035
F7
#Headgear used with positive airway pressure device
A7036
F7
#Chinstrap used with positive airway pressure device
A7037
F7
#Tubing used with positive airway pressure device
A7044
F6
#Oral interface used with positive airway pressure device, each
A7045
F7
#Exhalation port with or without swivel used with accessories for positive airway devices,
replacement only
E0445
F3
‘-RR
’
Oximeter device for measuring blood oxygen levels non-invasively
General Guidelines
- A “spot check” pulse oximeter for intermittently checking oxygen levels is included in the
monthly rental reimbursement for all oxygen systems (E0424, E0431, E0434, E0439,
E1390, and E1392) and should not be billed separately.
- A “continuous” monitoring oximeter, required for more than spot-checking oxygen levels
(e.g., required for continuous monitoring, recording/trending, alarms), must be submitted
through prior approval.
- A “continuous” oximeter for short-term use less than 6 months is rented. The monthly
rental amount includes probes, cables, repair, and maintenance. If medical need for
“continuous” oximeter extends beyond the initial 6 months, submit through prior
approval for purchase. All rental fees must be deducted from purchase price.
- A “continuous” oximeter for long-term use, greater than 6 months is purchased. The
maximum reimbursement amount for the continuous oximeter includes all probes,
cables, and supplies necessary for use of the device.
- Once purchased, supplies require prior approval.
Coverage Criteria for “Continuous” Oximeter:
Covered in combination with oxygen therapy under the following circumstances:
- Weaning from oxygen.
- Changes in physical condition requiring adjustments in oxygen therapy.
- Maintaining oxygen levels within a narrow range.
- As part of a primary care provider’s or physician specialist’s treatment plan requiring
frequent monitoring/assessment of oxygen levels that cannot be achieved using a “Spot
check” oximeter.
Covered without oxygen therapy under the following circumstance:
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
20
- In cases of complex cardiac conditions, such as, but not limited to, univentricular heart or
unrepaired cyanotic heart disease.
Documentation Requirements for “Continuous” Oximeter
The following documentation is necessary to support prior approval of a “continuous” oximeter:
- Diagnosis/medical condition justifying the need to monitor blood oxygen levels.
- Current oxygen orders, if applicable (note: Medicaid guidelines require oxygen orders to
be renewed every 12 months).
- Treatment plan listing the required parameters and interventions for abnormal readings,
including corresponding oxygen titrations if applicable.
- Availability of caregivers trained to appropriately manage the listed treatment
interventions.
If used with a ventilator, CPAP, BiPAP, or other respiratory assist device, the type, make, and
model of the respiratory assist device must be provided to ensure oximetry is not already
available on that device.
A4606
F6
Oxygen probe for use with oximeter device, replacement
- Pulse oximeter probes are used with the “Continuous” Oximeter (E0445) and are included
in the reimbursement for the pulse oximeter rental or at initial issue of the device if
purchased.
- Prior approval for oxygen probes (A4606) is required when replacement is necessary for
member-owned equipment.
- Disposable pulse oximeter probes are limited to four per month.
- Reusable pulse oximeter probes are limited to one every twelve months.
- Submit fiscal order and invoice with prior approval request.
Ventilators
E0465, E0466, and BiPAP ST devices (E0471 and E0472) will:
- Only be rented and are not to be billed in combination, and
- As with all rentals, the 30-day fee includes all necessary equipment, delivery, maintenance and repair costs,
parts, supplies (e.g. tracheostoma filters, any type) and services for equipment set-up, maintenance and
replacement of worn essential accessories or parts, loading or downloading software, and back-up equipment
as needed.
General Guidelines:
Ventilators (E0465, E0466, and E0467) are covered for the following conditions as supported by documentation in the
member’s medical record:
- Neuromuscular disorder/disease
- Thoracic restrictive disorder/disease
- Chronic respiratory failure

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
21
The following information must be in the member’s medical record and available on request:
- The underlying medical condition requiring ventilator support.
- The need for the ventilator must be documented by the ordering medical professional. Frequency of use and
ventilator settings must be on the fiscal order.
Home ventilators are:
- Not covered when used to function as a CPAP (E0601) or bi-level PAP (E0470, E0471).
- If the ventilator is only intended for use in CPAP or BiPAP mode, the ordering provider is responsible to order
the appropriate equipment and the equipment provider is responsible to dispense the appropriate
equipment.
E0465
F26
#Home ventilator, any type, used with invasive interface, (e.g., tracheostomy tube)
E0466
F26
#Home ventilator, any type, used with non-invasive interface, (e.g., mask, chest shell)
E0467
F26
#Home ventilator, multi-function respiratory device, also performs any or all of the additional
functions of oxygen concentration, drug nebulization, aspiration, and cough stimulation, includes all
accessories, components and supplies for all functions
General Guidelines:
1. Only one ventilator code will be reimbursable per rental month.
2. It is the billing provider’s responsibility to maintain documentation that the member meets coverage criteria.
3. The following therapies/supplies/equipment are included in the functionality of code E0467 and will not be
separately reimbursable:
- Ventilators (HCPCS codes E0465, E0466)
- Oxygen and Oxygen Equipment
- Nebulizers and related accessories
- Aspirator and related accessories
- Cough Stimulator
- Mechanical Insufflation-Exsufflation devices and related accessories
- High Frequency Chest Wall Oscillation Devices and related accessories
- Oscillatory positive expiratory pressure device
4. As with all rentals, the 30-day fee includes all necessary equipment, delivery, maintenance and repair costs,
parts, supplies (e.g. tracheostoma filters, any type) and services for equipment set-up, maintenance and
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
22
replacement of worn essential accessories or parts, loading or downloading software, and back up equipment
as needed.
Coverage Criteria:
Members must meet the following criteria:
- Member is new to ventilator use, AND
- Member must require ventilator and one of the following covered therapies: cough stimulator, oxygen, suction
pump, nebulizer.
Positive Airway Pressure Devices (PAP)
Positive Airway Pressure (PAP) Devices are for the treatment of Obstructive Sleep Apnea. The term PAP (positive airway
pressure) devices refers to both a single-level continuous positive airway pressure device (E0601) and a bi-level
respiratory assist device without back-up rate (E0470) when it is used in the treatment of obstructive sleep apnea.
E0601
F3
‘-RR’
#Continuous positive airway pressure (CPAP) device
E0470
F3
‘-RR’
#Respiratory assist device, bi-level pressure capability without backup rate feature, used with
noninvasive interface, e.g., nasal or facial mask (intermittent assist device with continuous positive
airway pressure device)
Coverage Guidelines:
CPAP (E0601) is covered for treatment of Obstructive Sleep Apnea (OSA) if the following criteria are met:
- The patient must have a diagnosis of OSA documented by an attended, facility-based, as defined by Medicare
polysomnogram and meet the following criteria:
- The apnea-hypopnea index (AHI) or Respiratory Disturbance Index, (RDI) is greater than 15 events per hour
with a minimum of 30 events, or
- The AHI or RDI is greater than or equal to 5 and less than or equal to 14 events per hour with a minimum of 10
events and
- Documentation of:
a. Excessive daytime sleepiness, impaired cognition, mood disorders, or insomnia or,
b. Hypertension, ischemic heart disease, or history of stroke.
CPAP Replacement (E0601)
If a CPAP device is replaced prior to or following the 5-year useful life, there must be an in-person evaluation by the
treating practitioner that documents that the member continues to use and benefit from the CPAP device.
The following documentation must be submitted with the prior approval request:
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
23
- Face-to-face clinical reevaluation by the treating practitioner with documentation that symptoms of
obstructive sleep apnea have improved or stabilized; and
- Objective evidence of member compliance with use of the CPAP device, including but not limited to,
compliance graph printouts. Adherence to therapy is defined as use of CPAP four (4) or more hours per night
on at least 70% of nights during a consecutive thirty (30) day period anytime within the last 6 months of usage
prior to submitting for a replacement E0601 or E0470.
BIPAP (E0470) will be covered for members with a diagnosis of OSA who have failed a facility-based therapeutic trial of
a single level positive airway pressure device (CPAP).
Positive Airway Pressure (PAP) devices can either be purchased or rented as a 10-month capped rental. If the member
has a primary payor, the provider must submit an EOB from the primary payor according to Medicaid billing
guidelines.
RESPIRATORY ASSIST DEVICES
- BiPAP: E0470
- BiPAP ST: E0471 and E0472
A Respiratory Assist Device (RAD) is covered for those members with one of the following clinical disorders: restrictive
thoracic disorders (i.e., neuromuscular diseases or severe thoracic cage abnormalities), severe chronic obstructive
pulmonary disease (COPD), CSA or CompSA (Complex sleep apnea), or hypoventilation syndrome.
E0471
F26
#Respiratory assist device, bi-level pressure capability, with backup rate feature, used with noninvasive
interface, e.g., nasal or facial mask (intermittent assist device with continuous positive airway pressure
device) (BiPAP ST)
E0472
F26
#Respiratory assist device, bi-level pressure capability, with backup rate feature, used with invasive
interface, e.g., tracheostomy tube (intermittent assist device with continuous positive airway pressure
device) (BiPAP ST)
Airway Clearance Devices
E0480, E0481, E0482, E0483
Requests for Airway Clearance Devices must have the following information documented in the member’s medical
record and be available upon request:
- The underlying medical condition(s) causing the accumulation of pulmonary secretions and the specific
diagnosis supporting such equipment (e.g., neuromuscular disease(s); chronic pulmonary disease,
bronchiectasis, cystic fibrosis).
- The need for the requested equipment and the treatment plan, with frequency of use and settings included on
the fiscal order.
- The training given to the member or caregiver on the use of the equipment.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
24
E0480
F3
‘-RR’
#Percussor, electric or pneumatic, home model
E0481
F9
#Intrapulmonary percussive ventilation system and related accessories
Purchase price reached at 720 days (24 months)
E0482
F9
#Cough stimulating device, alternating positive and negative airway pressure (manual or
automatic)
Purchase price reached at 720 days (24 months)
E0483
F9
#High frequency chest wall oscillation air-pulse generator system, (includes hoses and vest), each
Purchase price reached at 720 days (24 months)
E0484
F6
#Oscillatory positive expiratory pressure device, non-electric, any type, each (one per year)
A7020
F9
Interface for cough stimulating device, includes all components, replacement only
A7025
F2
#High frequency chest wall oscillation system vest, replacement for use with patient owned
equipment, each
A7026
F2
#High frequency chest wall oscillation system hose, replacement for use with patient owned
equipment, each
A7046
F7
Water chamber for humidifier, used with positive airway pressure device, replacement, each
E0550
F3
‘-RR’
#Humidifier, durable for extensive supplemental humidification during IPPB treatments or oxygen
delivery
E0561
F3
‘-RR’
#Humidifier, non-heated, used with positive airway pressure device
E0562
F3
‘-RR’
#Humidifier, heated, used with positive airway pressure device
E0565
F3
‘-RR’
#Compressor, air power source for equipment which is not self-contained or cylinder driven
A compressor is covered only as an air power source for medically necessary durable medical
equipment that is not self-contained.
E0570
F6
#Nebulizer, with compressor
E0575
F3
#Nebulizer, ultrasonic, large volume
Ultrasonic nebulizers are covered where the presence of chronic obstructive pulmonary disease
necessitates the greatest possible degree of nebulization in order to affect a therapeutic response
E0580
F9
Nebulizer, durable, glass or autoclavable plastic, bottle type, for use with regulator or flowmeter
E0600
F3
Respiratory suction pump, home model, portable or stationary, electric
K0730
F9
#Controlled dose inhalation drug delivery system
- Covered with a diagnosis of pulmonary arterial hypertension with Class III or IV
symptoms, for administration of lloprost inhalation.
- The 30-day rate includes all supplies.
S8185
F6
#Flutter device (positive expiratory pressure device)
S8999
F3
Resuscitation bag (manual resuscitator for use by patient on artificial respiration during power
failure or other catastrophic event)
Traction Equipment, Various
Trapeze/traction equipment is covered if the member needs this device to sit up because of a respiratory condition, to
change body position for other medical reasons, or to get in or out of bed. Heavy duty trapeze equipment is covered if
the member meets the criteria for regular trapeze equipment and the member's weight is more than 250 pounds.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
25
E0849
F2
‘-RR’
#Traction equipment, cervical, free-standing stand/frame, pneumatic, applying traction force to
other than mandible
E0855
F2
‘-RR’
#Cervical traction equipment not requiring additional stand or frame
E0860
F3
Traction equipment, overdoor, cervical
E0890
F3
Traction frame, attached to footboard, pelvic traction
E0900
F3
Traction stand, free standing, pelvic traction (e.g., Buck's)
E0910
F3
‘-RR’
#Trapeze bars, also known as Patient Helper, attached to bed, with grab bar
E0911
F3
‘-RR’
#Trapeze bar, heavy duty, for patient weight capacity greater than 250 pounds, attached to bed,
with grab bar
E0912
F3
‘-RR’
#Trapeze bar, heavy duty, for patient weight capacity greater than 250 pounds, free standing,
complete with grab bar
E0940
F3
‘-RR’
#Trapeze bar, free standing, complete with grab bar
E0946
F3
‘-RR’
#Fracture, frame, dual with cross bars, attached to bed (e.g. Balken, Four Poster)
Walkers (Any Width)
E0130
F2
#Walker, rigid (pick-up), adjustable or fixed height
E0135
F2
#Walker, folding (pick-up), adjustable or fixed height
E0140
F3
Walker, with trunk support, adjustable or fixed height, any type
- Home walkers with trunk support provide complete adjustment to the center of gravity
and trunk angle; and support and stimulate walking movements for an adult who
requires gait training or retraining due to severe motor and balance dysfunction.
- Clinical documentation from a trial period must be submitted with the prior approval
request.
Coverage Criteria:
- The member is unable to stand or ambulate independently due to conditions such as,
but not limited to, neuromuscular or congenital disorders, including acquired skeletal
abnormalities.
- The alignment of the member’s lower extremities is such that they can tolerate a
standing or upright position.
- The member does not have orthostatic hypotension, postural tachycardia syndrome,
osteogenesis imperfecta, osteoporosis and other brittle bone diseases.
- The member has demonstrated improved mobility, function and physiologic symptoms
or has maintained status with the use of the requested walker with trunk support (when
other alternatives have failed) and is able to follow a home ambulation program
incorporating the use of the walker with trunk support (as documented by a clinical
ambulation program or a home trial with the requested walker).
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
26
- There is a home therapy plan outlining the use of the requested walker with trunk
support.
- The member does not require a home standing device in addition to a walker or gait
trainer. Provision of both a standing device and walker/gait trainer is typically considered
a duplication of service, as both address weight bearing.
Documentation requirements:
- A prescription including the walker and any modifications/accessories requested.
- A detailed letter of medical necessity (LMN) that includes:
1. A comprehensive history and physical exam by a licensed physician, physical therapist,
or occupational therapist.
2. A summary of the existing medical condition, age at diagnosis, prognosis, and co-
morbid conditions.
3. The member’s functional and physical assessment including strength, range of motion,
tone, sensation, balance, ADLs, and functional status.
4. Documentation of failure of less costly alternatives (include make and model of
alternatives tried as well as the length of the trial with each alternative).
5. A home therapy plan outlining the planned use of the requested walker with trunk
support.
6. Documentation that the member does not have sufficient access to equipment in an
alternative setting, e.g. clinic, outpatient therapy, etc.
7. Documentation regarding the level of caregiver assistance available and/or needed on
daily basis.
8. Documentation that the member’s home can accommodate the requested walker with
trunk support and that the family/caregiver has been trained in the use and
maintenance of the requested walker.
E0141
F2
#Walker, rigid, wheeled, adjustable or fixed height
E0143
F4
#Walker, folding, wheeled, adjustable or fixed height
E0144
F3
#Walker, enclosed, four sided framed, rigid or folding, wheeled with posterior seat
- Provides safety and promotes unassisted walking.
- May include brake and/or variable resistance wheels.
- For an adult or child who requires enclosure and seat due to motor and balance
dysfunction.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
27
E0147
F3
#Walker, heavy duty, multiple braking system, variable wheel resistance
E0148
F3
#Walker, heavy duty, without wheels, rigid or folding, any type, each
E0149
F3
#Walker, heavy duty, wheeled, rigid or folding, any type
E0153
F7
#Platform attachment, forearm crutch, each (supports arm)
E0154
F7
#Platform attachment, walker, each (supports arm)
E0155
F7
#Wheel attachment, rigid pick-up walker, per pair
E0156
F4
#Seat attachment, walker
E0157
F7
#Crutch attachment, walker, each
E0159
F7
#Brake attachment for wheeled walker, replacement, each
Pediatric Gait Trainers
- Home pediatric gait trainers provide support and encourage upright positioning for children requiring gait
training/retraining due to motor and balance dysfunction.
- Additional prompts provide adjustment to the center of gravity and trunk angle and support and stimulate
walking movements for a child who requires gait training or retraining due to severe motor and balance
dysfunction.
- Clinical documentation from a trial period must be submitted with the prior approval request.
Coverage Criteria:
- The member is unable to stand or ambulate independently due to conditions such as, but not limited to,
neuromuscular or congenital disorders, including acquired skeletal abnormalities.
- The alignment of the member’s lower extremities is such that they can tolerate a standing or upright position.
- The member does not have orthostatic hypotension, postural tachycardia syndrome, osteogenesis imperfecta,
osteoporosis and other brittle bone diseases.
- The member has demonstrated improved mobility, function and physiologic symptoms or has maintained
ambulation status with the use of the requested gait trainer (when other alternatives have failed) and is able to
follow a home ambulation program incorporating the use of the gait trainer (as documented by clinical
ambulation program or home trial with the requested gait trainer).
- There is a home therapy plan outlining the use of the requested gait trainer.
- The member does not utilize, or require, a home standing device in addition to a walker or gait trainer.
Provision of both a standing system and walker/gait trainer is typically considered a duplication of service, as
both address weight bearing.
Documentation Requirements:
- A prescription including the gait trainer and any modifications/accessories requested.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
28
- A detailed letter of medical necessity (LMN) that includes:
1. A comprehensive history and physical exam by a licensed physician, physical therapist, or occupational
therapist.
2. A summary of the existing medical condition, age at diagnosis, prognosis, and co-morbid conditions.
3. The member’s functional and physical assessment including strength, range of motion, tone, sensation,
balance, ADLs, and functional status.
4. Documentation of failure of less costly alternatives (include make and model of alternatives tried as well as
the length of the trial with each alternative).
5. A home therapy plan outlining the planned use of the requested gait trainer.
- Documentation that the member does not have sufficient access to equipment in an alternative setting, e.g.
clinic, outpatient therapy, etc.
- Documentation regarding the level of caregiver assistance available/needed on daily basis.
- Documentation that the member’s home can accommodate the requested gait trainer and that the
family/caregiver has been trained in the use and maintenance of the requested gait trainer.
E8000
F3
Gait trainer, pediatric size, posterior support, includes all accessories and components
E8001
F3
Gait trainer, pediatric size, upright support, includes all accessories and components
E8002
F3
Gait trainer, pediatric size, anterior support, includes all accessories and components
Wheeled Mobility Equipment (WME), Seating And Positioning Components (SPC)
I. General Clinical and Coverage Criteria for Wheeled Mobility Equipment
- The term wheeled mobility equipment (WME) describes manual wheelchairs (MWC), power mobility
devices (PMD) including power wheelchairs (PWC), power operated vehicles (POV) and push rim
activated power assist devices (PAD). Seating and positioning components (SPC) describe seat, back
and positioning equipment used to optimize the individual’s positioning and level of function in their
wheeled mobility equipment.
- Wheeled mobility equipment is covered if the member’s medical condition(s) and mobility limitation(s)
are such that without the use of the WME, the member’s ability to perform mobility related activities
of daily living (MRADL) in the home and/or community is significantly impaired, and the member is
not ambulatory or functionally ambulatory.
- For these criteria to be met, the member must have an evaluation that was performed by a qualified
practitioner who has specific training and/or experience in wheelchair evaluation and ordering.
- The practitioner must document, to the extent required by the coverage criteria for the specific WME,
how the member’s medical condition supports Medicaid reimbursement.
- The practitioner must have no financial relationship with the supplier.
- If coverage criteria for the WME that is requested or provided are not met and if there is another
device that meets the member’s medical needs, payment will be based on the allowance for the least
costly medically appropriate alternative.
- Determination of least costly alternatives will take into account the member’s weight, seating needs,
amount and type of use and needs for other medically necessary features.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
29
- Reimbursement for the wheelchair codes includes all labor charges involved in the assembly of the
wheelchair. Reimbursement also includes support services, such as delivery, set-up, and education
about the use of the WME. No separate or additional payments will be made for shipping, handling,
delivery or necessary fittings and adjustments.
- Maintaining documentation of least costly alternatives reviewed and attempted is the responsibility of
the ordering practitioner and DMEPOS provider.
- Documentation must be submitted or provided at the time of manual review of a prior approval
request, claim, or audit.
- When a member presents for a medical evaluation for WME and SPC (Seating and Positioning
Components), the sequential consideration of the questions, listed below, by ordering and treating
practitioners provides clinical guidance for the ordering of one appropriate device to meet the
medical need of treating and restoring the member’s ability to perform MRADLs. MRADLs include
dining, personal hygiene tasks and activities specified in a medical treatment plan completed in
customary locations in the home and/or community.
Note: Medicaid funds and maintains one medically necessary manual mobility device to meet the
member’s medical needs whether primarily used in the home, community, or as a back-up to the
primary PWC.
1. Does the member have a mobility limitation that significantly impairs his/her ability to participate in one or
more MRADLs? A mobility limitation is one that:
a) Prevents the member from accomplishing the MRADLs entirely, or
b) Places the member at a reasonably determined heightened risk of morbidity or mortality
secondary to attempts to participate in MRADLs, or
c) Prevents the member from completing the MRADLs within a reasonable time frame.
2. Are there other conditions that limit the member’s ability to participate in MRADLs?
a) Some examples are significant impairment of cognition or judgment and/or vision.
b) For these members, the provision of WME and SPC might not enable them to participate in
MRADLs if the co-morbidity prevents effective use of the wheelchair or reasonable
completion of the tasks even with WME and SPC.
3. If these other limitations exist, can they be ameliorated or compensated sufficiently such that the
additional provision of WME and SPC will be reasonably expected to significantly improve the member’s
ability to perform or obtain assistance to participate in MRADLs?
a) A caregiver, for example a family member, may be compensatory, if consistently available and
willing and able to safely operate and transfer the member to and from the wheelchair and to
transport the member using the wheelchair. The caregiver’s need to use a wheelchair to assist
the member in the MRADLs is to be considered in this determination.
b) If the amelioration or compensation requires the member's compliance with treatment, for
example medications or therapy, substantive non-compliance, whether willing or involuntary,
can be grounds for denial of WME and SPC coverage if it results in the member continuing to
have a significant limitation. It may be determined that partial compliance results in adequate
amelioration or compensation for the appropriate use of WME and SPC.
4. Does the member or caregiver demonstrate the capability and the willingness to consistently operate the
WME and SPC safely and independently?

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
30
a) Safety considerations include personal risk to the member as well as risk to others. The
determination of safety may need to occur several times during the process as the
consideration focuses on a specific device.
b) A history of unsafe behavior may be considered.
5. Can the functional mobility deficit be sufficiently resolved by the prescription of a cane or walker?
a) The cane or walker should be appropriately fitted to the member for this evaluation.
b) Assess the member’s ability to safely use a cane or walker.
6. Does the member’s typical environment support the use of WME and SPC?
a) Determine whether the member’s environment will support the use of these types of WME
and SPC.
b) Keep in mind such factors as physical layout, surfaces, and obstacles, which may render WME
and SPC unusable.
7. Does the member have sufficient upper and/or lower extremity function to propel a manual wheelchair to
participate in MRADLs during a typical day? The manual wheelchair should be optimally configured
(seating and positioning components, wheelbase, device weight, and other appropriate accessories) for
this determination.
a) Limitations of strength, endurance, range of motion, coordination, and absence or deformity
in one or both upper extremities are relevant.
b) A member with sufficient upper extremity function may qualify for a manual wheelchair. The
appropriate type of manual wheelchair, i.e. light weight, etc., should be determined based on
the member’s physical characteristics and anticipated intensity of use.
c) The member’s home should provide adequate access, maneuvering space, and surfaces for
the operation of a manual wheelchair.
d) Assess the member’s ability to safely use a manual wheelchair.
8. Does the member have sufficient strength and postural stability to operate a POV/scooter?
a) A covered POV is a 4-wheeled device with tiller steering and limited seat modification
capabilities. The member must be able to maintain stability and position for adequate
operation without additional SPC (a 3-wheeled device is not covered).
b) The member’s home should provide adequate access, maneuvering space, and surfaces for
the operation of a POV.
c) Assess the member’s ability to safely use a POV/scooter.
d) Consider the potential for progression of some diagnoses.
9. Are the additional features provided by a power wheelchair or powered SPC needed to allow the member
to participate in one or more MRADLs?
a) The pertinent features of a power wheelchair compared to a POV are typically controlled by a
joystick or alternative input device, lower seat height for slide transfers, and the ability to
accommodate a variety of seating needs.
b) The type of wheelchair and options provided should be appropriate for the degree of the
member’s functional impairments.
c) The member's home should provide adequate access, maneuvering space, and surfaces for
the operation of a power wheelchair.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
31
d) Assess the member’s ability to safely and independently use a power wheelchair and powered
SPC.
Note: If the member is unable to use a power wheelchair or power SPC and if there is a caregiver who is available,
willing, and able to provide assistance, a manual wheelchair and manual SPC is appropriate.
Go to http://www.cms.hhs.gov/determinationprocess/downloads/id143c.pdf
for a flow chart developed by the
Medicare program that visually describes the clinical criteria for the evaluation and ordering of WME.
II. Wheeled Mobility Equipment Documentation Requirements
- All services must be supported by the original signed written order from a qualified licensed practitioner. In the
event an order has been telephoned or faxed to the vendor, it is the vendor’s responsibility to obtain the
signed fiscal order from the ordering practitioner within 30 calendar days. A written, faxed, or telephoned
order must be received prior to delivery of the service.
- The fiscal order must be specific to the item being requested. Generic orders such as “wheelchair” or
“wheelchair repairs” are not acceptable. The order must clearly and specifically state the type of repairs being
requested (e.g., “replace seat covering”) or the presenting problem (e.g., “joystick malfunctioning”).
- In addition to the fiscal order, the supplier must maintain the following written documentation of medical
necessity for WME/SPC in the member’s file and/or submit to the Department for review:
1. A description of, and cost quote for all the equipment and components as ordered (e.g., HCPCS code,
make, model, size, seat, and back dimensions) and how they accommodate relevant member
measurements (e.g., height, weight, chest, shoulders, thighs, legs).
2. A statement of the alternatives considered or attempted (e.g., manual versus power, single versus multiple
power option) and why these alternatives do not meet the member’s medical needs.
3. A description of the customary environment and caregiver supports (e.g., skilled nursing facility, OMRDD-
certified residence, private home, home health or waiver services); please give details of the results of trial
of equipment in this environment (e.g., fitting through doorways, access to home, transportable, ability to
safely operate, secure storage space).
4. The practitioner must document medical necessity, to the extent required by the coverage criteria for the
specific WME/SPC; how the member’s medical condition supports Medicaid reimbursement. The
documentation must be summarized and forwarded to the supplier in the form of a qualified practitioner’s
letter of medical justification, an evaluation template and/or, physician's office records, hospital records,
nursing home records, home health agency records, records from other healthcare professionals and test
reports. The practitioner must maintain appropriate and complete medical records even if a letter of
medical justification or evaluation template is provided to the supplier. Examples of medical
documentation which is applicable include but are not limited to:
History:
• Symptoms.
• Explain history of decubitus/skin breakdown, if applicable.
• How long the condition has been present.
• Clinical progression.
• Interventions that have been tried and the results.
• Past use of walker, manual wheelchair, POV, or power wheelchair and the results.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
32
• A list of all current WME and SPC (e.g., make, model, serial number, age) and an explanation of why it
no longer meets the member’s medical needs (suppliers must obtain cost estimates of repair of
equipment).
• Reports of pertinent laboratory tests, x-rays, and/or other diagnostic tests (e.g., pulmonary function
tests, cardiac stress test, electromyogram, etc.) performed in the course of management of the
member.
• Describe other physical limitations or concerns (e.g., respiratory).
• Describe any recent or expected changes in medical, physical, or functional status.
Physical exam
:
• Related diagnoses.
• Impairment of strength, range of motion, sensation, or coordination of arms and legs.
• Presence of abnormal tone or deformity of arms, legs, or trunk.
• Neck, trunk, and pelvic posture and flexibility.
• Sitting and standing balance.
• Measurements of height, weight, chest, shoulders, hips, legs.
• Absent or impaired sensation in the area of contact with the seating surface.
• Physicians shall document the examination in a detailed narrative note in their charts in the format that
they use for other entries. The note must clearly indicate that a major reason for the visit was a mobility
examination.
Functional assessment
:
• Describe MRADL capabilities and any problems with performing MRADLs, including the need to
use a cane, walker, or the assistance of another person.
• Describe activities, other than MRADLs, performed while in wheelchair.
• Transferring between a bed, chair, commode, toilet and WME.
• Walking around customary environment – provide information on distance walked, speed, and
balance.
• Ability to carry out a functional weight shift.
• Describe in detail any significant postural asymmetries with applicable quantitative measurements
(e.g., scoliosis, leg length discrepancy).
• Describe feeding capabilities and seating modifications required to facilitate feeding capabilities.
• Specifics of why less costly alternatives are not medically appropriate based on the member’s
medical needs.
Plan of Care
:
• Intended use and amount of time daily the equipment is used and, degree of ambulation in
customary environment.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
33
• What MRADLs will the member participate in with the new WME and SPC.
• A narration of medical necessity for the WME and SPC, describing what medical needs specific to
the member will be met if the equipment is provided.
• An estimate of how long the equipment will be needed.
• If surgery is anticipated, indicate the CPT Procedure code(s) and ICD Diagnosis code(s) and
expected surgery date.
• Describe anticipated modifications or changes to the equipment within the next three years.
• Describe the growth potential of the requested equipment in number of years.
• For SPC, describe whether it can be integrated into a new or existing wheelchair.
5. For members who receive a Group 2 Single Power Option or Multiple Power Options PWC, any Group 3 or
Group 4 PWC, or a push-rim activated power assist device, the evaluation must provide detailed
information explaining why each specific option or accessory is needed to address the member’s mobility
limitation.
6. Prior to or at the time of delivery of a MWC, POV, or PWC, the supplier, practitioner, or case manager
must perform an on-site evaluation of the member’s home to verify that the member can adequately
maneuver the device that is provided considering physical layout, doorway width, doorway thresholds, and
surfaces. The evaluation should also include a description of the secure storage space in the member’s
home for the wheeled mobility device. Whether the WME is approved for the home and/or community,
the WME provided must have an accessible secure storage space in the home. A written report of this
evaluation should be available on request.
See the following link for an example of an evaluation form template Wheelchair and Seating Assessment Guide
. This
form is not a required element of the medical record or prior approval submission. Although a practitioner-completed
form is considered part of the medical record, it is not a substitute for the comprehensive medical record as noted
above. If only a form is provided to the supplier, the documentation, to the extent required by the coverage criteria for
the specific WME/SPC, present on the form must describe how the member’s medical condition supports Medicaid
reimbursement. If the evaluation form, letter of medical justification or medical records of a licensed/certified medical
professional (LCMP) (e.g., physical or occupational therapist) is to be considered as part of the medical record, there
must be a signed and dated attestation by the supplier that the LCMP has no financial relationship with the supplier.
Documentation without such an attestation will not be considered part of the medical record for prior approval or
audit purposes. Documentation must contain the therapist's name and licensure, evaluation date, phone number,
address, and employer.
III. Manual Wheelchairs
Manual Wheelchairs are covered when:
- Criterion 1-5 are met; and
- Criterion 6 or 7 is met, and
- Criterion is met for specific devices listed below:
1. The member has a mobility limitation that significantly impairs his/her ability to participate in one or more
MRADL, and

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
34
2. The member’s mobility limitation cannot be sufficiently resolved using an appropriately fitted cane or
walker, and
3. The manual wheelchair supplied to the member for use in the home and/or community settings provides
adequate access to these settings (e.g., between rooms, in and out of the home, transportation and over
surfaces), and
4. Use of a manual wheelchair will significantly improve the member’s ability to participate in MRADLs and
the member will use it on a regular basis, and
5. The member has not expressed an unwillingness to use the manual wheelchair that is provided, and
6. The member has sufficient upper extremity and/or lower extremity function and other physical and mental
abilities needed to safely self-propel the manual wheelchair during a typical day. Limitations of strength,
endurance, range of motion, or coordination, presence of pain, or deformity or absence of one or both
upper extremities are relevant to the assessment of upper extremity function, or
7. The member has a caregiver who is available, willing, and able to provide assistance with the wheelchair.
Reimbursement price for all manual wheelchairs includes:
1. any type arm style or armrest, arm pad
2. seat (a medically indicated non-standard seat, back cushion or seating system that is not included by the
manufacturer may be billed separately)
3. standard leg rest
4. standard footrest
5. safety belt/pelvic strap (2-point)
6. solid tires and casters, metal hand rims
7. brakes
8. side guards (any type)
9. push/attendant handles (any type)
(The above parts may not be billed separately with a new wheelchair.)
Codes and descriptions:
E1161
F3
#Manual adult size wheelchair, includes tilt-in-space
E1229
F3
Wheelchair, pediatric size, not otherwise specified
E1233
F3
#Wheelchair, pediatric size, tilt-in-space, rigid, adjustable, without seating system (E2231 solid
seat included)
E1234
F3
#Wheelchair, pediatric size, tilt-in-space, folding, adjustable, without seating system
- Manual tilt-in-space wheelchairs (E1161, E1233, and E1234) are covered when:
a) The member is not independent with transfers, and
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
35
b) The member has a plan of care that addresses the medical need for frequent positioning changes (e.g.,
for pressure reduction or poor/absent trunk control) that do not always include a tilt position.
- Pediatric tilt-in-space wheelchairs satisfy future growth capability, attendant, or user-controlled tilt, multi
position tilt, transit system, attendant handles, 10-18” width, 13-18” depth and standard back heights.
- Adult tilt-in-space wheelchairs feature attendant or user-controlled tilt, multi position tilt, transit system,
attendant handles, 14-19” width and standard depth and back height.
- A combination of manual tilt-in-space along with manual recline option is covered when the member meets
the coverage criteria for both components and when provided alone, one function will not meet their seating
and positioning needs.
E1236
F3
Wheelchair, pediatric size, folding, adjustable, with seating system (Limited to stroller-style mobility
devices only)
- Code includes all accessories, parts, and seating. Wheelchair accessory codes are not to be
used at initial issue or for replacement parts.
- All requested repairs and replacement parts should be submitted for prior approval review
using code E1236 RB.
- Strollers (E1236) are covered when supporting documentation:
a) illustrates why a manual wheelchair (E1161, E1233, E1234, K0001-K0009) would not
meet the member’s medical needs in their customary environment.
b) selection is not based solely on caregiver convenience but on medical need of the
member.
c) confirms there is no presence of severe, fixed postural deviations or contractures.
K0001
F4
‘-RR’
#Standard wheelchair
A standard wheelchair is covered when:
(a) The member can self-propel the wheelchair, or
(b) Propel with assistance.
This wheelchair features heavy steel cross adult frame and fixed rear axle position, 16/18” width, 16”
depth, and 16/18/20” back.
K0002
F4
‘-RR’
#Standard hemi (low seat) wheelchair
A standard hemi -wheelchair is covered:
(a) For disarticulation of one or both lower extremities, or
(b) Requires a lower seat height because of short stature, or
(c) To enable the member to place his/her feet on the ground for propulsion.
This wheelchair features heavy steel cross frame and fixed rear axle position, 16/18” width, 16” depth,
and 16-18” back.
K0003
F3
‘-RR’
#Lightweight wheelchair
A lightweight wheelchair is covered:
(a) When a member’s medical condition and the weight of the wheelchair affects the member’s
ability to self-propel, or
(b) For a member with marginal propulsion skills.
This wheelchair features an adult, hemi or pediatric folding frame, aluminum or steel cross frame,
fixed rear axle position, 14/16/18” width, 16/18” depth, and 16-18” back
K0004
F3
‘-RR’
#High strength, lightweight wheelchair
A high strength lightweight wheelchair is covered when:
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
36
(a) The member’s medical condition and the weight of the wheelchair affects the member’s ability to
self-propel while engaging in frequent MRADLs that cannot be performed in a standard or
lightweight wheelchair, or
(b) The member requires a seat width, depth, or height that cannot be accommodated in a standard,
lightweight or hemi-wheelchair.
This wheelchair features an adult, hemi, or pediatric folding frame, limited rear axle adjustment,
lightweight tires and casters, 12-20” width, 16-19” depth and 16-19” back.
K0005
F3
#Ultra lightweight wheelchair
An ultra lightweight multi-adjustable wheelchair is covered when:
(a) The member’s medical condition and the weight of the wheelchair affects the member’s ability to
self-propel while engaging in frequent MRADLs that cannot be performed in a standard, lightweight
or high strength lightweight wheelchair, and
(b) The member’s medical condition and the position of the push rim in relation to the member’s
arms and hands is integral to the ability to self-propel the wheelchair effectively, and
(c) The member has demonstrated the cognitive and physical ability to self-propel the wheelchair
independently and functionally, or
(d) The member’s medical condition requires multi-adjustable features or dimensions that are not
available in a less costly wheelchair (e.g., pediatric size and growth options).
A high-strength multi-adjustable (e.g.: depth adjustable back, adjustable seat to floor angle,
adjustable seat to back angle) wheelchair features low rolling resistance, a fully adjusting rear axle,
any type push handles, transport option, quick release axles, and folding or rigid pediatric or adult
frame. Additionally, the weight distribution may be changed, adjusting the ease or difficulty of self-
propulsion. This wheelchair features 11-19” width, 12-19” depth, and 17-20” back.
Note:
Ultra lightweight wheelchairs should not be dispensed as back-up manual wheelchairs unless
due to the required dimensions not being available in less costly alternatives (e.g., pediatric size and
growth options).
K0006
F3
‘-RR’
#Heavy-duty wheelchair
A heavy-duty wheelchair is covered when:
(a) The member weighs more than 250 pounds, or
(b) The member has severe spasticity, or
(c) Body measurements cannot be accommodated by standard sized wheelchairs.
This wheelchair features a reinforced folding cross frame, 300 lb. weight capacity, reinforced seat and
back, fixed rear axle position, calf pads, 20-22” width, 16-19” depth, and 18-20” back.
K0007
F3
#Extra heavy-duty wheelchair
An extra heavy duty (K0007) wheelchair is covered when:
(a) The member weighs more than 300 pounds, or
(b) Body measurements cannot be accommodated by a heavy-duty wheelchair.
In addition to the features provided in a heavy-duty wheelchair, a double cross brace and dual or
triple axle positioning, 19-24” width, 16-20” depth and low/medium/tall backs are featured.
K0009
F5
Other manual wheelchair/base
This code is to be used for members with medical needs for features in addition to those indicated
for the wheelchair and/or accessory codes listed. Custom-made wheelchairs feature a wheelchair
frame that is uniquely constructed or substantially modified for a specific member and is covered if
the feature needed is not available in an already manufactured wheelchair or accessory. The
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
37
assembly of a wheelchair from modular components and the use of customized options do not meet
the requirements for a custom-made wheelchair.
Back-up Manual Wheelchair
Back-up manual wheelchairs are covered when:
- the member meets the criteria for a power mobility device, and
- the member meets the criteria for the rented or purchased back-up manual wheelchair, and
- the member is unable to complete MRADLs without a back-up manual wheelchair, and
- the back-up wheelchair accommodates the SPC on the primary wheelchair.
If the SPC is integrated into the primary power wheelchair and cannot be removed or transferred with appropriate
hardware, Medicaid would consider secondary seating for the back-up manual wheelchair. Documentation for the
secondary seating must include:
- the make/model of the power wheelchair; AND
- make/model of the seating system that cannot be transferred; AND
- documentation from the power wheelchair manufacturer that the seating cannot be removed.
Note: Ultra lightweight wheelchairs should not be dispensed as back-up manual wheelchairs unless due to the
required dimensions not being available in less costly alternatives (e.g., pediatric size and growth options).
Pediatric sized folding adjustable wheelchairs with seating systems are covered as primary or back-up wheeled mobility
when:
- the member meets the criteria for wheeled mobility, and
- the wheelchair is an appropriate size for the member, and
- the member meets the criteria for recline and positioning options, and
- the wheelchair provides growth capability in width and length.
IV. Powered Mobility Devices (PMD)
Are covered when:
- Criterion 1-3 are met, and
- Criterion is met for specific devices listed below.
1. The member has a mobility limitation that impairs his or her ability to participate in one or more MRADL,
and
2. The member’s mobility limitation cannot be sufficiently and safely resolved using an appropriately fitted
cane or walker, and
3. The member does not have sufficient upper extremity function to self-propel an optimally configured manual
wheelchair to perform MRADLs during a typical day. Limitations of strength, endurance, range of motion, or
coordination, presence of pain, or deformity or absence of one or both upper extremities are relevant to the

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
38
assessment of upper extremity function. An optimally configured manual wheelchair is one with an appropriate
wheelbase, device weight, seating options, and other appropriate non-powered accessories.
Note: A PMD will be denied as not medically necessary if the underlying condition is reversible and the length of need is
less than 3 months (e.g., following lower extremity surgery which limits ambulation).
Power Operated Vehicles (POV)
Four-wheeled, are covered if all the basic coverage criteria (1-3) for PMDs have been met and if criteria (4-9) are also
met.
4. The member can:
a) Safely transfer to and from a POV, and
b) Operate the tiller steering system, and
c) Maintain postural stability and position in standard POV seating while operating the POV without the use
of any additional positioning aids.
5. The member’s mental capabilities (e.g., cognition, judgment) and physical capabilities (e.g., vision) are
sufficient for safe mobility using a POV in the home, and
6. The member’s home provides adequate access between rooms, adequate maneuvering space, and a secure
storage space for the operation of the POV that is provided, and
7. The member’s weight is less than or equal to the weight capacity of the POV that is provided, and
8. Use of a POV will significantly improve the member’s ability to participate in MRADLs, and
9. The member has not expressed an unwillingness to use a POV.
NOTE: Group 2 POVs have added capabilities that must be medically justified; otherwise, payment will be based on the
allowance for the least costly medically appropriate alternative, the comparable Group 1 POV. If coverage criteria 1-9 are
met and if a member’s weight can be accommodated by a POV with a lower weight capacity than the POV that is
provided, payment will be based on the allowance for the least costly medically appropriate alternative.
Reimbursement price for all POV includes:
1. Battery or batteries required for operation
2. Battery charger single mode
3. Weight appropriate upholstery and seating system
4. Tiller steering
5. Non-expandable controller with proportional response
6. Complete set of tires
7. All accessories needed for safe operation
(The above parts may not be billed separately with a new POV.)
Repairs to a POV:
• Base codes for POVs includes all accessories, parts and seating. Power wheelchair accessory codes are not to
be used at initial issue or for replacement parts.
• All requested repairs and replacement parts should be submitted for prior approval review using code K0800
RB unless the repair is less than 25% of the base code’s MRA. Less than 25% of the base code can be directly
billed twice per year.
Codes and Descriptions:
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
39
Group 1 (POVs)
Features: Width less than or equal to 28 inches, length less than or equal to 48 inches, minimum top end speed-flat
3mph, minimum range 5 miles, minimum obstacle climb 20 mm, radius pivot turn less than or equal to 54 inches,
dynamic stability incline 6 degrees, fatigue cycle test 200,000 cycles, and drop test 6,666 cycles.
K0800
F3
Power operated vehicle, group 1 standard, patient weight capacity up to and Including 300 pounds
K0801
F3
Power operated vehicle, group 1 heavy duty, patient weight capacity 301 to 450 Pounds
K0802
F3
Power operated vehicle, group 1 very heavy duty, patient weight capacity 451 to 600 pounds
Group 2 (POVs)
Features: Width less than or equal to 28 inches, length less than or equal to 48 inches, minimum top end speed-flat 4
mph, minimum range 10 miles, minimum obstacle climb 50 mm, radius pivot turn less than or equal to 54 inches,
dynamic stability incline 7.5 degrees, fatigue cycle test 200,000 cycles, and drop test 6,666 cycles.
K0806
F3
Power operated vehicle, group 2 standard, patient weight capacity up to and Including 300 pounds
K0807
F3
Power operated vehicle, group 2 heavy duty, patient weight capacity 301 to 450 Pounds
K0808
F3
Power operated vehicle, group 2 very heavy duty, patient weight capacity 451 to 600 pounds
K0812
F3
Power operated vehicle, not otherwise classified
Power Wheelchairs (PWC)
Covered if all the basic coverage criteria (1-3) for PMDs have been met and:
- The member does not meet coverage criterion 4, 5, or 6 for a POV; and
- Criterion 10-13 (below) are met; and
- Any coverage criteria pertaining to the specific wheelchair grouping (see below) are met.
10. The member has the mental and physical ability to safely and independently operate the power wheelchair that
is provided, and
11. The member’s weight is less than or equal to the weight capacity of the power wheelchair that is provided, and
12. The member’s home and/or community environments provide adequate access between rooms, in and out of
the home, maneuvering space and over surfaces for the operation of the power wheelchair that is provided,
and
13. The member has not expressed an unwillingness to use a power wheelchair.
Reimbursement price for all power wheelchairs (PWCs) includes the following accessories:
1. Lap belt or safety belt
2. Battery or batteries required for operation
3. Battery charger single mode
4. Complete set of tires and casters, any type
5. Fixed, swing away or detachable non-elevating leg rests with or without calf pad
Elevating leg rests may be billed separately.
6. Fixed, swing away or detachable footrests or a foot platform without angle adjustment with or without calf
pad
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
40
There is no separate billing for angle adjustable footplates with Group 1 or 2. Angle adjustable footplates
may be billed separately with Group 3, 4 and 5
7. Fixed, swing away, or detachable non-adjustable height armrests with arm pad
Adjustable height armrests may be billed separately
8. Joystick standard proportional (integrated or remote)
A non-proportional or mini, compact or short throw proportional joystick or other alternative control device
may be billed separately with a Group 2 or Group 3 wheelchair.
9. Joystick hardware, fixed, swing away and/or retractable
10. Controller and Input Device – Non-expandable controller and a standard proportional joystick (integrated
or remote)
11. Any weight specific components (braces, bars, upholstery, brackets, motors, gears, etc.) as required by
patient weight capacity
12. Any seat width and depth. Exception: for Group 3 and 4 PWCs with a sling/solid seat/back the following
may be billed separately:
a. For Standard Duty, seat width and/or depth greater than 20 inches,
b. For Heavy Duty, back width greater than 22 inches,
c. For Very Heavy Duty, back width greater than 24 inches,
d. For Extra Heavy Duty, no separate billing
13. Any back width. Exception: for Group 3 and 4 PWCs with a sling/solid seat/back, the following may be
billed separately:
a. For Standard Duty, back width greater than 20 inches,
b. For Heavy Duty, seat width and/or depth greater than 22 inches,
c. For Very Heavy Duty, seat width and/or greater than 24 inches,
d. For Extra Heavy Duty, no separate billing
14. Transit option/Transport brackets
15. Push/attendant handles (any type)
16. Attendant control joystick/controller: When an alternate drive control (e.g.: head array, min proportional
joystick, etc.) is provided on a new power wheelchair, an attendant control would not be separately payable.
The MRA for a new power wheelchair includes a joystick.
PWC Seating
- A sling/solid seat is a rigid metal or plastic material usually covered with cloth, vinyl, leather or equal material,
with or without some padding material designed to serve as the support for the buttocks or back of the user
respectively. They may or may not have thin padding but are not intended to provide cushioning or positioning
for the user. PWC’s with an automatic back and a solid seat pan are considered as a solid seat/back system, not
Captains Chair.
- A Captain’s Chair is a one or two-piece automotive-style seat with a rigid frame, cushioning material in both seat
and back sections, covered in cloth, vinyl, leather or equal upholstery, and designed to serve as a complete
seating, support, and cushioning system for the user. It may have armrests that can be fixed, swing away, or
detachable. It will not have a headrest. Chairs with stadium style seats are billed using the captain’s chair codes.
If medically necessary, refer to positioning/ skin protection seat/back codes and bill the PWC using a sling/solid
seat code.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
41
PWC Power Options
- Power Options are defined as tilt, recline, elevating seat, and power standing. These may be added to a PWC
to accommodate a patient’s specific medical need for seating and positioning assistance.
- No power options- A category of PWCs that is incapable of accommodating any power options.
- Single power option- A category of PWCs with the capability to accept and operate only one power option at a
time on the base. A PMD does not have to be able to accommodate all features to qualify for this code. For
example, a power wheelchair that can only accommodate a power tilt could qualify for this code.
- Multiple Power Option- A category of PWC with the capability to accept and operate more than one power
option at a time on the base. A PWC does not have to accommodate all features from the defined list of power
options to qualify for this code but must be capable of having more than one power feature present and
operational on the PWC at the same time.
- Proportional control input device is a device that transforms a user’s drive command (a physical action initiated
by the user) into a corresponding and comparative movement, both in direction and in speed, of the wheelchair.
The input device shall be considered proportional if it allows for both a non-discrete directional command and
a non-discrete speed command for a single drive command movement.
Codes and Descriptions:
Group 1 Power Wheelchairs
Features: Standard duty, 300 pounds or less, length less than or equal to 40 inches, width less than or equal to 24
inches, minimum top end speed-flat 3 mph, minimum range 5 miles, minimum obstacle climb 20 mm, and fatigue
cycle test 6 degrees, fatigue cycle test 200,000 cycles, drop test 6,666 cycles, standard integrated or remote
proportional control input device, non-expandable controller, largest single component not to exceed 55 pounds
(portable only), incapable of upgrade to expandable controllers, incapable of upgrade to alternative control devices,
may have cross brace construction, accommodates non-powered options and seating systems (e.g., recline only backs,
manually elevating leg rests).
K0813
F3
Power wheelchair, group 1 standard, portable, sling/solid seat and back, patient weight capacity up to
and including 300 pounds
K0814
F3
Power wheelchair, group 1 standard, portable, captains chair, patient weight capacity up to and
including 300 pounds
K0815
F3
Power wheelchair, group 1 standard, sling/solid seat and back, patient weight capacity up to and
including 300 pounds
K0816
F3
Power wheelchair, group 1 standard, captains chair, patient weight capacity up to and including 300
pounds
Group 2 Power wheelchairs
Features: Length less than or equal to 48 inches, width less than or equal to 34 inches, minimum top end speed-flat 3
mph, minimum range 7 miles, minimum obstacle climb 40 mm, dynamic stability incline 6 degrees, fatigue cycle test
200,000 cycles, drop test 6,666 cycles, standard integrated or remote proportional control input device, may have cross
brace construction, accommodates seating and positioning items (e.g., seat and back cushions, headrests, lateral trunk
supports, lateral hip supports, medial thigh supports) (except captain’s chairs).
No Power Options

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
42
Features: In addition to standard Group 2 features, has non-expandable controller, incapable of upgrade to expandable
controllers, incapable of upgrade to alternative control devices, largest single component not to exceed 55 pounds
(portable only), accommodates non-powered options and seating systems (e.g., recline only backs, manually elevating
leg rests).
K0820
F3
Power wheelchair, group 2 standard, portable, sling/solid seat/back, patient weight capacity up to and
including 300 pounds
K0821
F3
Power wheelchair, group 2 standard, portable, captains chair, patient weight capacity up to and
including 300 pounds
K0822
F3
Power wheelchair, group 2 standard, sling/solid seat/back, patient weight capacity up to and including
300 pounds
K0823
F3
Power wheelchair, group 2 standard, captains chair, patient weight capacity up to and including 300
pounds
K0824
F3
Power wheelchair, group 2 heavy duty, sling/solid seat/back, patient weight capacity 301 to 450
pounds
K0825
F3
Power wheelchair, group 2 heavy duty, captains chair, patient weight capacity 301 to 450 pounds
K0826
F3
Power wheelchair, group 2 very heavy duty, sling/solid seat/back, patient weight capacity 451 to 600
pounds
K0827
F3
Power wheelchair, group 2 very heavy duty, captains chair, patient weight capacity 451 to 600 pounds
K0828
F3
Power wheelchair, group 2 extra heavy duty, sling/solid seat/back, patient weight capacity 601 pounds
or more
K0829
F3
Power wheelchair, group 2 extra heavy duty, captains chair, patient weight 601 pounds or more
Single Power Option
Covered if all the coverage criteria (1-3, 10-13) for a PWC are met and if:
1. The member meets coverage criteria for a power tilt, power recline, or power elevating seating system and the
system is being used on the wheelchair.
Features: In addition to Group 2 standard features, non-expandable controller, capable of upgrade to expandable
controllers, capable of upgrade to alternative control devices, accommodates only one powered seating system at a time
on the base.
K0835
F3
Power wheelchair, group 2 standard, single power option, sling/solid seat/back, patient weight capacity
up to and including 300 pounds
K0836
F3
Power wheelchair, group 2 standard, single power option, captains chair, patient weight capacity up to
and including 300 pounds
K0837
F3
Power wheelchair, group 2 heavy duty, single power option, sling/solid seat/back, patient weight
capacity 301 to 450 pounds
K0838
F3
Power wheelchair, group 2 heavy duty, single power option, captains chair, patient weight capacity 301
to 450 pounds
K0839
F3
Power wheelchair, group 2 very heavy duty, single power option sling/solid seat/back, patient weight
capacity 451 to 600 pounds
K0840
F3
Power wheelchair, group 2 extra heavy duty, single power option, sling/solid seat/back, patient weight
capacity 601 pounds or more
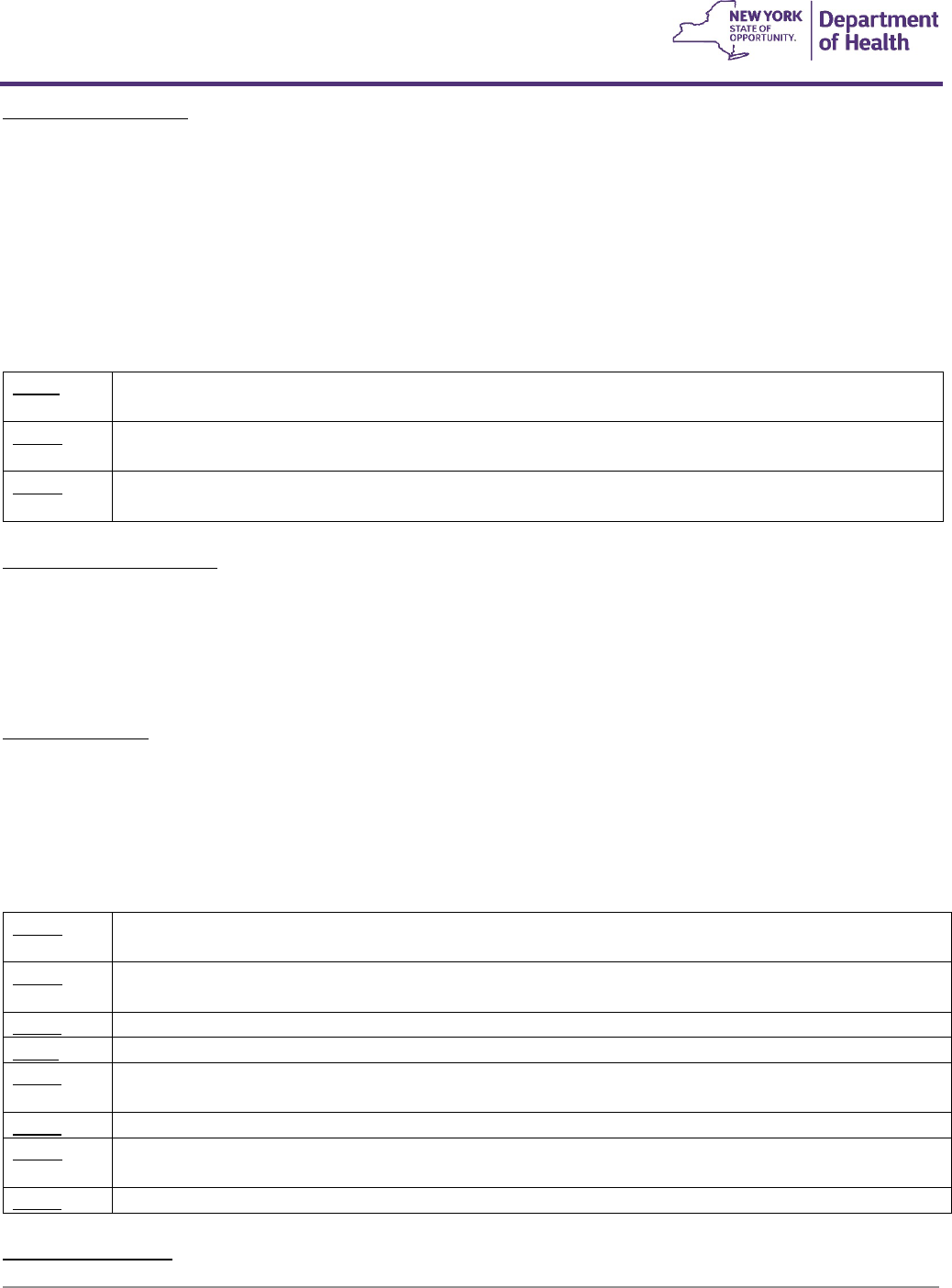
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
43
Multiple Power Options
Covered if all the coverage criteria (1-3, 10-13) for a PWC are met and if criterion 1 or 2 below is met:
1. The member meets coverage criteria for a power tilt and recline seating system and the system is being used
on the wheelchair, or
2. The member uses a ventilator which is mounted on the wheelchair.
Features: In addition to Group 2 standard features, expandable controller at initial use, capable of upgrade to alternative
control devices, accommodates more than one powered seating system at a time on the base, and accommodates
ventilators.
K0841
F3
Power wheelchair, group 2 standard, multiple power option, sling/solid seat/back, patient weight
capacity up to and including 300 pounds
K0842
F3
Power wheelchair, group 2 standard, multiple power option, captains chair, patient weight capacity up
to and including 300 pounds
K0843
F3
Power wheelchair, group 2 heavy duty, multiple power option, sling/solid seat/back, patient weight
capacity 301 to 450 pounds
Group 3 Power wheelchairs
Features: Length less than or equal to 48 inches, width less than or equal to 34 inches, minimum top end speed-flat 4.5
mph, minimum range 12 miles, minimum obstacle climb 60 mm, dynamic stability incline 7.5 degrees, fatigue cycle test
200,000, drop test 6,666 cycles, standard integrated or remote proportional control, drive wheel suspension to reduce
vibration, may not have cross brace construction, accommodates seating and positioning items (e.g. seat and back
cushions, headrests, lateral trunk supports, lateral hip supports, medial thigh supports) (except captain’s chairs).
No Power Options
Covered if all the coverage criteria (1-3, 10-13) for a PWC are met and if the member's mobility limitation is due to a
neurological condition, myopathy, or congenital skeletal deformity.
Features: In addition to Group 3 standard features, non-expandable controller, capable of upgrade to expandable
controllers, capable of upgrade to alternative control devices, accommodates non-powered options and seating systems
(e.g., recline only backs, manually elevating leg rests).
K0848
F3
Power wheelchair, group 3 standard, sling/solid seat/back, patient weight capacity up to and including
300 pounds
K0849
F3
Power wheelchair, group 3 standard, captains chair, patient weight capacity up to and including 300
pounds
K0850
F3
Power wheelchair, group 3 heavy duty, sling/solid seat/back, patient weight capacity 301 to 450 pounds
K0851
F3
Power wheelchair, group 3 heavy duty, captains chair, patient weight capacity 301 to 450 pounds
K0852
F3
Power wheelchair, group 3 very heavy duty, sling/solid seat/back, patient weight capacity 451 to 600
pounds
K0853
F3
Power wheelchair, group 3 very heavy duty, captains chair, patient weight capacity 451 to 600 pounds
K0854
F3
Power wheelchair, group 3 extra heavy duty, sling/solid seat/back, patient weight capacity 601 pounds
or more
K0855
F3
Power wheelchair, group 3 extra heavy duty, captains chair, patient weight capacity 601 pounds or more
Single Power Options
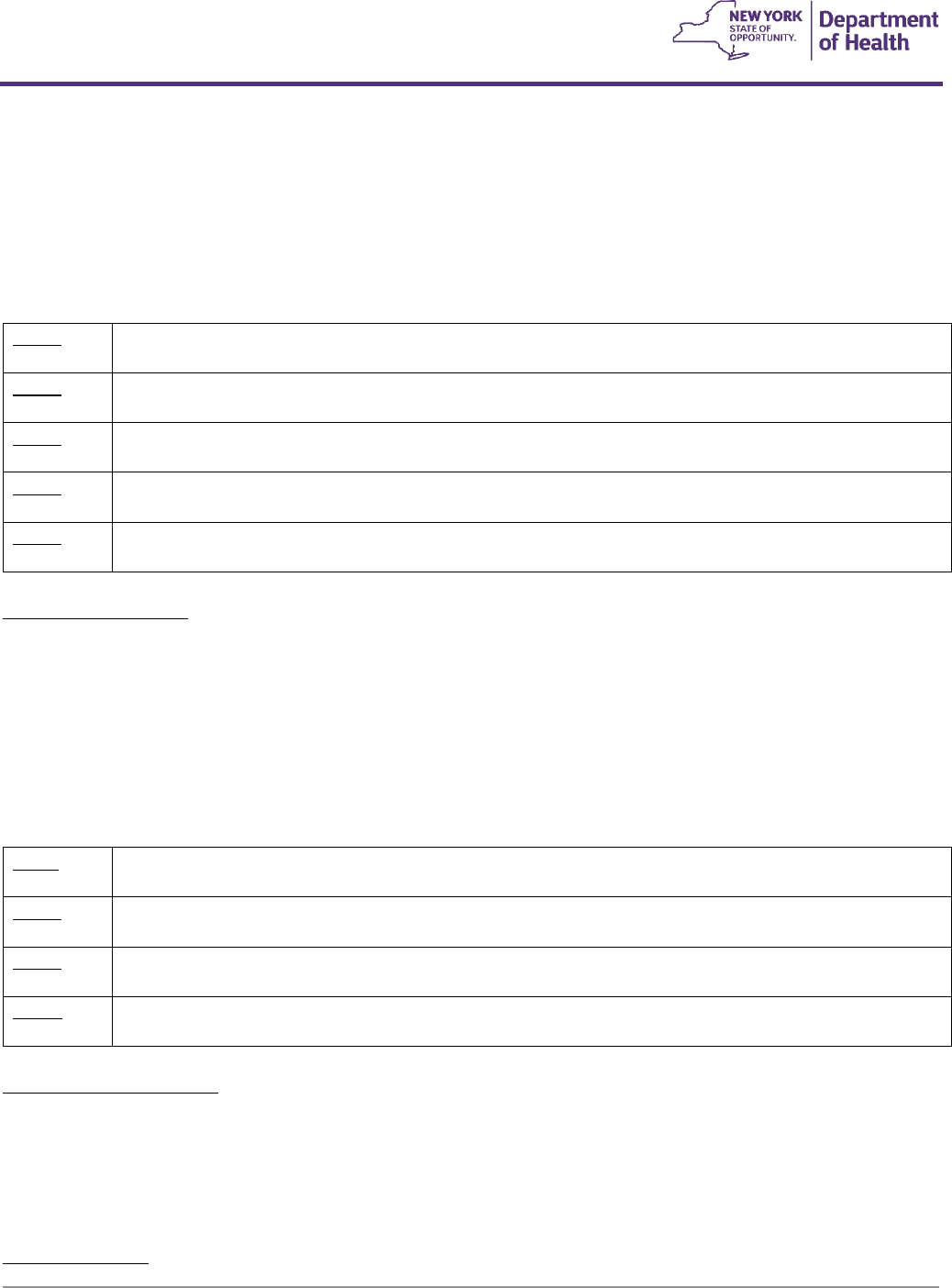
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
44
Covered if all the coverage criteria (1-3, 10-13) for a PWC are met and if:
1. The Group 3 No Power Option criteria are met, and
2. The Group 2 Single Power Option criteria are met.
Features: In addition to Group 3 standard features, non-expandable controller, capable of upgrade to expandable
controllers, capable of upgrade to alternative control devices, accommodates only one powered seating system at a
time on the base.
K0856
F3
Power wheelchair, group 3 standard, single power option, sling/solid seat/back, patient weight capacity
up to and including 300 pounds
K0857
F3
Power wheelchair, group 3 standard, single power option, captains chair, patient weight capacity up to
and including 300 pounds
K0858
F3
Power wheelchair, group 3 heavy duty, single power option, sling/solid seat/back, patient weight 301 to
450 pounds
K0859
F3
Power wheelchair, group 3 heavy duty, single power option, captains chair, patient weight capacity 301
to 450 pounds
K0860
F3
Power wheelchair, group 3 very heavy duty, single power option, sling/solid seat/back, patient weight
capacity 451 to 600 pounds
Multiple Power Options
Covered if all the coverage criteria (1-3, 10-13) for a PWC are met and if:
1. The Group 3 no power option criteria are met, and
2. The Group 2 Multiple Power Options are met.
Features: In addition to Group 3 standard features, expandable controller at initial use, capable of upgrade to alternative
control devices, accommodates more than one powered seating system at a time on the base, and accommodates
ventilators.
K0861
F3
Power wheelchair, group 3 standard, multiple power option, sling/solid seat/back, patient weight
capacity up to and including 300 pounds
K0862
F3
Power wheelchair, group 3 heavy duty, multiple power option, sling/solid seat/back, patient weight
capacity 301 to 450 pounds
K0863
F3
Power wheelchair, group 3 very heavy duty, multiple power option, sling/solid seat/back, patient weight
capacity 451 to 600 pounds
K0864
F3
Power wheelchair, group 3 extra heavy duty, multiple power option, sling/solid seat/back, patient weight
capacity 601 pounds or more
Group 4 Power wheelchairs
Features: Length less than or equal to 48 inches, width less than or equal to 34 inches, minimum top end speed-flat 6
mph, minimum range 16 miles, minimum obstacle climb 75 mm, dynamic stability incline 9 degrees, fatigue cycle test
200,000 cycles, drop test 6,666 cycles, standard integrated or remote proportional control, may not have cross brace
construction, and accommodates seating and positioning items (e.g. seat and back cushions, headrests, lateral trunk
supports, lateral hip supports, medial thigh supports) (except captain’s chairs).
No Power Options
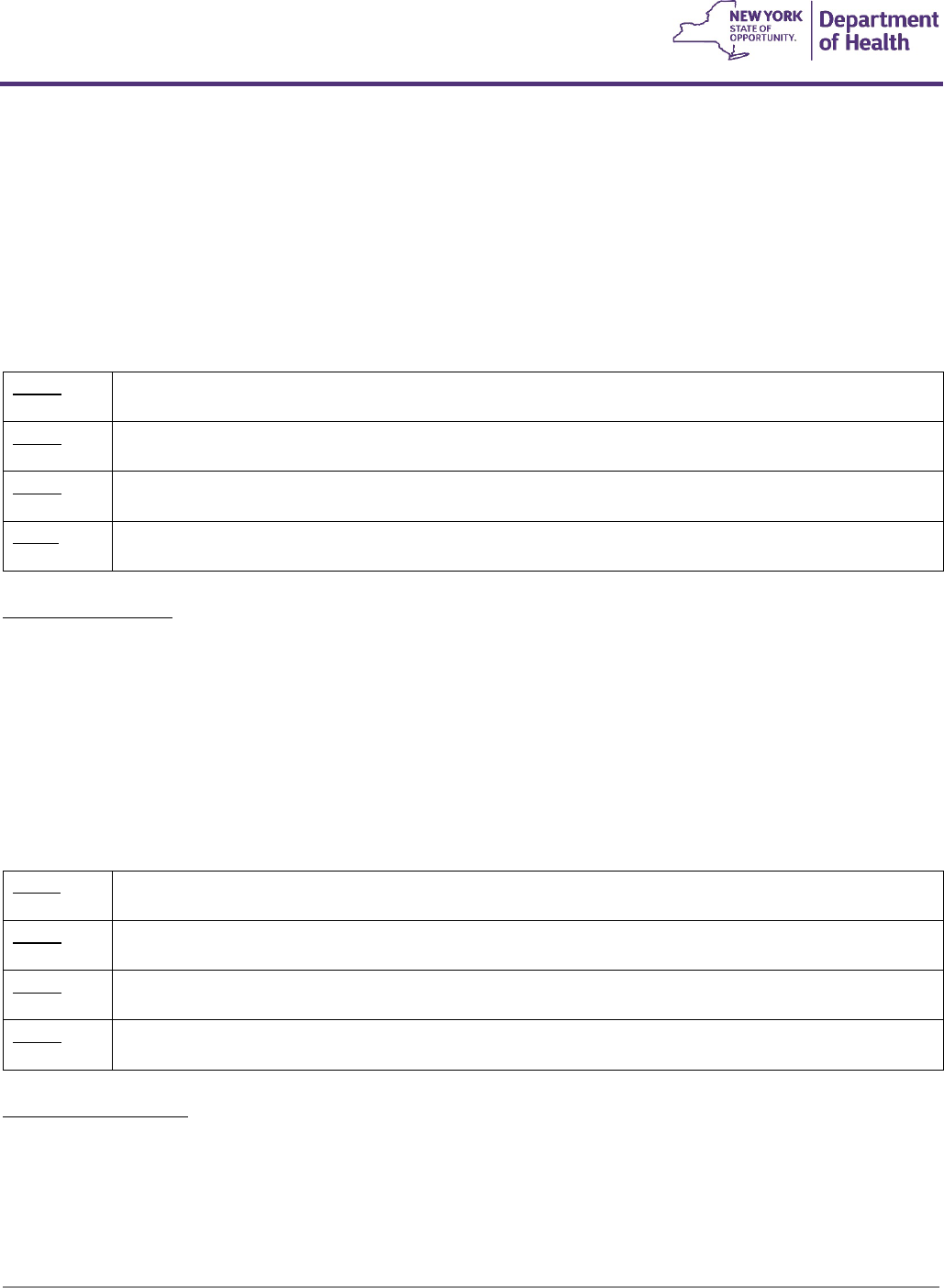
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
45
A Group 4 PWC with no power options (K0868-K0871) is covered if all of the coverage criteria (1-3, 10-13) for a PWC are
met and if:
1. The Group 3 criteria are met, and
2. The minimum range, top end speed, obstacle climb or dynamic stability incline that is medically necessary for
the patient engaging in frequent MRADLs cannot be performed in a Group 3 PWC.
Features: In addition to Group 4 standard features, non-expandable controller, capable of upgrade to expandable
controllers, capable of upgrade to alternative control devices, accommodates non-powered options and seating
systems (e.g. recline only backs, manually elevating leg rests).
K0868
F3
Power wheelchair, group 4 standard, sling/solid seat/back, patient weight capacity up to and including
300 pounds
K0869
F3
Power wheelchair, group 4 standard, captains chair, patient weight capacity up to and including 300
pounds
K0870
F3
Power wheelchair, group 4 heavy duty, sling/solid seat/back, patient weight capacity 301 to 450
pounds
K0871
F3
Power wheelchair, group 4 very heavy duty, sling/solid seat/back, patient weight capacity 451 to 600
pounds
Single Power Options
Covered if all the coverage criteria (1-3, 10-13) for a PWC are met and if:
1. The Group 4 no power option criteria are met, and
2. The Group 2 Single Power Option criteria.
Features: In addition to Group 4 standard features, non-expandable controller, drive wheel suspension to reduce
vibration, capable of upgrade to expandable controllers, capable of upgrade to alternative control devices,
accommodates non-powered options and seating systems (e.g. recline-only, backs, manually elevating leg rests), and
accommodates only one powered seating system at a time on the base.
K0877
F3
Power wheelchair, group 4 standard, single power option, sling/solid seat/back, patient weight capacity
up to and including 300 pounds
K0878
F3
Power wheelchair, group 4 standard, single power option, captains chair, patient weight capacity up to
and including 300 pounds
K0879
F3
Power wheelchair, group 4 heavy duty, single power option, sling/solid seat/back, patient weight
capacity 301 to 450 pounds
K0880
F3
Power wheelchair, group 4 very heavy duty, single power option, sling/solid seat/back, patient weight
451 to 600 pounds
Multiple Power Options
Covered if all the coverage criteria (1-3, 10-13) for a PWC are met and if:
1. The Group 4 no power option criteria are met, and
2. The Group 2 Multiple Power Options are met.
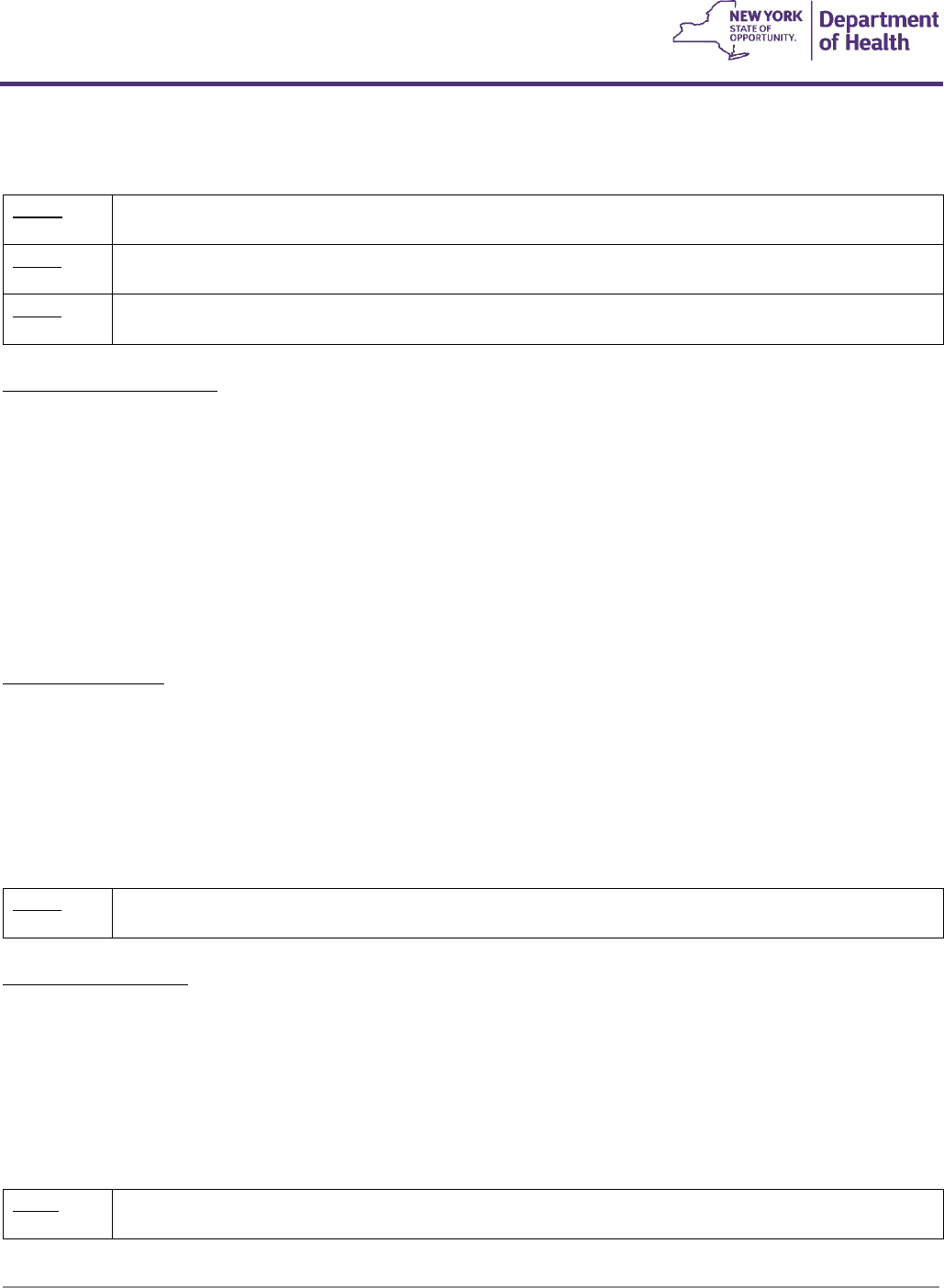
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
46
Features: In addition to Group 4 standard features, expandable controller at initial issue, capable of upgrade to alternative
control devices, accommodates more than one powered seating system at a time on the base, and accommodates
ventilators.
K0884
F3
Power wheelchair, group 4 standard, multiple power option, sling/solid seat/back, patient weight
capacity up to and including 300 pounds
K0885
F3
Power wheelchair, group 4 standard, multiple power option, captains chair, patient weight capacity up
to and including 300 pounds
K0886
F3
Power wheelchair, group 4 heavy duty, multiple power option, sling/solid seat/back, patient weight
capacity 301 to 450 pounds
Group 5 Power wheelchairs
Features: Patient weight capacity pediatric (125 pounds or less), length less than or equal to 48 inches, width less than
or equal to 28 inches, minimum top end speed-flat 4 mph, minimum range 4 mph, minimum range 12 miles, minimum
obstacle climb 60 mm, dynamic stability incline 9 degrees, crash testing passed, fatigue cycle test 200,000 cycles, drop
test 6,666 cycles, standard integrated or remote proportional control, seat width minimum of 5 one-inch options, seat
depth minimum 3 one-inch options, seat height adjustment requirements greater than or equal to 3 inches, back height
adjustment requirements minimum of 3 options, seat to back angle range of adjustment - minimum of 12 degrees, drive
wheel suspension to reduce vibration, expandable controller at initial issue, capable of upgrade to alternative control
devices, accommodates powered seating options, accommodates seating and positioning items (e.g. seat and back
cushions, headrests, lateral trunk supports, lateral hip supports, medial thigh supports), adjustability for growth (minimum
of 3 inches for width, depth, and back height adjustment).
Single Power Option
Covered if the coverage criteria (1-3, 10-13) for a PWC are met, and
1. The member is expected to grow in height, and
2. The Group 2 Single Power Option criteria are met.
Features: In addition to Group 5 standard features, may accommodate non-powered options and seating systems,
allows only one power option on the base at a time.
K0890
F3
Power wheelchair, group 5 pediatric, single power option, sling/solid seat/back, patient weight capacity
up to and including 125 pounds
Multiple Power Options
Covered if the coverage criteria (1-3, 10-13) for a PWC are met, and
1. The member is expected to grow in height, and
2. The Group 2 Multiple Power Options are met.
Features: In addition to Group 5 standard features, allows more than one power option on the base at a time, and
accommodates ventilators.
K0891
F3
Power wheelchair, group 5 pediatric, multiple power option, sling/solid seat/back, patient weight
capacity up to and including 125 pounds
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
47
Group 6 PWC Miscellaneous Code
K0898
F3
Power wheelchair, not otherwise classified
V. Seating and Positioning Components (SPC)/ Wheeled Mobility Accessories
SPC are covered when:
- Criterion 1, 2 and 3 (below) are met, and
- The coverage criteria listed under the specific SPC procedural code is met.
1. The member has met the criteria for Wheeled Mobility Equipment (WME), and
2. The SPC meets the quality standards and coding definitions specified in the Definitions Section. A Product
Classification List with products which have received a Medicare coding verification can be found on the
Medicare Pricing, Data Analysis and Coding (MPDAC) web site. If a coding assignment is not available
from MPDAC, the vendor must exercise due diligence in assigning an appropriate code. The Medicaid
program reserves the right to review any and all coding assignments by vendors and the MPDAC based
on submitted and published product specifications and other relevant information.
3. The primary and back-up WME bases accommodate the SPC.
4. See code E0950 for Upper extremity support systems (UESS).
5. If foam-in-place or other material is used to fit a substantially prefabricated cushion to an individual
member, the cushion must be billed as a customized cushion, not custom fabricated.
General Guidelines
- The code for a seat or back cushion includes any rigid or semi-rigid base or posterior panel, respectively, which is
an integral part of the cushion.
- Payment for all wheelchair seats, backs and accessory codes includes fixed, adjustable, removable and/or quick-
release mounting hardware, if hardware is applicable to the item. If the code description includes any type of
mounting or adjustable hardware, no additional payment for this hardware will be made.
- The swing away, retractable, or flip-down hardware upgrade code (E1028) may only be billed in addition to the
codes for a headrest, lateral trunk supports, hip supports, medial thigh supports, calf supports,
abductors/pommels, foot supports, and replacement joystick mounts when medically justified. It must not be billed
in addition to the codes for shoulder harness/straps or chest straps, wheelchair seat cushions or back cushions, or
new power wheelchair joystick mounts. If the swing away or flip-down hardware is being added to a new accessory
(e.g. headrest, medial knee support or laterals), it will be reimbursed at invoice cost in addition to the MRA for the
accessory component.
- May be included with new WME or billed separately under the following conditions:
1. Refer to the SPC Coverage Criteria for information concerning coverage of the following: general use, skin
protection, and positioning, powered and custom-made components.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
48
2. A POV or PWC with Captain's Chair seating is not appropriate for a member who needs a separate SPC.
3. If a member needs a seat and/or back cushion but does not meet coverage criteria for a skin protection
and/or positioning cushion, it is appropriate to provide a Captain's Chair seat (if the code exists) rather
than a sling/solid seat/back and a separate general use seat and/or back cushion.
4. A general use seat and/or back cushion provided with a PWC with a sling/solid seat/back will be
considered equivalent to a power wheelchair with Captain's Chair and will be coded and priced
accordingly if that code exists.
5. If a member’s weight combined with the weight of seating and positioning accessories can be
accommodated by WME with a lower weight capacity than the wheelchair that is requested or provided,
approval or payment will be based on the appropriate HCPCS code that meets the medical need.
- Wheeled mobility accessories that are included in new equipment (as indicated in the Manual and Powered
Mobility sections) are reimbursable ONLY as replacement parts outside of warranty and are not to be billed with a
new wheelchair. For new wheeled mobility devices, use accessory codes ONLY when included accessories do not
meet a specific medical need.
- Coverage of flat free, zero pressure and foam filled tires is limited to members who are independent in mobility or
whose medical conditions indicate such tires.
Codes, Descriptions, and Code Specific Criteria
E0944
F7
#Pelvic belt/harness/boot (limited to wheelchair 4-point padded belt)
E0950
F3
#Wheelchair accessory, tray, each (upper extremity support surface for positioning only)
- Covered when the medical need for positioning in a wheelchair cannot be met with
less costly alternatives such as any combination of a safety belt, pelvic strap, harness,
prompts, armrest modifications, recline, tilt in space or other existing or potential
seating or wheelchair features.
- The MRA for trays/upper extremity supports includes any size/dimension, all
mounting hardware/accessories, cut outs, and rims.
- UESS dimensions should not exceed the positioning length of the forearms (e.g., 12-
15”).
- UESS and related accessories are not covered when used solely for activities of daily
living.
- Padding and positioning blocks are separately billable using HCPCS code K0108.
E0951
F6
#Heel loop/holder, any type, with or without ankle strap, each
E0952
F6
#Toe loop/holder, any type, each
E0953
F5
#Wheelchair accessory, lateral thigh or knee support, any type including fixed mounting
hardware, each
E0954
F5
#Wheelchair accessory, foot box, any type, includes attachment and mounting hardware,
each foot
(Includes padding. If dispensing a double-leg or full size footbox, obtain an
authorization for quantity of 2.)
E0955
F5
#Wheelchair accessory, headrest, cushioned, any type, including fixed mounting hardware,
each
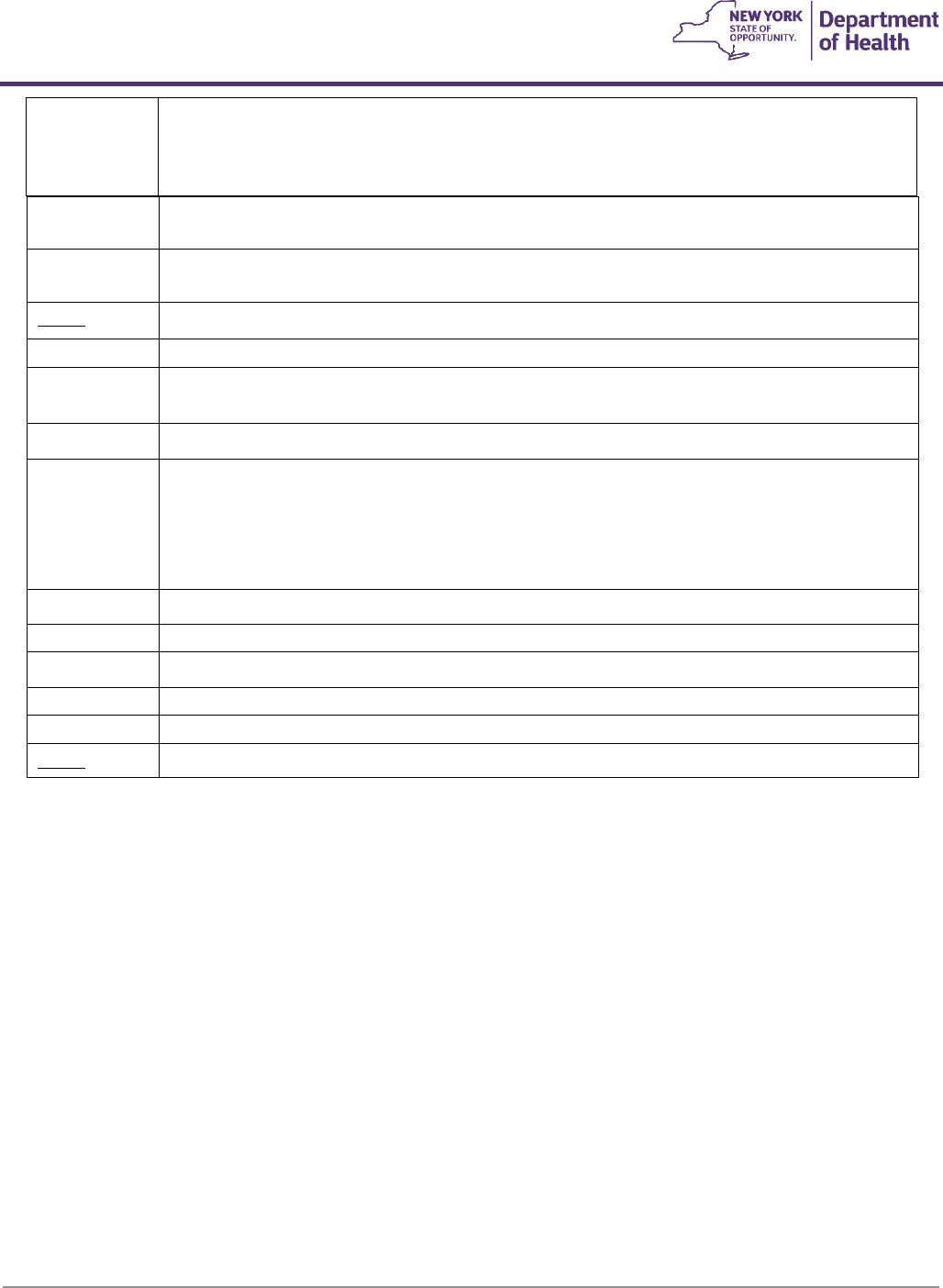
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
49
E0956
F5
#Wheelchair accessory, lateral trunk or hip support, any type, including fixed mounting
hardware, each (up to 4 supports/prompts)
E0957
F5
#Wheelchair accessory, medial thigh support, any type, including fixed mounting hardware,
each
E0958
F5
Manual wheelchair accessory, one-arm drive attachment, each
E0959
F5
#Manual wheelchair accessory, adapter for amputee, each
E0960
F7
#Wheelchair accessory, shoulder harness/straps or chest strap, including any type mounting
hardware
(includes padding and strap guides)
E0961
F5
#Manual wheelchair accessory, wheel lock brake extension (handle), each
E0966
F5
#Manual wheelchair accessory, headrest extension, each
Covered when the member has a covered manual tilt-in space, manual semi or fully reclining
back, or power tilt and/or recline power seating system or needs additional head support. The
code for a headrest includes any type of cushioned headrest, fixed, removable, or non-
removable hardware.
E0967
F3
#Manual wheelchair accessory, hand rim with projections, any type, replacement only, each
E0971
F7
#Manual wheelchair accessory, anti-tipping device, each
E0973
F4
#Wheelchair accessory, adjustable height, detachable armrest, complete assembly, each
E0974
F5
#Manual wheelchair accessory, anti-rollback device, each
E0978
F7
#Wheelchair accessory, positioning belt/safety belt/pelvic strap, each (includes padding)
E0986
F3
Manual wheelchair accessory, push rim activated power assist system
Power Assist System
A push-rim activated power assist device (E0986) for a manual wheelchair is covered if the coverage criteria (1-3, 10-13)
for a PWC are met; and documentation includes:
1. A thorough upper extremity assessment including but not limited to ROM, strength testing, tone
assessment, and evaluation of gross and fine motor skills and hand strength.
2. Description of a detailed, successful trial in a variety of situations in all customary environments (or
simulations of customary environments) showing a clear regard for safety as well as awareness of others,
the environment, and objects/barriers. Include ability to navigate indoor/outdoor, up/down ramps, tight
spaces, backing up, etc.
3. A well-defined medical necessity justification for this item versus a power wheelchair.
4. Confirmation that the member has no excessive non purposeful spasticity/extraneous movements.
5. Confirmation that the member has no history of seizures or there is confirmed successful medical
management of seizures.
Please note: An additional back-up manual wheelchair, when primary mobility is a manual wheelchair with a power
assist system, is not considered a medical necessity. In addition, when primary mobility is a power wheelchair, there is
no medical necessity for a back-up manual wheelchair to include power assisted propulsion.
Covered when the member has a covered manual tilt-in-space, manual semi or fully reclining
back, or power tilt and/or recline power seating system or needs additional head support. The
code for a headrest includes any type of cushioned headrest, fixed, removable, or non-
removable hardware.
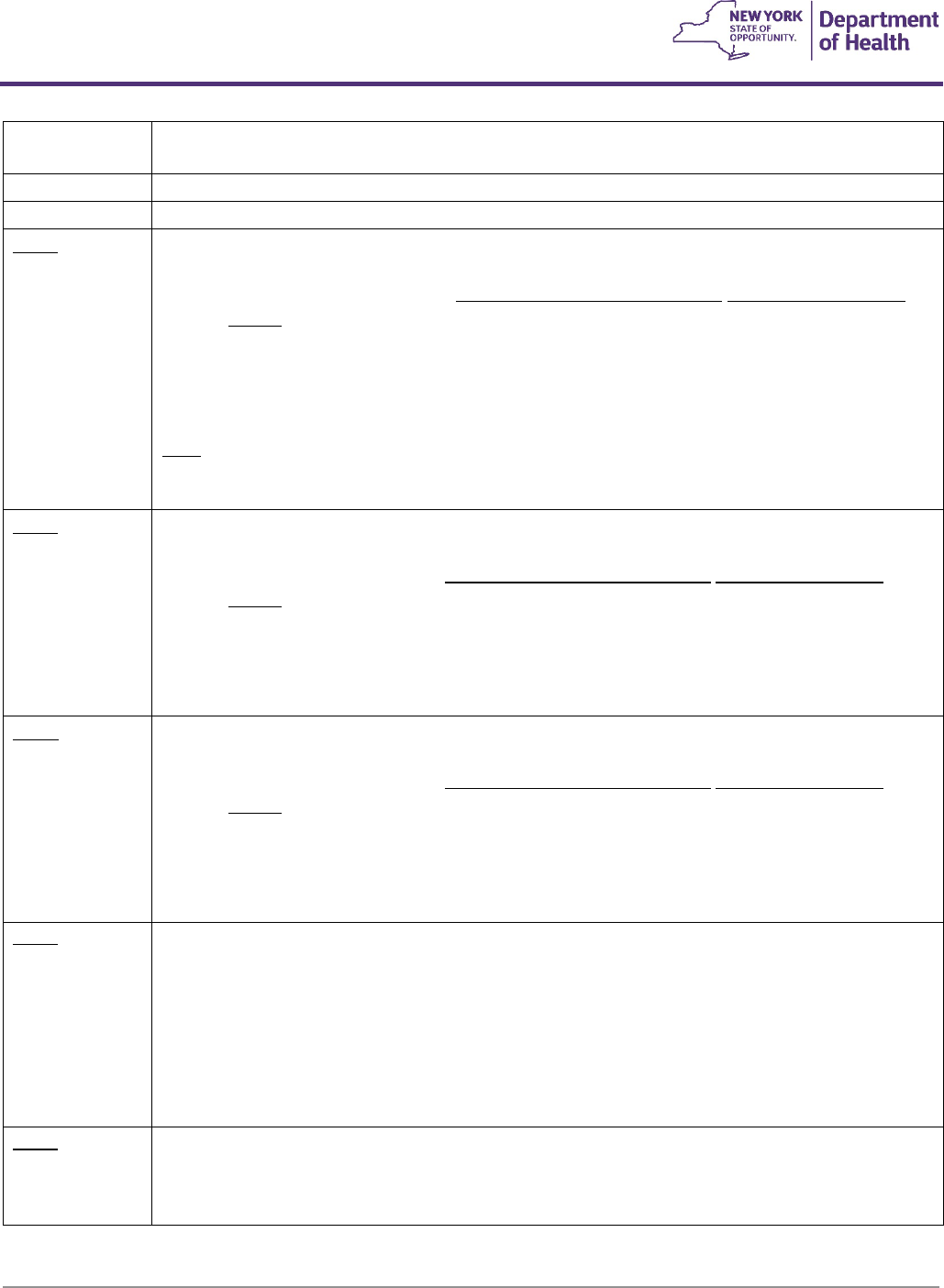
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
50
E0990
F5
‘-RR’
#Wheelchair accessory, elevating leg rest, complete assembly, each
E0992
F6
#Manual wheelchair accessory, solid seat insert
E0995
F6
#Wheelchair accessory, calf rest/pad, replacement only, each
E1002
F3
Wheelchair accessory, power seating system, tilt only
Covered when:
- The member meets criterion 1-3 of the Seating and Positioning Components coverage
criteria, and
- The member meets the coverage criteria for manual tilt, and
- The member has the mental and physical ability to safely and independently operate the
power tilt-in-space that is provided.
Note
: A combination power tilt-in-space and recline option is covered when the member meets
the coverage criteria for both components and, when provided alone, one function will not meet
their seating and positioning needs.
E1003
F3
Wheelchair accessory, power seating system, recline only, without shear reduction
Covered when:
- The member meets criteria 1-3 of the Seating and Positioning component coverage
criteria, and
- The member meets the above criteria for manual recline, and
- The member has the mental and physical ability to operate the provided power recline
feature safely and independently.
E1004
F3
Wheelchair accessory, power seating system, recline only, with mechanical shear reduction
Covered when:
- The member meets criteria 1-3 of the Seating and Positioning component coverage
criteria, and
- The member meets the above criteria for manual recline, and
- The member has the mental and physical ability to operate the provided power recline
feature safely and independently.
E1005
F3
Wheelchair accessory, power seating system, recline only, with power shear reduction Covered
when:
- The member meets criteria 1-3 of the Seating and Positioning component coverage
criteria, and
- The member meets the above criteria for manual recline, and
- The member has the mental and physical ability to safely and independently operate the
power recline feature that is provided.
E1006
F3
Wheelchair accessory, power seating system, combination tilt and recline, without shear reduction
A combination of power tilt-in-space along with power recline option is covered when the
member meets the coverage criteria for both components and when provided alone, one
function will not meet their seating and positioning needs.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
51
E1007
F3
Wheelchair accessory, power seating system, combination tilt and recline, with mechanical shear
reduction
A combination of power tilt-in-space along with power recline option is covered when the
member meets the coverage criteria for both components and when provided alone, one
function will not meet their seating and positioning needs.
E1008
F3
Wheelchair accessory, power seating system, combination tilt and recline, with power shear
reduction
A combination of power tilt-in-space along with power recline option is covered when the
member meets the coverage criteria for both components and when provided alone, one
function will not meet their seating and positioning needs.
E1009
F3
Wheelchair accessory, addition to power seating system, mechanically linked leg elevation system,
including push rod and leg rest, each
E1010
F3
Wheelchair Accessory, addition to power seating system, power leg elevation system, including
leg rest, pair
E1011
F3
Modification to pediatric size wheelchair, width adjustment package (not to be dispensed with
initial chair)
E1012
F3
Wheelchair accessory, addition to power seating system, center mount power elevating leg
rest/platform, complete system, any type, each
E1014
F3
‘-RR’
#Reclining back, addition to pediatric size wheelchair
E1020
F3
#Residual limb support system for wheelchair, any type (with adjustable drop hooks)
E1028
F3
Wheelchair accessory, manual swing away, retractable or removable mounting hardware for
joystick, other control interface or positioning accessory
E1029
F3
Wheelchair accessory, ventilator tray, fixed
E1225
F3
Wheelchair accessory, manual semi-reclining back, (recline greater
than 15 degrees, but less than 80 degrees), each Covered when:
The member meets criteria 1-3 of the Seating and Positioning component coverage criteria, and
4. The member has a plan of care that requires a recline position to complete Mobility Related
Activities of Daily Living (MRADLs), and
5. The member has positioning needs that cannot be met by upright or fixed angle chair, or
6. The member’s postural control requires a recline feature, or
7. The member utilizes intermittent catheterization for bladder management and is unable to
independently transfer from the wheelchair to the bed.
E1226
F3
‘-RR’
#Wheelchair accessory, manual fully reclining back, (recline greater than 80 degrees), each
Covered when:
The member meets criteria 1-3 of the Seating and Positioning component coverage criteria, and
4. The member has a plan of care that requires a recline position to complete Mobility Related
Activities of Daily Living (MRADLs), and
5. The member has positioning needs that cannot be met by upright or fixed angle chair, or
6. The member’s postural control requires a recline feature, or
7. The member utilizes intermittent catheterization for bladder management and is unable to
independently transfer from the wheelchair to the bed.
E1228
F6
Special back height for wheelchair
E1298
F3
Special wheelchair seat depth and/or width, by construction
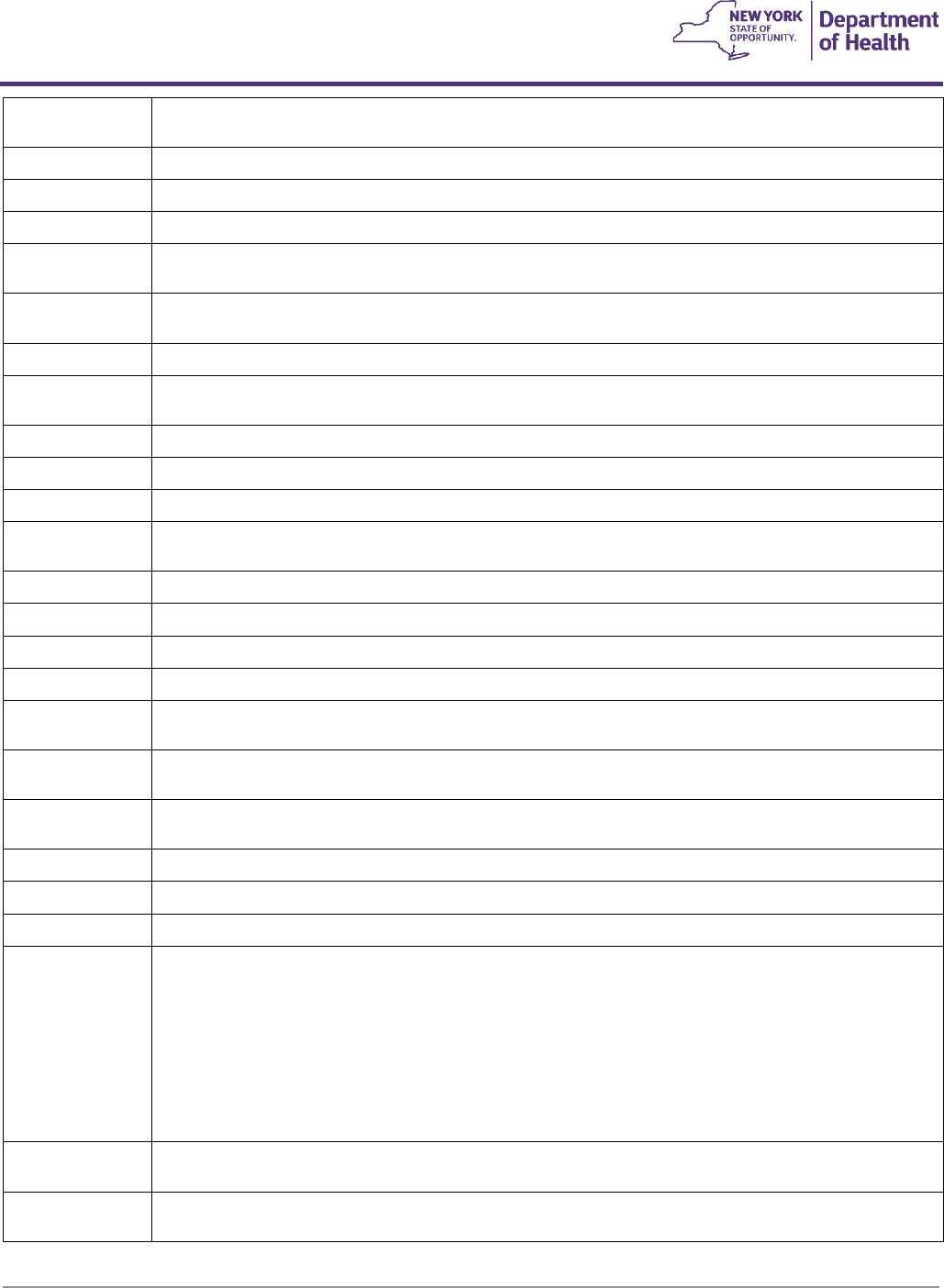
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
52
E2201
F3
#Manual wheelchair accessory, nonstandard seat frame, width greater than or equal to 20 inches
and less than 24 inches
E2202
F3
#Manual wheelchair accessory, nonstandard seat frame width, 2427 inches
E2203
F3
#Manual wheelchair accessory, nonstandard seat frame depth, 20 to less than 22 inches
E2204
F3
#Manual wheelchair accessory, nonstandard seat frame depth, 22 to 25 inches
E2205
F3
# Manual wheelchair accessory, hand rim without projections (includes ergonomic or contoured),
any type, replacement only, each
E2206
F7
#Manual wheelchair accessory, wheel lock assembly, complete, replacement only, each (any type
of brakes)
E2207
F6
#Wheelchair accessory, crutch and cane holder, each
E2209
F6
#Arm trough, with or without hand support, each (includes non- angle adjustable/articulating
hardware and straps)
E2210
F6
Wheelchair accessory, bearings, any type, replacement only, each
E2211
F7
#Manual wheelchair accessory, pneumatic propulsion tire, any size, each
E2212
F7
#Manual wheelchair accessory, tube for pneumatic propulsion tire, any size, each
E2213
F6
#Manual wheelchair accessory, insert for pneumatic propulsion tire (removable), any type, any
size, each
E2214
F7
#Manual wheelchair accessory, pneumatic caster tire, any size, each
E2215
F7
#Manual wheelchair accessory, tube for pneumatic caster tire, any size, each
E2218
F6
#Manual wheelchair accessory, foam propulsion tire, any size, each
E2219
F6
#Manual wheelchair accessory, semi pneumatic foam caster tire, any size, each
E2220
F7
#Manual wheelchair accessory, solid (rubber/plastic) propulsion tire, any size, replacement only,
each
E2221
F7
#Manual wheelchair accessory, solid (rubber/plastic) caster tire
(removable), any size, replacement only, each
E2222
F6
#Manual wheelchair accessory, solid (rubber/plastic) caster tire with integrated wheel, any size,
replacement only, each
E2224
F6
#Manual wheelchair accessory, propulsion wheel excludes tire, any size, replacement only, each
E2225
F6
#Manual wheelchair accessory, caster wheel excludes tire, any size, replacement only, each
E2226
F6
#Manual wheelchair accessory, caster fork, any size, replacement only, each
E2231
F3
#Manual wheelchair accessory, solid seat support base (replaces sling seat), includes any type
mounting hardware
A solid seat support base/insert with mounting hardware may be billed separately when added to
a folding manual wheelchair or when replacement is needed (When replacing a solid seat support
base on a rigid manual wheelchair or power wheelchair use the chairs base code and the RB
modifier)
NOTE:
Because payment for power wheelchairs, rigid manual wheelchairs, and pediatric seating
for any wheelchair includes a solid seat support base/insert, it may not be billed separately.
E2291
F3
#Back, planar, for pediatric size wheelchair including fixed attaching hardware
Pediatric sized chairs have seat depths and widths less than 16 inches
E2292
F3
#Seat, planar, for pediatric size wheelchair including fixed attaching hardware
Pediatric sized chairs have seat depths and widths less than 16 inches

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
53
E2298
F3
Complex rehabilitative power wheelchair accessory, power seat elevation system, any type
Coverage Criteria:
- E2298 can only be used on K0835- K0898 complex power wheelchair bases.
- In rare circumstances, if power seat elevation needs to be added to a non-complex
rehabilitative power wheelchair K0822-K0829 (no power option), K0108 should be used.
Invoice is required for cost+51% pricing, however, cost+51% pricing will not exceed the
fee listed on the DMEPOS Fee Schedule for E2298.
- The member meets criterion 1-3 of the Powered Mobility Device coverage criteria, and
- The member has demonstrated the mental and physical abilities to safely and
independently operate the power seat function that is requested; AND
- Selection of the power seat elevator system is not based solely on caregiver convenience
but on medical need of the member.
- All less costly options have been considered including reasonable
adaptation/modification of the member’s environment. Examples of reasonable
adaptation/modification include, but are not limited to, adjustable height bed/table,
dresser/closet re-organization, refrigerator re-organization, or installation of a grab bar
for transfer assistance; AND (one of the following)
• the member is not able to transfer independently without power height adjustment,
OR
• power seat elevation allows the member to independently perform MRADLs that
cannot be performed independently without the addition of power seat elevation.
E2301
F3
Wheelchair accessory, power standing system, any type (includes all medically necessary supports
and accessories)
Power Standing System
General Criteria (must meet all the following):
1. Wheelchair evaluation, written LOMN, and recommendations are made by a physician, physical or
occupational therapist that has experience in complex rehab wheelchair prescription.
2. Member has a set, recommended standing program prescribed by a physician.
3. Member does not have a caregiver available for all waking hours.
4. Member must have adequate cognition to know when to use the power standing feature, how to operate it,
and good safety awareness.
5. Member cannot access a static home standing system, when necessary, with or without assistance.
Documentation must include that the member has tried more cost-effective alternatives, and still requires a
power wheelchair with power standing feature.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
54
6. The member does not have orthostatic hypotension, postural tachycardia syndrome, osteogenesis
imperfecta (or similar diagnoses), or hip or knee flexion contractures of more than 45°.
7. Provision of the requested power standing feature would decrease the necessity for caregivers.
Guidelines
When requesting a standing power wheelchair, the following guidelines should be considered:
- Member does not have ROM limitations, tonal abnormalities, or strength limitations that would make ADLs
unsafe to complete in customary locations in the home and/or community (ADLs include dining, personal
hygiene tasks and activities specified in a medical treatment plan).
- Member meets all established criteria for power seat elevation (E2300) and static home standing systems
(E0637-E0641).
- Member is independent with managing associated chest and knee supports.
- Documented history of bone loss (limited to adults).
- The alignment of the member’s lower extremities is such that they can tolerate a standing or upright position
and the member has recently trialed and effectively utilized a static stander with no history of adverse
physiological responses.
- The member has evidence-based reasons and documented clinical justification for why a power assisted
standing component will meet the member’s medical needs and why a
- static stander, tilt table, or other therapeutic interventions cannot meet those medical needs.
- Member is at high risk for lower extremity contractures with thorough explanation of why they cannot be
appropriately managed by other treatment modalities (i.e. stretching, active therapy, orthotics, home
programs, etc.) or use of a static stander.
- The member does not have, and it is not anticipated they will require, a walker or gait trainer.
Documentation requirements:
1. Fiscal order from a qualified provider (physician, nurse practitioner, physician’s assistant) for a power standing
component on a power wheelchair.
2. Letter of medical necessity (LOMN) that includes:
a) Comprehensive history and physical exam by a qualified provider.
b) Summary of the existing medical condition, age at diagnosis, prognosis, and co-morbid conditions.
c) Wheelchair evaluation, performed by a physiatrist, physical or occupational therapist that has experience
in complex rehab wheelchair prescription.
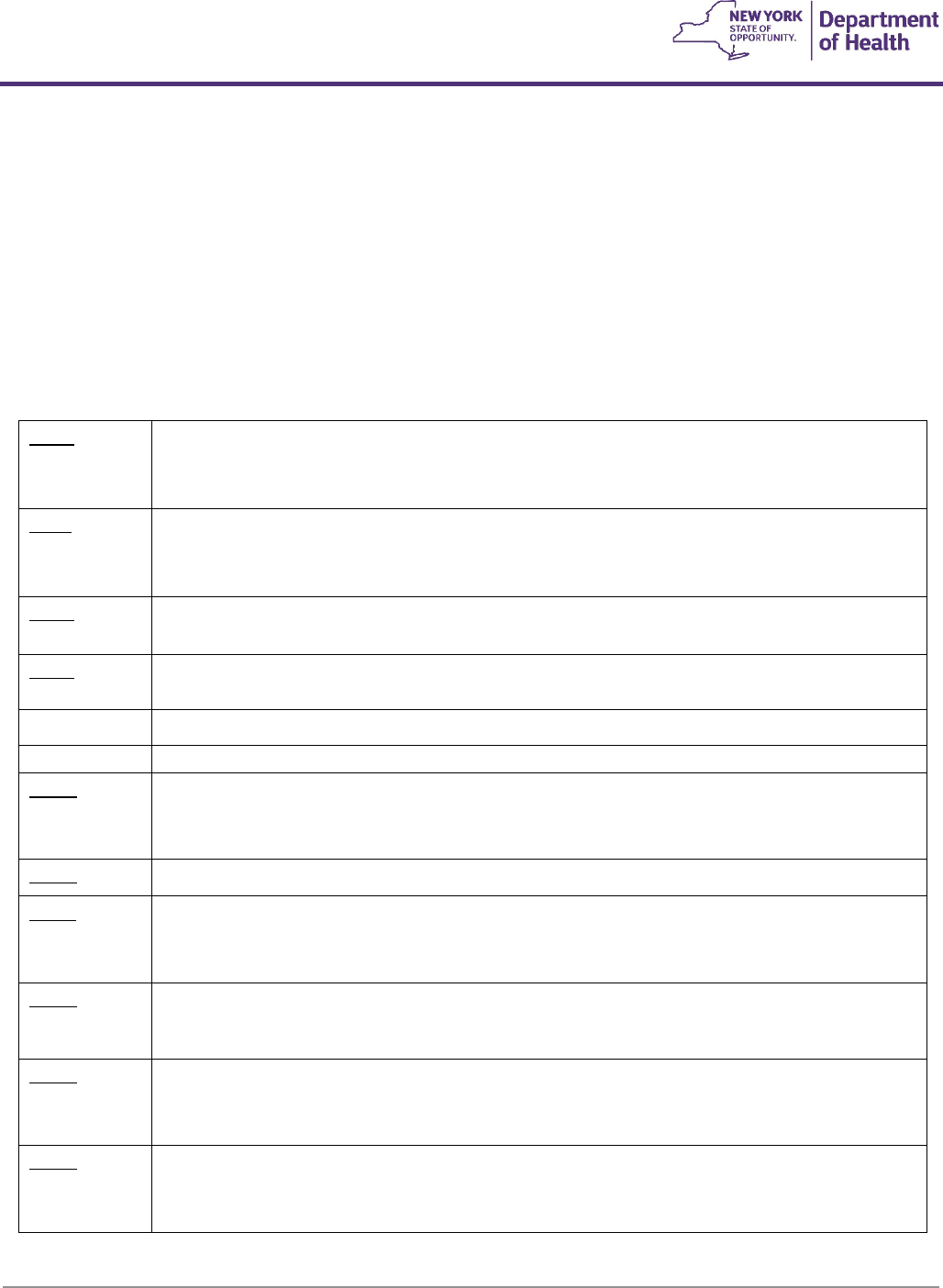
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
55
d) Thorough description of the member’s functional and physical assessment including strength, range of
motion (ROM), tone, sensation, balance, ADLs, and functional status.
e) Documentation of trial of less costly alternatives (include make and model of alternatives tried as well as
the length of the trial and results with each alternative) and why they do not meet the members current
needs.
f) Home therapy plan outlining the planned use of the requested standing feature.
g) Documentation regarding the level of caregiver assistance available/needed on a daily basis, including a
tentative schedule.
h) Itemized list of all current DME (including, but not limited to, standers, wheelchairs, any transfer devices,
etc.) owned, rented, or borrowed.
E2310
F3
Power wheelchair accessory, electronic connection between wheelchair controller and one
power seating system motor, including all related electronics, indicator feature, mechanical
function selection switch, and fixed mounting hardware
E2311
F3
Power wheelchair accessory, electronic connection between wheelchair controller and two or
more power seating system motors, including all related electronics, indicator feature,
mechanical function selection switch, and fixed mounting hardware
E2312
F6
Power wheelchair accessory, hand or chin control interface, mini proportional remote joystick,
proportional, including fixed mounting hardware
E2313
F6
Power wheelchair accessory, harness for upgrade to expandable controller, including all
fasteners, connectors and mounting hardware, each
E2323
F5
#Power wheelchair accessory, specialty joystick handle for hand control interface, prefabricated
E2324
F6
#Power wheelchair accessory, chin cup for chin control interface
E2325
F3
Power wheelchair accessory, sip and puff interface, nonproportional, including all related
electronics, mechanical stop switch, and manual swing away mounting hardware
(includes
enhanced visual display)
E2326
F3
Power wheelchair accessory, breath tube kit for sip and puff interface
E2327
F3
Power wheelchair accessory, head control interface, mechanical, proportional, including all
related electronics, mechanical direction change switch, and fixed mounting hardware
(includes
enhanced visual display)
E2328
F3
Power wheelchair accessory, head control or extremity control interface, electronic,
proportional, including all related electronics and fixed mounting hardware
(includes enhanced
visual display)
E2329
F3
Power wheelchair accessory, head control interface, contact switch mechanism,
nonproportional, including all related electronics, mechanical stop switch, mechanical direction
change switch, head array, and fixed mounting hardware
(includes enhanced visual display)
E2330
F3
Power wheelchair accessory, head control interface, proximity switch mechanism,
nonproportional, including all related electronics, mechanical stop switch, mechanical direction
change switch, head array, and fixed mounting hardware
(includes enhanced visual display)
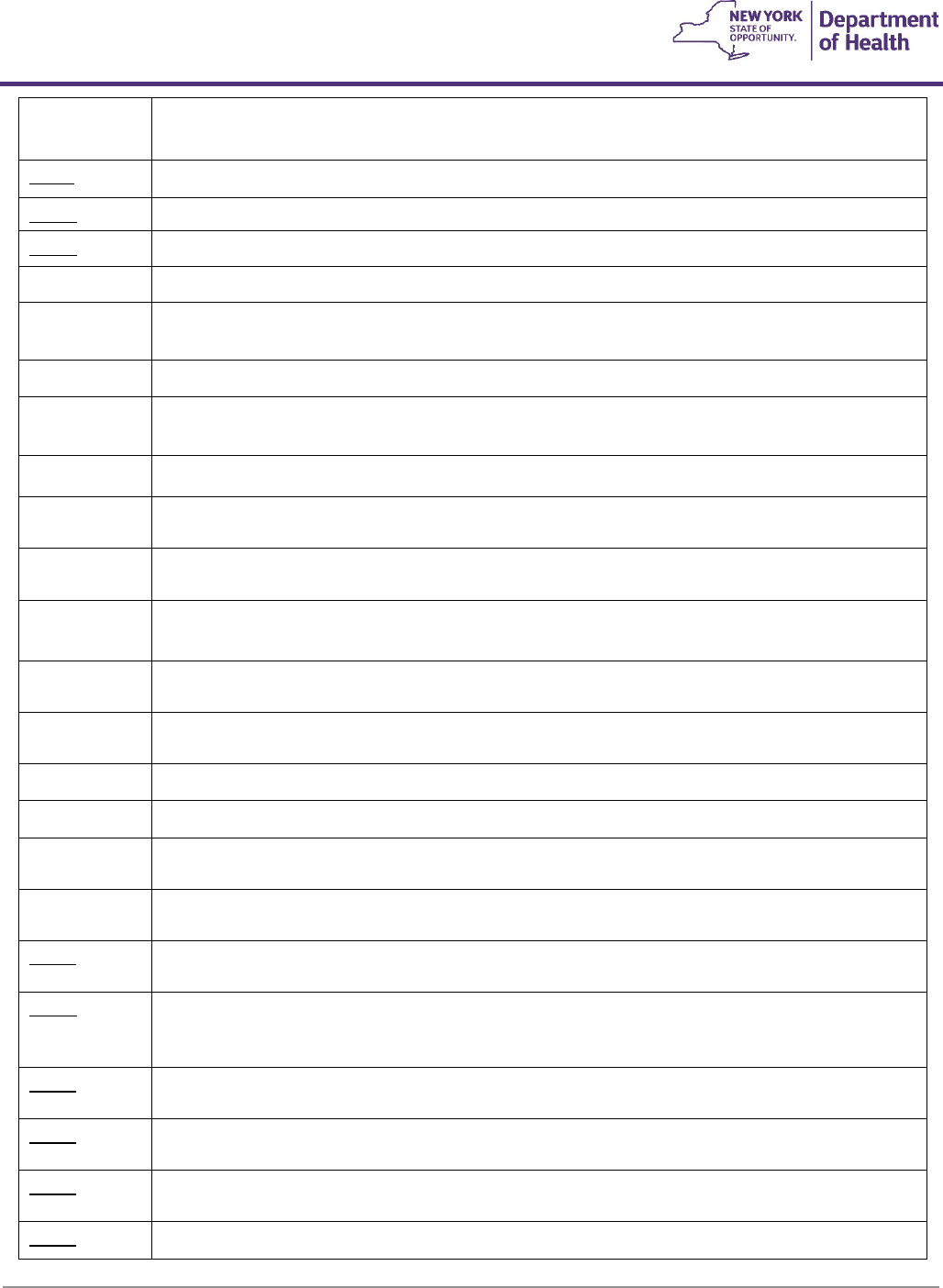
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
56
E2340
F3
#Power wheelchair accessory, nonstandard seat frame width, 20-
23 inches
(for 21”-23” only, 20” included in base)
E2341
F3
Power wheelchair accessory, nonstandard seat frame width, 24-27 inches
E2342
F3
Power wheelchair accessory, nonstandard seat frame depth, 20-21 inches
E2343
F3
Power wheelchair accessory, nonstandard seat frame depth, 22-25 inches
E2358
F6
Power Wheelchair accessory, Group 34 non-sealed lead acid battery, each (replacement only)
E2359
F6
Power Wheelchair accessory, Group 34 sealed lead acid battery, each (e.g. Gel Cell, Absorbed
glassmat)
(replacement only)
E2360
F6
Power wheelchair accessory, 22 NF non-sealed lead acid battery, each (replacement only)
E2361
F6
Power wheelchair accessory, 22 NF sealed lead acid battery, each, (e.g. gel cell, absorbed glass
mat)
(replacement only)
E2362
F6
Power wheelchair accessory, group 24 non-sealed lead acid battery, each (replacement only)
E2363
F6
Power wheelchair accessory, group 24 sealed lead acid battery, each (e.g. gel cell, absorbed
glassmat) (replacement only)
E2364
F6
Power wheelchair accessory, U-1 non-sealed lead acid battery, each (replacement only)
E2365
F6
Power wheelchair accessory, U-1 sealed lead acid battery, each (e.g. gel cell, absorbed glassmat)
(replacement only)
E2366
F3
#Power wheelchair accessory, battery charger, single mode, for use with only one battery type,
sealed or non-sealed, each (replacement only)
E2367
F3
#Power wheelchair accessory, battery charger, dual mode, for use with either battery type,
sealed or non-sealed, each (replacement only)
E2368
F3
#Power wheelchair component, drive wheel motor, replacement only
E2369
F3
#Power wheelchair component, drive wheel gear box, replacement only
E2370
F3
#Power wheelchair component, drive wheel motor and gear box combination, replacement
only
E2371
F7
#Power wheelchair accessory, group 27 sealed lead acid battery,
(e.g. gel cell, absorbed glassmat), each (replacement only)
E2373
F6
Power wheelchair accessory, hand or chin control interface, compact remote joystick,
proportional, including fixed mounting hardware
E2374
F6
Power wheelchair accessory, hand or chin control interface, standard remote joystick (not
including controller), proportional, including all related electronics and fixed mounting
hardware, replacement only
E2375
F6
Power wheelchair accessory, non-expandable controller, including all related electronics and
mounting hardware, replacement only
E2376
F6
Power wheelchair accessory, expandable controller, including all related electronics and
mounting hardware, replacement only (includes harness)
E2377
F2
Power wheelchair accessory, expandable controller, including all related electronics and
mounting hardware, upgrade provided at initial issue
E2378
F6
Power wheelchair component, actuator, replacement only
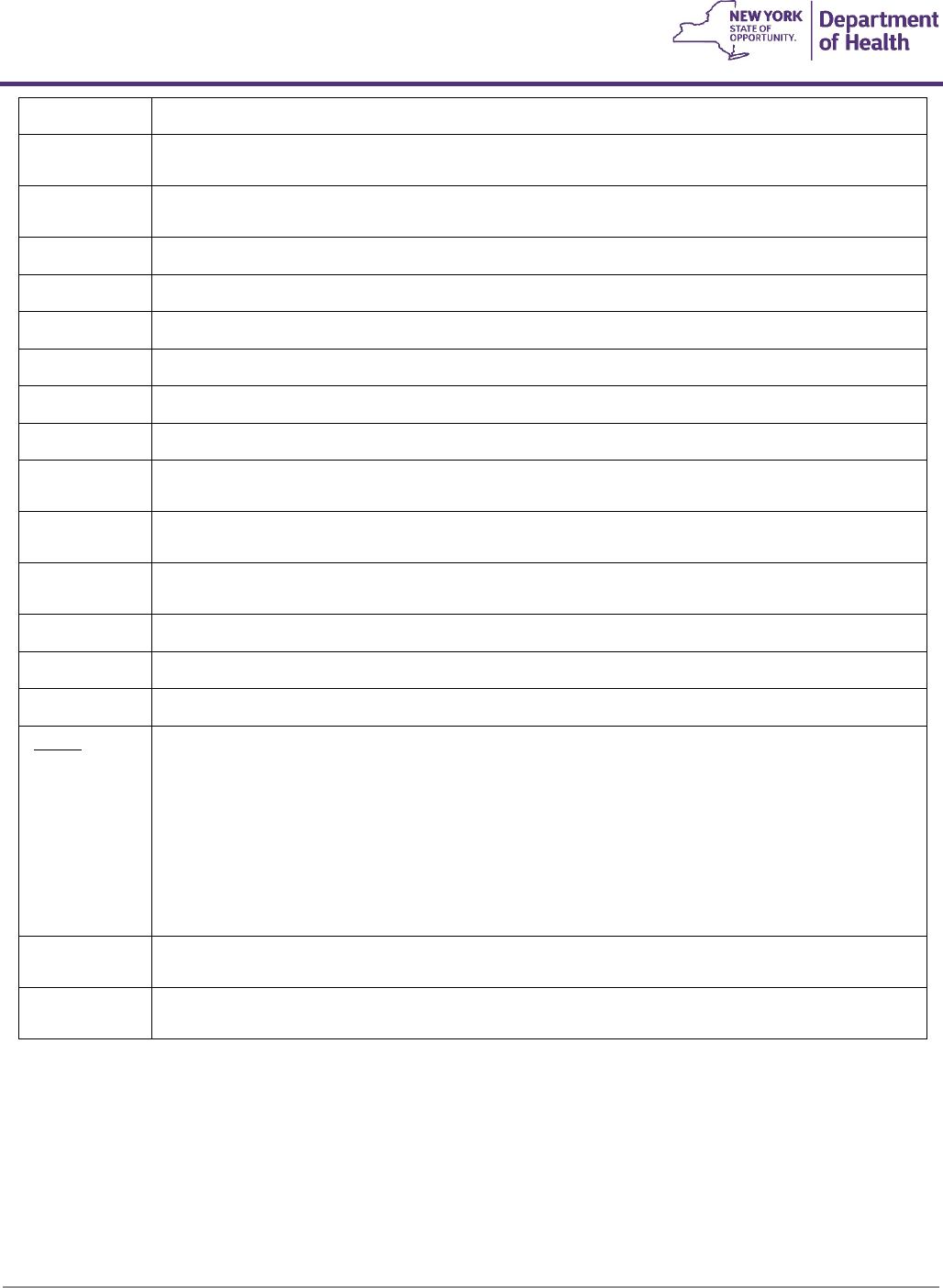
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
57
E2381
F6
#Power wheelchair accessory, pneumatic drive wheel tire, any size, replacement only, each
E2382
F6
#Power wheelchair accessory, tube for pneumatic drive wheel tire, any size, replacement only,
each
E2383
F6
#Power wheelchair accessory, insert for pneumatic drive wheel tire
(removable), any type, any size, replacement only, each
E2384
F6
#Power wheelchair accessory, pneumatic caster tire, any size, replacement only, each
E2385
F6
#Power wheelchair accessory, tube for pneumatic caster tire, any size, replacement only, each
E2386
F6
#Power wheelchair accessory, foam filled drive wheel tire, any size, replacement only, each
E2387
F6
#Power wheelchair accessory, foam filled caster tire, any size, replacement only, each
E2388
F6
#Power wheelchair accessory, foam drive wheel tire, any size, replacement only, each
E2389
F6
#Power wheelchair accessory, foam caster tire, any size, replacement only, each
E2390
F6
#Power wheelchair accessory, solid (rubber/plastic) drive wheel tire, any size, replacement only,
each
E2391
F6
#Power wheelchair accessory, solid (rubber/plastic) caster tire
(removable), any size, replacement only, each
E2392
F6
#Power wheelchair accessory, solid (rubber/plastic) caster tire with integrated wheel, any size,
replacement only, each
E2394
F6
#Power wheelchair accessory, drive wheel excludes tire, any size, replacement only, each
E2395
F6
#Power wheelchair accessory, caster wheel excludes tire, any size, replacement only, each
E2396
F6
#Power wheelchair accessory, caster fork, any size, replacement only, each
E2398
F3
Wheelchair accessory, dynamic positioning hardware for back
Covered when:
1. the member has moderate to severe hypertonicity, or
2. has a documented history of rocking, shaking or other movements related to
behavior and/or increased muscle tone, and
3. there is documented evidence of frequent backrest, back canes, or wheelchair frame
repairs as a result of the member’s behaviors and tone.
E2601
F5
#General use wheelchair seat cushion, width less than 22 inches, any depth
A general use seat cushion (E2601) is covered when 1, 2 and 3 of the SPC guidelines are met.
E2602
F5
#General use wheelchair seat cushion, width 22 inches or greater, any depth
See coverage criteria for E2601
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
58
E2603
F5
#Skin protection wheelchair seat cushion, width less than 22 inches, any depth
A skin protection seat cushion (E2603) is covered when 1, 2 and 3 of the SPC guidelines are met
and that member has one of the following diagnoses/conditions:
a) A current pressure ulcer or past history of a pressure ulcer on the area of contact
with the seating surface (See Appendix A); or
b) Absent or impaired sensation in the area of contact with the seating surface due to
but not limited to one of the following diagnoses: spinal cord injury resulting in
quadriplegia or paraplegia, other spinal cord disease, multiple sclerosis, other
demyelinating disease , cerebral palsy, anterior horn cell diseases including
amyotrophic lateral sclerosis, post-polio paralysis, traumatic brain injury resulting in
quadriplegia, spina bifida, childhood cerebral degeneration, Alzheimer’s disease,
Parkinson’s disease (See Appendix A); or
c) Inability to carry out a functional weight shift due to one of, but not limited to, the
following diagnoses: spinal cord injury resulting in quadriplegia or paraplegia, other
spinal cord disease, multiple sclerosis, other demyelinating disease, cerebral palsy,
anterior horn cell diseases including amyotrophic lateral sclerosis, post-polio
paralysis, traumatic brain injury resulting in quadriplegia, spina bifida, childhood
cerebral degeneration, Alzheimer’s disease, Parkinson’s disease (See Appendix A); or
d) Confined to their wheelchair for more than four (4) continuous hours daily.
e) Documentation of malnutrition (past and present).
E2604
F5
#Skin protection wheelchair seat cushion, width 22 inches or greater, any depth
See coverage criteria for E2603
E2605
F5
#Positioning wheelchair seat cushion, width less than 22 inches, any depth
A positioning seat cushion (E2605) is covered when 1, 2 and 3 of the SPC guidelines are met and
the member has one of the following:
a) Significant postural asymmetries that are due to, but not limited to, one of the diagnoses
listed above under E2603 (b); or
b) One of the following diagnoses: monoplegia of the lower limb, hemiplegia due to
stroke, traumatic brain injury, or other etiology, muscular dystrophy, torsion dystonias,
spinocerebellar disease. (See Appendix A)
E2606
F5
#Positioning wheelchair seat cushion, width 22 inches or greater, any depth
See coverage criteria for E2605
E2607
F5
#Skin protection and positioning wheelchair seat cushion, width less than 22 inches, any depth
A combination skin protection and positioning seat cushion (E2607) is covered when criterion 1,
2, 3 of the SPC guidelines are met and the criteria for both a skin protection seat cushion and a
positioning seat cushion are met.
E2608
F5
#Skin protection and positioning wheelchair seat cushion, width 22 inches or greater, any
depth See coverage criteria for E2607
E2609
F5
Custom fabricated wheelchair seat cushion, any size (pediatric or adult)
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
59
A custom fabricated seat cushion (E2609) is covered if the criteria for a skin protection and
positioning seat cushion are met and there is a comprehensive written evaluation by a licensed
clinician (who is not an employee of or otherwise paid by a vendor or manufacturer) which
clearly explains why a standard seating system is not sufficient to meet the member’s seating
and positioning needs. (If a custom fabricated seat and back are integrated into a one-piece
cushion, code using the custom seat plus the custom back codes.)
E2611
F5
#General use wheelchair back cushion, width less than 22 inches, any height, including any type
mounting hardware
A general use back cushion (E2611) is covered when 1, 2 and 3 of the SPC guidelines are met.
E2612
F5
#General use wheelchair back cushion, width 22 inches or greater, any height, including any
type mounting hardware See coverage criteria for E2611
E2613
F5
#Positioning wheelchair back cushion, posterior, width less than 22 inches, any height, including
any type mounting hardware
A positioning back cushion (E2613) is covered when 1, 2 and 3 of the SPC guidelines are met and
the member has one of the following:
a) Significant postural asymmetries that are due to, but not limited to, one of the diagnoses
listed under E2603 (b); or
b) One of the following diagnoses: monoplegia of the lower limb, hemiplegia due to
stroke, traumatic brain injury, or other etiology, muscular dystrophy, torsion dystonias,
spinocerebellar disease. (See Appendix A)
E2614
F5
#Positioning wheelchair back cushion, posterior, width 22 inches or greater, any height,
including any type mounting hardware
See coverage criteria for E2613
E2615
F5
#Positioning wheelchair back cushion, posterior-lateral, width less than 22 inches, any height,
including any type mounting hardware
A positioning back cushion (E2615) is covered when 1, 2 and 3 of the SPC guidelines are met and
the member has one of the following:
a) Significant postural asymmetries that are due to, but not limited to, one of the diagnoses
listed under E2603 (b); or
b) One of the following diagnoses: monoplegia of the lower limb, hemiplegia due to
stroke, traumatic brain injury, or other etiology, muscular dystrophy, torsion dystonias,
spinocerebellar disease. (See Appendix A)
E2616
F5
#Positioning wheelchair back cushion, posterior-lateral, width 22 inches or greater, any height,
including any type mounting hardware
See coverage criteria for E2615
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
60
E2617
F5
Custom fabricated wheelchair back cushion, any size, including any type mounting hardware
(pediatric or adult)
A custom fabricated back cushion (E2617) is covered if the criteria for a positioning back cushion are
met and there is a comprehensive written evaluation by a licensed clinician (who is not an employee
of or otherwise paid by a vendor or manufacturer) which clearly explains why a standard seating
system is not sufficient to meet the member’s seating and positioning needs. (If a custom fabricated
seat and back are integrated into a one-piece cushion, code using the custom seat plus the custom
back codes.)
E2619
F20
#Replacement cover for wheelchair seat cushion or back cushion, each
E2620
F5
#Positioning wheelchair back cushion, planar back with lateral supports, width less than 22 inches,
any height, including any type mounting hardware
E2621
F5
Positioning wheelchair back cushion, planar back with lateral supports, width 22 inches or greater,
any height, including any type mounting hardware
E2622
F5
#Skin protection wheelchair seat cushion, adjustable, width less than 22 inches, any depth
See coverage criteria for E2603
E2623
F5
#Skin protection wheelchair seat cushion, adjustable, width 22 inches or greater, any depth
See coverage criteria for E2603
E2624
F5
#Skin protection and positioning wheelchair seat cushion, adjustable, width less than 22 inches, any
depth
See coverage criteria for E2607
E2625
F5
#Skin protection and positioning wheelchair seat cushion, adjustable, width 22 inches or greater, any
depth
See coverage criteria for E2607
E2626
F3
#Wheelchair accessory, shoulder elbow, mobile arm support attached to wheelchair, balanced,
adjustable
E2627
F3
#Wheelchair accessory, shoulder elbow, mobile arm support attached to wheelchair, balanced,
adjustable rancho type
E2628
F3
#Wheelchair accessory, shoulder elbow, mobile arm support attached to wheelchair, balanced,
reclining
E2629
F3
#Wheelchair accessory, shoulder elbow, mobile arm support attached to wheelchair, balanced,
friction arm support (friction dampening to proximal and distal joints)
E2630
F3
#Wheelchair accessory, shoulder elbow, mobile arm support, monosuspension arm and hand
support, overhead elbow forearm hand sling support, yoke type suspension support
E2631
F3
#Wheelchair accessory, addition to mobile arm support, elevating proximal arm
E2632
F3
#Wheelchair accessory, addition to mobile arm support, offset or lateral rocker arm with elastic
balance control
E2633
F3
#Wheelchair accessory, addition to mobile arm support, supinator
K0015
F3
#Detachable, nonadjustable height armrest, each
K0017
F3
#Detachable, adjustable height armrest, base, replacement only, each
K0018
F3
#Detachable, adjustable height armrest, upper portion, replacement only, each
K0019
F7
#Arm pad, replacement only, each
K0037
F3
#High mount flip-up footrest, each
K0038
F6
#Leg strap, each
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
61
K0039
F6
#Leg strap, H style, each
K0040
F4
#Adjustable angle footplate, each
K0041
F4
#Large size footplate, each
K0042
F4
#Standard size footplate, replacement only, each
K0043
F4
#Footrest, lower extension tube, replacement only, each
K0044
F4
#Footrest, upper hanger bracket, replacement only, each
K0045
F4
#Footrest, complete assembly, replacement only
K0046
F4
#Elevating leg rest, lower extension tube, replacement only, each
K0047
F4
#Elevating leg rest, upper hanger bracket, replacement only, each
K0052
F4
#Swing away, detachable footrests, replacement only, each
K0053
F4
#Elevating footrests, articulating (telescoping), each
K0056
F3
Seat height less than 17" or equal to or greater than 21" for a high strength, lightweight, or ultra-
lightweight wheelchair
K0065
F5
#Spoke protectors, each
K0071
F6
#Front caster assembly, complete, with pneumatic tire, replacement only, each
K0072
F6
#Front caster assembly, complete, with semi pneumatic tire, replacement only, each
K0073
F6
#Caster pin lock, each
K0077
F6
#Front caster assembly, complete, with solid tire, replacement only, each
K0098
F6
#Drive belt for power wheelchair, replacement only
K0105
F4
#IV hanger, each (for wheelchair)
K0108
F6
Other accessories (limited to wheeled mobility parts not listed)
K0108 Examples:
UESS padding and positioning blocks:
- Padding is covered in addition to a UESS when there is documented evidence of skin breakdown as a result
of weight bearing and that a care plan without padding, including times when the UESS was removed,
proved unsuccessful.
- Positioning blocks are covered when there is a medical need, due to strong spasticity or exaggerated
muscle activity, to stabilize the upper extremities on the UESS to allow for weight bearing.
- Positioning blocks may also be considered for mounting directly to a wheeled mobility device when the
member does not meet the coverage criteria for a UESS.
Foot-Ankle Padded Positioning Straps (e.g., ankle huggers):
- Covered when there is a medical need for stabilization of the foot and ankle due to strong spasticity or
exaggerated muscle activity and positioning in the wheelchair cannot be met with less costly alternatives,
such as any combination of heel loop/holders and or toe/loop/holders, with or without ankle straps.
Dynamic Foot Support Systems (i.e.: Dynamic Footrest Coil; Dynamic Footrest Gas Spring; Dynamic Footrest Hanger):
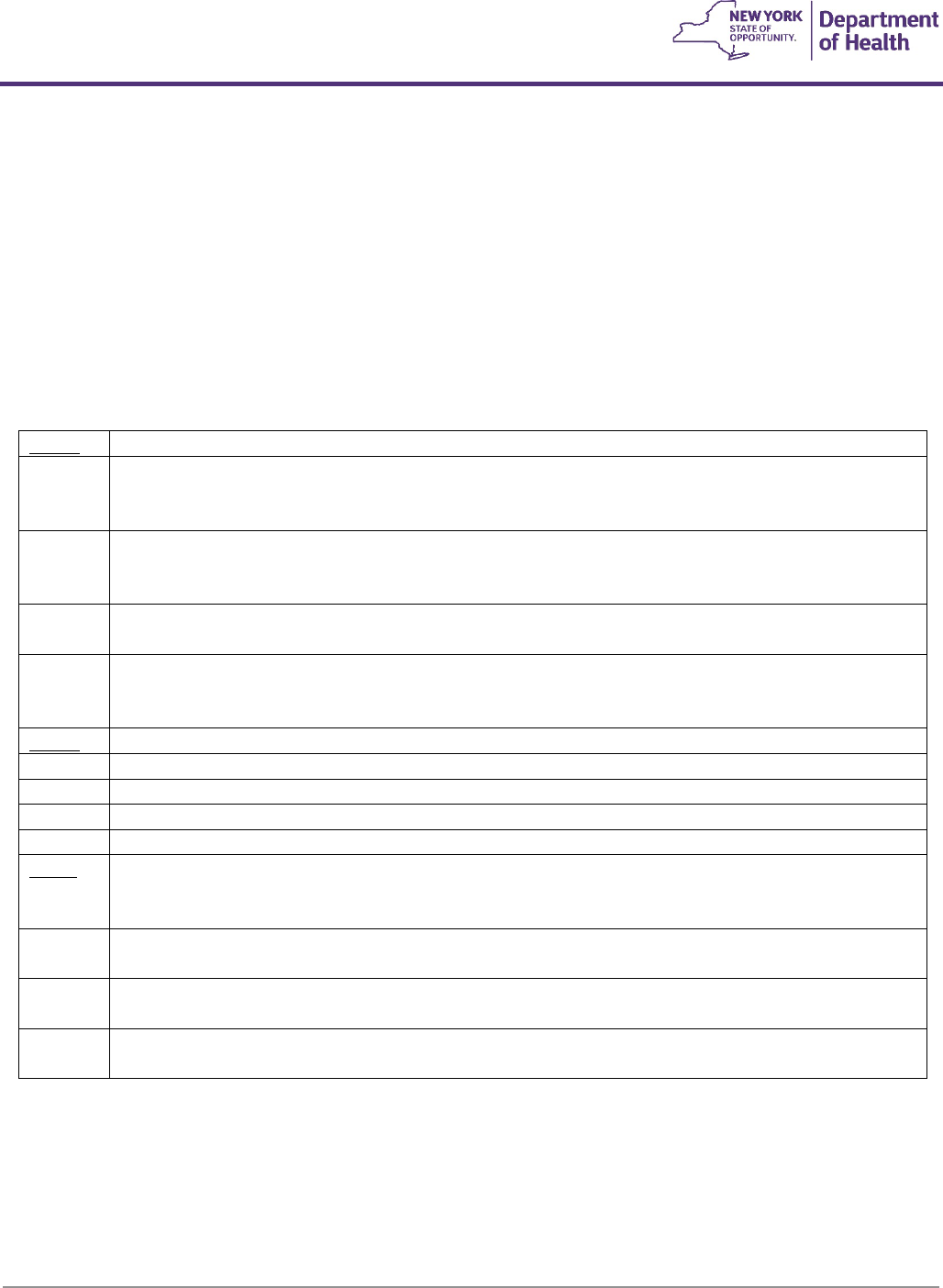
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
62
- Covered when the member has moderate to severe hypertonicity and less costly alternatives have been
tried and have not withstood the member’s tone, and there is documented evidence of frequent footrest,
footplate or wheelchair frame repairs and/or replacement.
Shock absorbers (non-standard caster forks, i.e.: Frog Legs or any other brands):
- Covered when the member has increased muscle tone that is triggered when driving the wheelchair over
bumps and cracks, or has documented low back pain that increases when driving the wheelchair over rough
terrain, or demonstrates fatigue with decreased proficiency in propelling the wheelchair, and the member
has shown a decrease in any of the above symptoms during a trial with the shock absorbers.
Miscellaneous Durable Medical Equipment
A4265
F9
Paraffin, per pound (for medically necessary paraffin bath unit)
A4556
F9
Electrodes (e.g., Apnea monitor), per pair (up to 2 pair, any type) TENs Replacement electrodes are
covered for members with a diagnosis of knee pain due to osteoarthritis. Please refer to the coverage
criteria listed under code E0730
A4557
F6
Lead wires (e.g., Apnea monitor), per pair (up to 2 pair, any type) TENs Replacement lead wires are
covered for members with a diagnosis of knee pain due to osteoarthritis. Please refer to the coverage
criteria listed under code E0730
A4602
Replacement battery for external infusion pump owned by patient, lithium, 1.5 volt, each (also see
A4632, K0601-K0605)
A4630
F7
#Replacement batteries, medically necessary, transcutaneous electrical stimulator, owned by patient
TENs Replacement batteries are covered for members with a diagnosis of knee pain due to
osteoarthritis. Please refer to the coverage criteria listed under code E0730.
A4632
F7
Replacement battery for external infusion pump, any type, each (also see K0601-K0605)
A7520
F9
Tracheostomy/laryngectomy tube, non-cuffed, polyvinylchloride (PVC), silicone or equal, each
A7521
F9
Tracheostomy/laryngectomy tube, cuffed, polyvinylchloride (PVC), silicone or equal, each
A7522
F7
Tracheostomy/laryngectomy tube, stainless steel or equal (sterilizable and reusable), each
A7524
F7
Tracheostoma stent/stud/button, each
E0235
F2
Paraffin bath unit, portable
Covered for rheumatoid arthritis only with documented treatment failure with medication and when
ordered by a rheumatologist.
B9002
F3
‘-RR’
#Enteral nutrition infusion pump, any type
B9004
F3
‘-RR’
#Parenteral nutrition infusion pump, portable
B9006
F3
‘-RR’
#Parenteral nutrition infusion pump, stationary
Note: The maximum monthly rental amount for infusion pumps (codes B9002, B9004, B9006, E0781, and E0791) is
$60.00. The maximum daily rental amount for a parenteral infusion pump for short-term use is $5.00 per day up to a
total of $60.00 per month. The maximum monthly rental amount is applicable if a pump is left in the home for a
monthly medication dose. Medicaid rents with option to purchase. All rental fees must be deducted from purchase
price.
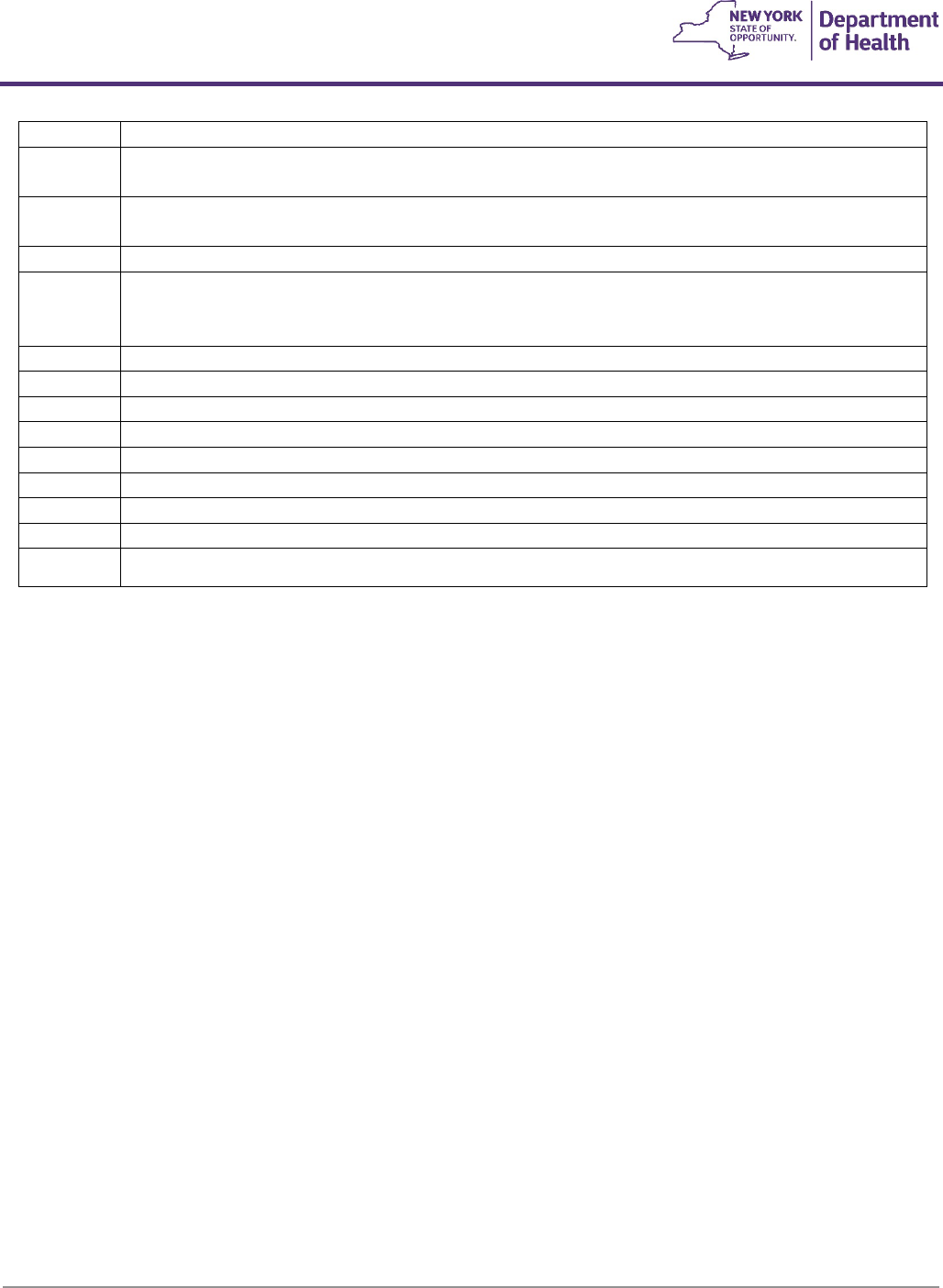
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
63
E0163
F3
#Commode chair, mobile or stationary, with fixed arms
E0165
F3
#Commode chair, mobile or stationary, with detachable arms (removable, drop down or swing
away)
E0168
F5
#Commode chair, extra wide and/or heavy duty, stationary or mobile, with or without arms, any
type, each
E0175
F3
#Foot rest, for use with commode chair, each (one or two piece)
E0202
F2
#Phototherapy (bilirubin) light with photometer
(rental only, blanket or overhead light)
(treatment plan greater than 10 days requires prior approval)
E0240
F3
#Bath/shower chair, with or without wheels, any size
E0241
F2
Bathtub wall rail, each
E0243
F2
Toilet rail, each
E0244
F3
#Raised toilet seat (with or without arms)
E0245
F3
#Tub stool or bench
E0246
F2
Transfer tub rail attachment
E0247
F3
#Transfer bench for tub or toilet with or without commode opening
E0248
F3
#Transfer bench, heavy duty, for tub or toilet with or without commode opening
E0604
F7
#Breast pump, hospital grade, electric (AC and/or DC), any type (rental only)
Hospital Grade Breast Pump
- Hospital or professional grade breast pump coverage is limited to cases of prematurity (including multiple
gestation), neurologic disorders, genetic abnormalities (e.g., Down’s Syndrome), anatomic and mechanical
malformations (e.g., cleft lip and palate), congenital malformations requiring surgery (e.g., respiratory, cardiac,
gastrointestinal, CNS), prolonged infant hospitalization, or other conditions that prevent normal breastfeeding
(e.g. respiratory compromise).
- A Dispensing Validation System (DVS) authorization is available for up to 2 months. Prior approval is required
for cases requiring more than 2 months rental (e.g. extreme prematurity, less than 28 weeks gestation).
The hospital grade electric (multi-user) pump must:
- Must not exceed 12 pounds including carrying case.
- Operate on a 110-volt household current and be UL listed.
- Have a visible breast milk pathway and no milk is able to contact the internal pump-motor unit parts at any
time when the product is used per manufacturer instructions.
- Have an adjustable suction pressure between 30 mm Hg and 250 mm Hg at the breast shield during use; a
suction range just at the low or high end of the range is not acceptable.
- Have an automatic mechanism to prevent suction greater than 250 mm Hg when used according to
manufacturer’s instructions to prevent nipple trauma.
- Have a mechanism for automatic release of suction for safety.
- Have variable/adjustable cycling not less than 30 cycles per minute; one fixed cycling time is not acceptable.
o Have double pumping capacity, which is simultaneous, not alternating.
o Include a pumping kit for each personal user including durable tubing to connect to the pump and
flanges and have single and double pumping capacities.
o Include a carrying case made of durable, washable materials for the pump-motor assembly and pump
kit accessories; this is recommended if the pump needs to be portable.
Minimum Breast Pump Specifications for Single-User/Multi-User* Double Pumping Kits
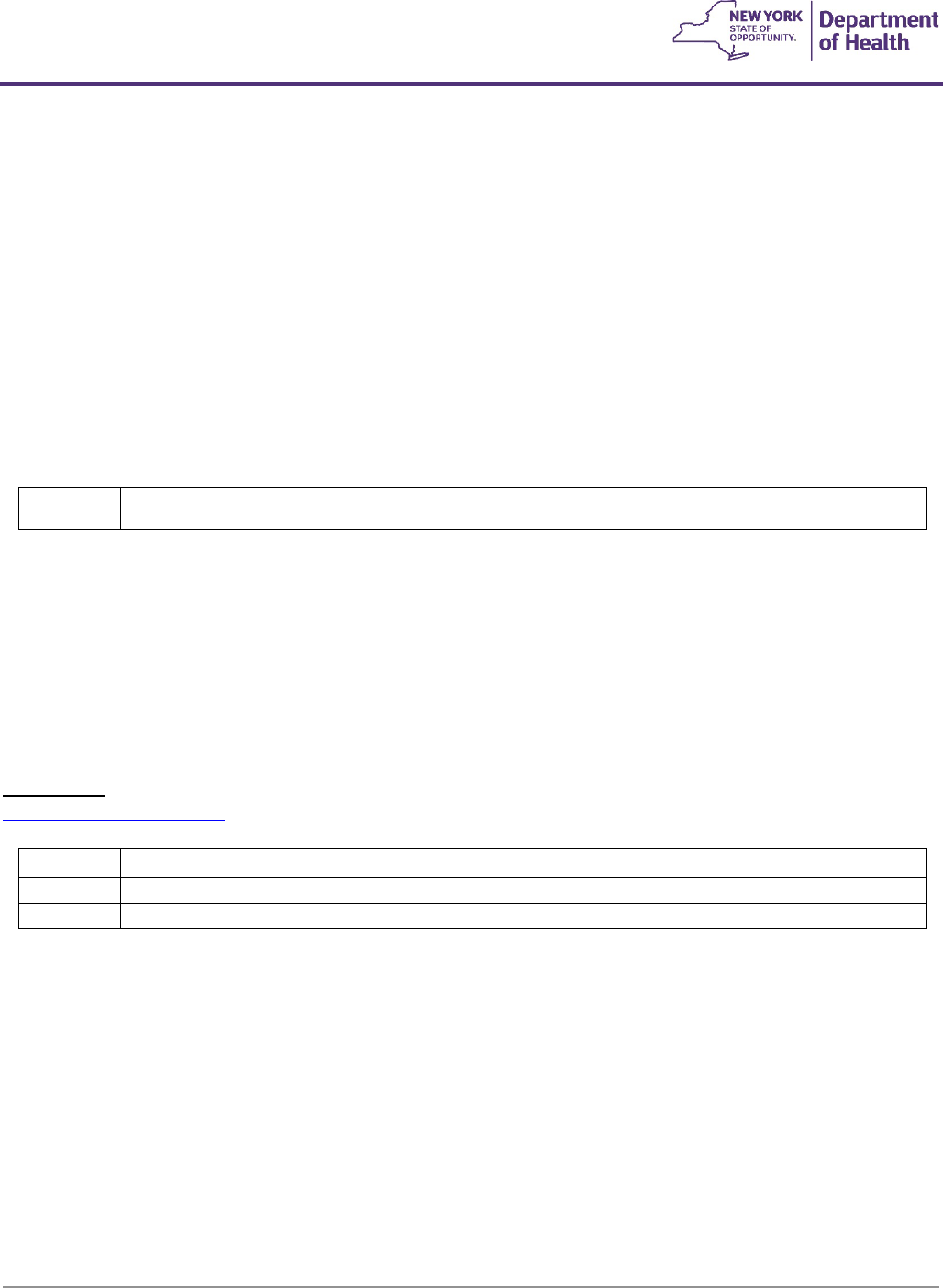
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
64
*Use with hospital grade rentals.
The kit must:
- Include breast flanges that are either adjustable/flexible or if rigid, come in at least two (2) sizes to
accommodate different breast sizes with no sharp edges.
- Be packaged pre-assembled with all accessories necessary for pumping two breasts simultaneously or only
one breast manually.
- Include at least two collection bottles of four (4) to six (6) ounces with a spill-proof cap and standard-sized
opening and be bisphenol-A (BPA) and DHEP-free.
- Contain collection bottle(s) and flanges made of medical grade quality to allow for repeated boiling
and/or dishwasher cleaning which are scratch resistant and non-breakable.
- Have durable tubing designed for long-term pumping use.
- Design and materials of the furnished assembly shall allow viewing the breast milk pathway.
- Include an adapter that can be used as an alternate power source other than electric; this is recommended
and may come as part of pump assembly or pumping kit.
E0619
F9
#Apnea monitor, with recording feature
Apnea Monitor
- Apnea monitors will only be rented. As with all rentals, the monthly fee includes all necessary features and
equipment, delivery, maintenance and repair costs, parts, supplies and services for equipment set-up,
maintenance, and replacement of worn essential accessories or parts, loading, or downloading software, and
back-up equipment as needed.
- For children under 1 year of age, an electronic DVS prior authorization number must be obtained prior to
providing an apnea monitor. Board certified pulmonologists or neonatologists only are qualified to order
apnea monitors.
- Prior approval is still required for members over 1 (one) year of age.
Related Links:
Infant Apnea Monitor billing
E0621
F6
Sling or seat, patient lift, canvas or nylon
E0627
F2
#Seat lift mechanism, electric, any type (see criteria below)
E0629
F2
#Seat lift mechanism, non-electric, any type:
Seat Lift Mechanism
Only separate seat lift mechanisms for use with patient owned furniture are covered. These codes are not to be used to
bill seat lift mechanisms incorporated into furniture.
A separate seat lift mechanism is covered if all the following criteria are met:
1. The member must have severe arthritis of the hip or knee or have a severe neuromuscular disease.
2. The seat lift mechanism must be a part of the physician's course of treatment and be prescribed to effect
improvement, or arrest or retard deterioration in the member's condition. (The physician ordering the seat lift
mechanism must be the treating physician or a consulting physician for the disease or condition resulting in
the need for a seat lift. The physician's record must document that all appropriate therapeutic modalities (e.g.
medication, physical therapy) have been tried and failed to enable the member to transfer from a chair to a
standing position.)
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
65
3. The member must be completely incapable of standing up from a regular armchair or any chair in their home.
(The fact that a member has difficulty or is even incapable of getting up from a chair, particularly a low chair, is
not sufficient justification for a seat lift mechanism. Almost all members who are capable of ambulating can get
out of an ordinary chair if the seat height is appropriate and the chair has arms.)
4. Once standing, the member must have the ability to ambulate.
- Coverage is limited to those types which operate smoothly, can be controlled by the member, and
effectively assist a member in standing up and sitting down without other assistance.
- Excluded from coverage is the type of lift which operates by spring release mechanism with a sudden,
catapult-like motion and jolts the member from a seated to a standing position.
- Patient (member) and seat lift equipment (E0628, E0629 & E0630) are not to be billed in combination.
E0630
F2
#Patient lift, hydraulic or mechanical, includes any seat, sling, strap(s) or pad(s)
Covered if the severity of the medical condition is such that periodic movement is necessary to
effect improvement or to retard deterioration of that condition, and the alternative to use of this
device is wheelchair or bed confinement.
E1399
F9
Durable medical equipment, miscellaneous
E1399 Examples:
Positioning bath chair, tub, or shower stand:
- A positioning bath chair is covered when the documented medical and hygiene needs of the member
require proper positioning and alignment while providing a stable and safe means of support during
bathing. The positioning bath chair’s maximum reimbursement amount (MRA) includes all accessories
required for positioning of the member such as but not limited to a head support, trunk laterals, hip
laterals, pelvic belt or chest belt.
- A tub stand addition is covered when the documented medical and safety needs of the member require a
tub stand and when the dimension of the member’s tub will accommodate the requested stand.
- A shower stand addition is covered when the documented medical and safety needs of the member require
the use of a shower stand.
To obtain a prior approval number for a positioning bath chair and stand additions, the item(s) must be coded E1399
(Durable Medical Equipment, Miscellaneous) and submitted using the following procedure:
a) DME provider obtains valid order and medical documentation (to maintain in their records for audit
purposes) from the ordering practitioner;
b) DME provider submits a prior approval request containing a copy of valid order and either a manufacturer’s
price quote or the item’s make and model;
c) These items must be submitted singularly on one line on a separate prior approval from all other prior
approval items;
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
66
d) The DME Provider will be issued a prior approval priced up to the established MRA and may bill Medicaid
upon dispensing.
Reimbursement for positioning bath chairs and stand additions can be found on the DMEPOS Fee Schedule under
E1399
https://www.emedny.org/ProviderManuals/DME/index.aspx
Reclining shower/commode chair:
Reclining shower-commode chair is covered when recline is necessary to complete hygiene needs, and the member
either has positioning needs that cannot be met by upright and a fixed angle chair or the member’s postural control
requires recline.
Reimbursement for reclining shower/commode chair can be found on the DMEPOS Fee Schedule under E1399
https://www.emedny.org/ProviderManuals/DME/index.aspx
Rehab (self-propelling) shower/commode chair:
- Rehab (self-propelling) shower/commode chairs are defined as chairs that have large rear wheelchair style
wheels, typically 18 inches or greater, to allow for self-propulsion.
- Rehab style chairs are covered when the member has access to a roll in shower and is capable of
independently propelling the chair into the shower and independently completing all aspects of the shower
routine.
Toilet systems:
Covered with:
- Documentation from a Urologist or Neurologist establishing the member is physiologically capable of
being toilet trained.
- Evidence of success with an established toilet training program.
- Evidence the member is unable to use a standard toilet due to physical limitations requiring additional
support.
Standing frame systems:
Use E1399 for member’s requiring a single (E0638) or multi-position (E0641) standing frame that accommodates an
individual over 60 inches tall. See Home Standing Systems guidelines below.
Home Standing Systems
General Guidelines:
- Standers are durable medical equipment (DME) designed to assist a child or adult in attaining and
maintaining an upright position.
- Standers may provide medical and functional benefits to otherwise bed or chair-bound individuals.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
67
- DMEPOS providers must provide documentation that the member has tried more cost-effective alternatives
and still requires a stander.
- A glider component does not qualify as DME, as it is non-medical in nature and is primarily used for
exercise purposes.
Clinical Coverage:
- The member is unable to stand or ambulate independently due to conditions such as, but not limited to,
neuromuscular or congenital disorders, including acquired skeletal abnormalities.
- The member is at high risk for lower extremity contractures that cannot be appropriately managed by other
treatment modalities (i.e. stretching, active therapy, home programs, etc.).
- The alignment of the member’s lower extremities is such that they can tolerate a standing or upright
position.
- The member does not have orthostatic hypotension, postural tachycardia syndrome, osteogenesis
imperfecta, osteoporosis and other brittle bone diseases, or hip or knee flexion contractures of more than
45°.
- The member has demonstrated improved mobility, function and physiologic symptoms or has maintained
status with the use of the requested stander (when other alternatives have failed) and is able to follow a
home standing program incorporating the use of the stander (as documented by clinical standing program
or home trial with the requested stander).
- The member is unable to stand or ambulate with caregiver assistance or ambulatory assistive device a
sufficient duration/distance to achieve a medical benefit.
- The member does not have, and it is not anticipated they will require, a walker or gait trainer. Provision of
both a walker/gait trainer and standing device is typically considered a duplication of service, as both type
devices address the medical need for weight bearing.
- There is a home therapy plan outlining the use of the requested stander.
- The member can self-propel the mobile stander (code E0642 only), the documentation establishes the
specific medical need(s) that will be met while using the mobile stander, and why these medical needs must
be met while utilizing the mobile stander.
Documentation Requirements:
- A prescription including the stander and any modifications/accessories requested.
- A detailed letter of medical necessity (LMN) that includes:
1. A comprehensive history and physical exam by a licensed physician, physical therapist, or occupational
therapist.
2. A summary of the existing medical condition, age at diagnosis, prognosis, and co-morbid conditions.
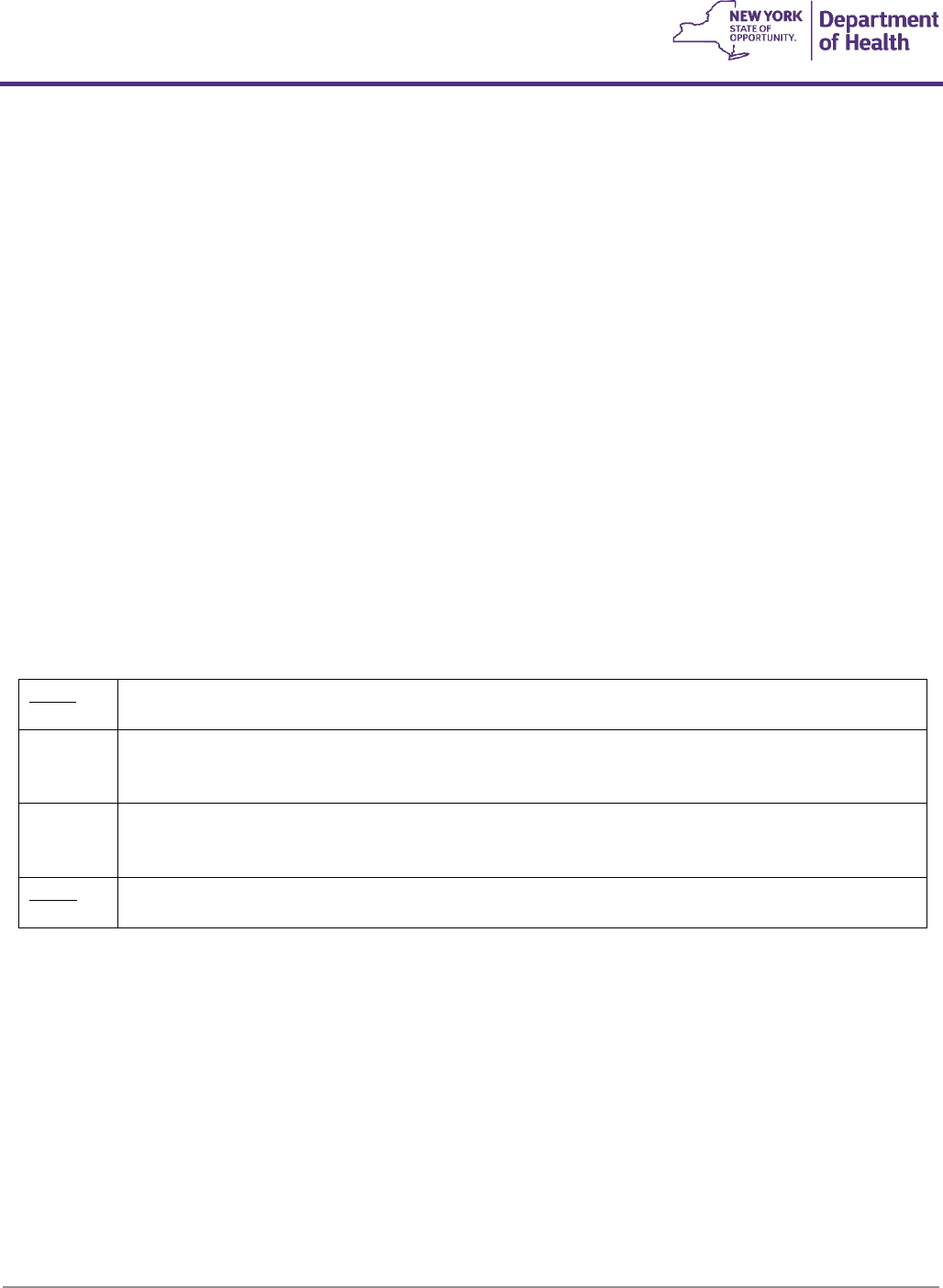
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
68
3. The member’s functional and physical assessment including strength, range of motion, tone, sensation,
balance, ADLs, and functional status.
4. Documentation of failure of less costly alternatives (include make and model of alternatives tried as well as
the length of the trial with each alternative).
5. A home therapy plan outlining the planned use of the requested stander.
- Documentation that the member does not have sufficient access to equipment in an alternative setting, e.g.
clinic, outpatient therapy, etc.
- Documentation regarding the level of caregiver assistance available/needed on daily basis.
- Documentation that the member’s home can accommodate the requested stander and that the
family/caregiver has been trained in the use and maintenance of the requested stander.
- Documentation the member does not have, and it is not anticipated they will require, a walker or gait
trainer. Provision of both a walker/gait trainer and standing device is typically considered a duplication of
service, as both type devices address the medical need for weight bearing.
- Documentation that the member is able to self-propel the mobile stander (code E0642 only), the specific
medical need(s) that will be met while using the mobile stander, and why these medical needs must be met
while utilizing the mobile stander.
- The fees listed for home standing systems include all necessary prompts and supports.
E0637
F2
‘-RR’
Combination sit to stand frame/table system, any size including pediatric, with seat lift feature, with
or without wheels
E0638
F2
‘-RR’
#Standing frame/table system, one position (e.g. upright, supine or prone stander), any size
including pediatric, with or without wheels
Prior approval is required for ages 21 and over
E0641
F2
‘-RR’
#Standing frame/table system, multi-position (e.g. three-way stander), any size including pediatric,
with or without wheels
Prior approval is required for ages 21 and over
E0642
F2
Standing frame/table system, mobile (dynamic stander), any size including pediatric (self-propelled,
multi-positioning, no lift feature, for use when gait trainer does not meet medical need)
Pneumatic Compression Device (PCD)
Pneumatic compression devices (lymphedema pumps) are covered for the treatment of generalized or refractory
lymphedema, or refractory edema from chronic venous insufficiency, only when all less invasive treatments have been
attempted and are unsuccessful.
Coverage Criteria for E0650 and E0651
I. Lymphedema
- The member has a diagnosis of lymphedema, and
- Persistence of chronic and severe lymphedema as documented by presence of at least one of the following:
• Marked hyperkeratosis with hyperplasia and hyperpigmentation

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
69
• Papillomatosis cutis lymphostatica
• Deformity of limb or involved area - i.e., elephantiasis (measurements to support compared to
contralateral limb)
• Skin breakdown with persisting lymphorrhea
• Detailed measurements over time confirming the persistence of lymphedema with a history evidencing a
likely etiology, and
- A documented 4-week trial of conservative therapy demonstrating failed response to the treatment is
required. The trial must include
ALL the following:
• Regular compliance with an appropriate compression bandage system or compression garment to provide
adequate compression. (Adequate compression is defined as having sufficient pressure at lowest pressure
point to cause fluid movement, and sufficient pressure across the gradient (from highest to lowest
pressure point) to move fluid from distal to proximal.) The compression should not create a tourniquet
effect at any point.
• The garment may be prefabricated or custom-fabricated but must provide adequate graduated
compression with a minimum of 30mmHg distally.
• Regular exercise program
• Elevation of limb
• Evidence of participation in a manual lymph drainage (MLD) program and results.
• Evidence of appropriate medication treatment for co-morbidities, i.e., congestive heart failure (CHF) and
results.
- Symptoms and objective findings, including measurements which establish the severity of the condition
- Reason the device is required, including treatments which have been tried and failed
II. Chronic Venous Insufficiency (CVI)
PCDs coded E0650 or E0651 are covered for treatment of CVI of the lower extremities ONLY if the member has ALL
the following:
- Edema in the affected lower extremity
- One or more venous stasis ulcer(s)
- Non-healing ulcers after a six-month trial of conservative therapy directed by the treating practitioner. The six-
month trial includes:
• The 4-week lymphedema trial criteria outlined above; AND
• Appropriate wound care for the ulcer(s) (including sharp debridement where appropriate)
Coverage Criteria for E0652
E0652 is only covered when the individual has unique characteristics which prevent them from receiving adequate
satisfactory pneumatic compression treatment using a non-segmented device along with a segmented appliance or
compression device without manual control of the pressure in each chamber.
A PCD coded as E0652 is covered for the treatment of lymphedema extending onto the chest, trunk and/or abdomen
when
ALL the following are met:
- Diagnosis of lymphedema of an extremity
- Coverage criteria for E0650 and E0651 are met
- The member has lymphedema extending onto the chest, trunk and/or abdomen that extends past the limits of
a standard compression sleeve, and the chest, trunk and/or abdominal lymphedema has failed to improve with
a four-week trial. 4-week trial includes all the requirements for the 4-week trial outlined above under
Lymphedema,
AND:
• Manual lymph drainage (MLD) (where available) and self MLD for at least 30 minutes/day
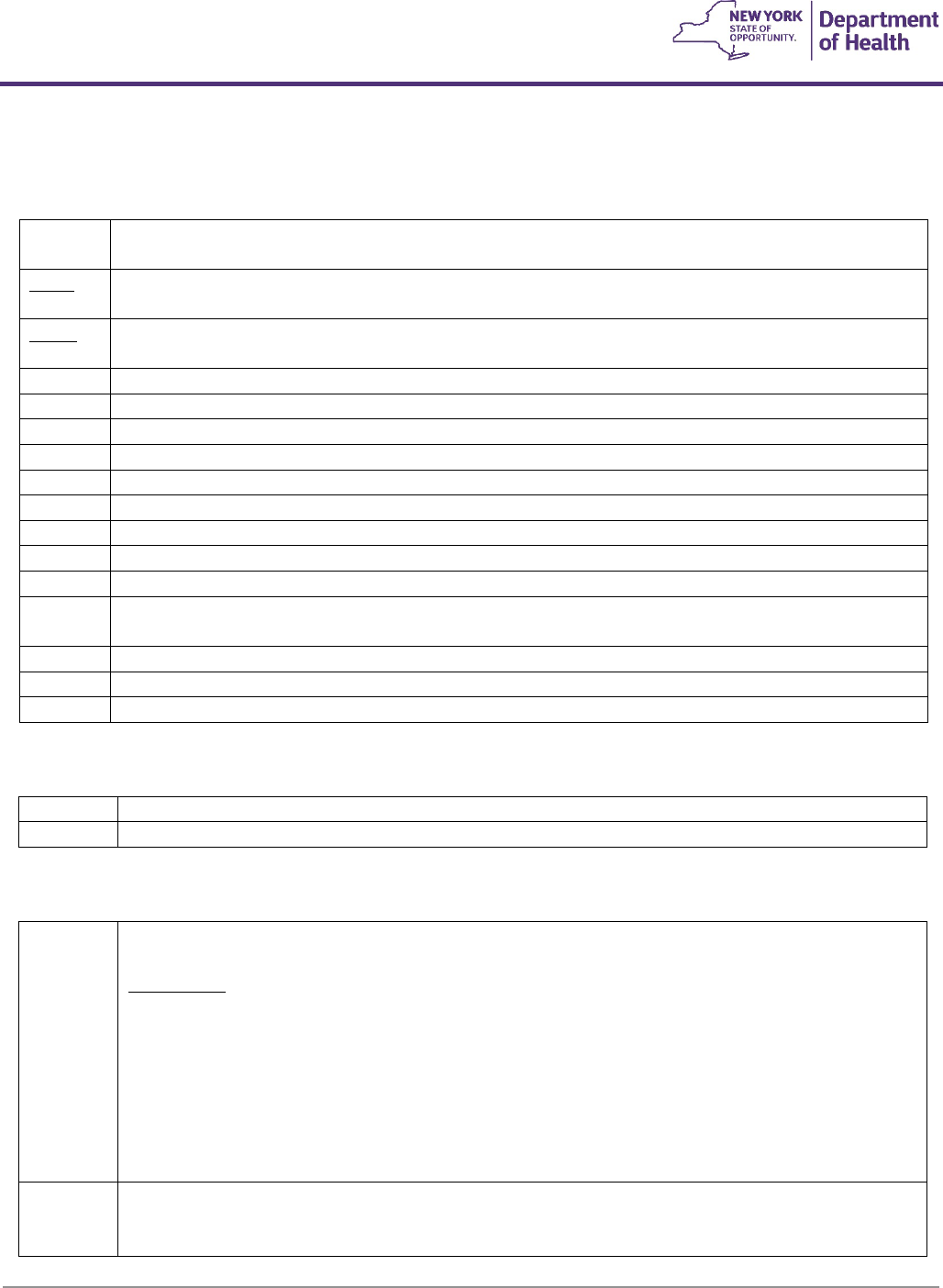
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
70
• Evaluation of diet and implementation of necessary changes
• Medications as appropriate (i.e., diuretics and/or treatment of CHF, etc.)
• correction (where possible) of anemia and/or hyponatremia
Safety Equipment
E0700
F5
#Safety equipment, device or accessory, any type (limited to gait belt)
E0705
F6
Transfer device, any type, each
TENS and Osteogenesis Stimulator
E0730
F5
#Transcutaneous electrical nerve stimulation (tens) device, four or more leads, for multiple nerve
stimulation
(dual channel)
Covered for:
- Members with a diagnosis of knee pain due to osteoarthritis.
- Reimbursable ICD codes are limited to: M17.0, M17.11, M17.12, M17.2, M17.31, M17.32,
M17.4, and M17.5.
- The following codes may be billed in conjunction with E0730: A4556, A4557 and A4630.
E0747
F2
#Osteogenesis stimulator electrical, noninvasive, other than spinal applications
Covered when ordered by a board-certified or board-eligible orthopedic surgeon for:
1. Nonunion of long bone fractures confirmed by a minimum 2 sets of radiographs:
E0650
F2
#Pneumatic compressor, non-segmental home model, (Lymphedema pump)
Appliances (garments) appropriate for use are E0655, E0660, E0665, E0666, E0671, E0672 and E0673
E0651
F2
Pneumatic compressor, segmental home model without calibrated gradient pressure
Appliances (garments) appropriate for use are E0667, E0668, E0669
E0652
F2
Pneumatic compressor, segmental home model with calibrated gradient pressure
Appliances (garments) appropriate for use are E0656, E0657, E0667, E0668, E0669 and E0670
E0655
F3
#Non-segmental pneumatic appliance for use with pneumatic compressor, half arm
E0656
F3
#Segmental pneumatic appliance for use with pneumatic compressor, trunk
E0657
F3
#Segmental pneumatic appliance for use with pneumatic compressor, chest
E0660
F3
#Non-segmental pneumatic appliance for use with pneumatic compressor, full leg
E0665
F3
#Non-segmental pneumatic appliance for use with pneumatic compressor, full arm
E0666
F3
#Non-segmental pneumatic appliance for use with pneumatic compressor, half leg
E0667
F3
#Segmental pneumatic appliance for use with pneumatic compressor, full leg
E0668
F3
#Segmental pneumatic appliance for use with pneumatic compressor, full arm
E0669
F3
#Segmental pneumatic appliance for use with pneumatic compressor, half leg
E0670
F3
#Segmental pneumatic appliance for use with pneumatic compressor, integrated, two full legs and
trunk
E0671
F3
#Segmental gradient pressure pneumatic appliance, full leg
E0672
F3
#Segmental gradient pressure pneumatic appliance, full arm
E0673
F3
#Segmental gradient pressure pneumatic appliance, half leg
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
71
- including multiple views of the fracture site,
- obtained prior to starting treatment with the osteogenic stimulator,
- separated by a minimum of 90 days, and
- accompanied by written physician interpretation stating there has been no clinically
significant evidence of fracture healing between the 2 sets of radiographs; OR
2. Failed fusion of a joint other than the spine, where a minimum of 9 months has elapsed since
the last surgery; OR
3. Congenital pseudarthrosis.
Not covered for:
1. Nonunion fractures of the skull.
2. Tumor-related fractures.
Related Links:
The osteogenesis stimulator worksheet is available at:
https://www.emedny.org/ProviderManuals/DME/PDFS/Osteogenesis_Stimulator_Worksheet
2019.pdf
E0748
F2
#Osteogenesis stimulator electrical, noninvasive, spinal applications
Covered when ordered by a board-certified or board-eligible orthopedic surgeon or neurosurgeon
for:
1. Failed spinal fusion where a minimum of 9 months has elapsed since the last surgery; OR
2. Following multilevel spinal fusion surgery; OR
3. Following spinal fusion surgery where there is a history of a previously failed spinal fusion at the
same site.
Not covered for:
1. Nonunion fractures of vertebral fractures.
Related Links:
The osteogenesis stimulator worksheet is available at:
https://www.emedny.org/ProviderManuals/DME/PDFS/Osteogenesis_Stimulator_Worksheet
2019.pdf
E0760
F2
#Osteogenesis stimulator, low intensity ultrasound, non-invasive
Covered when ordered by a board-certified or board-eligible orthopedic surgeon for:
Nonunion of long bone fractures confirmed by a minimum 2 sets of radiographs:
1. including multiple views of the fracture site,
2. obtained prior to starting treatment with the osteogenic stimulator,
3. separated by a minimum of 90 days, and
4. accompanied by written physician interpretation stating there has been no clinically
significant evidence of fracture healing between the 2 sets of radiographs.
Not covered for:
1. Nonunion fractures of the skull or vertebrae.
2. Tumor-related fractures.
3. Fresh fracture or delayed union.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
72
4. When used concurrently with other non-invasive osteogenic devices.
Related Links:
The osteogenesis stimulator worksheet is available at:
https://www.emedny.org/ProviderManuals/DME/PDFS/Osteogenesis_Stimulator_Worksheet
2019.pdf
Infusion Pumps
E0776
F2
‘-RR’
#I.V. pole
E0781
F3
‘-RR’
#Ambulatory infusion pump, single or multiple channels, electric or battery operated, with
administrative equipment, worn by patient
E0784
F3
External ambulatory infusion pump, insulin
An external ambulatory insulin infusion pump will be covered for the diagnosis of diabetes mellitus
when ordered by an endocrinologist or a medical practitioner who has experience managing
patients on continuous subcutaneous insulin infusion therapy if the following criteria are
demonstrated and documented in the clinical and DMEPOS provider’s records:
1. The member has been on a program of multiple daily injections of insulin (i.e., at least 3
injections per day) with frequent self-adjustments of insulin dose for at least 6 months prior to
initiation of the insulin pump and has failed to achieve acceptable control of blood sugars that
are not explained by poor motivation or compliance
AND
i. has one or more of the following criteria while receiving multiple daily injections:
a) HbA1c >7%
b) History of recurring hypoglycemia
c) Wide fluctuations in blood glucose before mealtime (>140mg/dl)
d) Dawn phenomenon in a fasting state (>200mg/dl)
e) History of severe glycemic excursions
AND
ii. has completed a comprehensive diabetes education program.
2. The member has a diagnosis of gestational diabetes.
Preferred Diabetic Supply Program
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
73
Topical Hyperbaric Oxygen Chamber
A4575
F2
#Topical hyperbaric oxygen chamber, disposable
General Definitions:
- Topical oxygen wound therapy (TOWT) is the controlled application of 100% oxygen directly to an open
moist wound at slightly higher than atmospheric pressure. An oxygen concentrator is connected to an FDA
approved O2 boot and/or O2 sacral device that are for onetime use and disposable, therefore reducing the
risk of cross contamination.
- Staging: The staging of pressure ulcers used in this policy is as follows:
1. Stage I: nonblanchable erythema of intact light toned skin or darker or violet hue in darkly pigmented
skin.
2. Stage II: partial thickness skin loss involving epidermis and/or dermis.
3. Stage III: full thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend
down to, but not through, underlying fascia.
4. Stage IV: full thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone,
or supporting structures.
- Wound healing: Defined as improvement occurring in either the surface area or depth of the wound. Lack
of improvement of a wound is defined as a lack of progress in these quantitative measurements.
Coverage Criteria:
- TOWT (A4575 with E1390) is covered when criteria 1 and any of criteria 2-6 are met:
1. A complete wound therapy program as applicable, depending on the type of wound, has been attempted
prior to the application of TOWT, including:
a) Documentation in the member's medical record of evaluation, care, compliance, and wound
measurements by the treating physician, and
Disposable insulin pump supplies and meters (i.e. Omnipod) are covered under the Preferred
Diabetic Supply Program. Please see the pharmacy preferred diabetic supply program link below for
additional information.
https://newyork.fhsc.com/providers/diabeticsupplies.asp
E0791
F3
‘-RR’
Parenteral infusion pump, stationary, single or multichannel
Covered if both the therapy and the prescribed pump are appropriate for home use and adequate
supervision by the physician is specified on the prescription.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
74
b) Application of dressings to maintain a moist wound environment, and
c) Debridement of necrotic tissue if present, and
d) Evaluation of and provision for adequate nutritional status, and
2. Stage IV pressure ulcers:
a) The member has been appropriately turned and positioned, and
b) The member has used a support surface for pressure ulcers on the posterior trunk or pelvis (not
required if the ulcer is not on the trunk or pelvis), and
c) The member's moisture and incontinence have been appropriately managed, or
3. Neuropathic (for example, diabetic) ulcers:
a) The member has been on a comprehensive diabetic management program, and
b) Reduction in pressure on a foot ulcer has been accomplished with appropriate modalities, or
4. Venous insufficiency ulcers:
a) Compression bandages and/or garments have been consistently applied, and
b) Leg elevation and ambulation have been encouraged, or
5. For non-healing surgically created or traumatic wounds, documentation of medical necessity for
accelerated formation of granulation tissue that cannot be achieved by other topical wound treatments, or
6. A chronic (being present for at least 30 days) ulcer of mixed etiology.
Non-Covered Indications:
- TOWT is considered investigational, not medically necessary, medically contraindicated and not covered for
all other indications, including but not limited to, the following:
1. The presence in the wound of necrotic tissue with eschar, if debridement is not attempted;
2. Untreated osteomyelitis within the vicinity of the wound;
3. Cancer present in the wound;
4. The presence of a fistula to an organ or body cavity within the vicinity of the wound;
5. Stage I, II or III pressure ulcers.
General Guidelines:

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
75
- The procedure codes for billing TOWT are A4575 Topical oxygen chamber, disposable and E1390 Oxygen
concentrator, single delivery port, capable of delivering 85% or greater oxygen concentration at the
prescribed flow rate.
- Payment for E1390 includes all necessary equipment, delivery, maintenance and repair costs, parts, supplies
and services for equipment set-up, maintenance, and replacement of worn essential accessories and parts.
- Payment for A4575 includes the dressing set and canister set used in conjunction with E1390 and contains
all necessary components, including but not limited to an occlusive dressing which creates a seal around
the wound site for maintaining the desired concentration of oxygen at the wound.
- Payment for E1390 and A4575 are considered payment in full for TOWT.
- An initial electronic prior authorization (DVS) will be granted for A4575 for a maximum of 16 days in a 28-
day period, as treatment is 4 days on, 3 days off. The DMEPOS provider should request authorization once
for the number of days (units) based on the written order. Prior approval is required for treatment
exceeding 4 weeks. E1390 is prior authorized (DVS) and is billed monthly.
- TOWT should be attempted first in a hospital or another health care facility prior to discharge to the home
setting. In these continuing cases, documentation should reflect member compliance and pain
management during application of TOWT. If TOWT has not been attempted, DMEPOS providers must
obtain an initial electronic prior authorization of two weeks (8 days or units) only. Prior approval may then
be requested for an extension of the treatment.
- Documentation of previous treatment regimens and how the member meets the coverage criteria above
must be maintained in the member’s medical record and available upon request. This documentation must
include dressing types and frequency of change, changes in wound conditions (including precise length,
width and surface area measurements), quantity of exudates, presence of granulation and necrotic tissue,
concurrent measures being addressed relevant to wound therapy (debridement, nutritional concerns,
support surfaces in use, positioning, incontinence control, etc.) and training received by the member/family
in the application of the occlusive dressing to the wound site and proper hook up of the oxygen to the
dressing set.
- When an extension of treatment is requested, the following documentation must be submitted: how the
member meets the coverage criteria, status of wound healing, weekly quantitative measurements of wound
characteristics, wound length, width and depth (surface area) and amount of wound exudate (drainage) and
member compliance with the treatment plan. If detailed documentation is insufficient or if any measurable
degree of wound healing has failed to occur, prior approval beyond the initial approved period of service
will not be granted.
- Upon completion of treatment, documentation regarding the outcome of treatment with TOWT must be
submitted to the prior approval office.
Negative Pressure Wound Therapy
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
76
E2402
F2
#Negative pressure wound therapy electrical pump, stationary or portable (Bill as a monthly
recurring rental rate with modifier “RR”. Initial 30 days allowed without prior approval)
- Supplies are billed separately:
• A6550: Wound care set, for negative pressure wound therapy electrical pump, includes all supplies and
accessories, and
• A7000: Canister, disposable, used with suction pump, each.
- Negative pressure wound therapy (NPWT) is the controlled application of sub atmospheric pressure to a
wound using an electrical pump (described in the definition of HCPCS coded E2402) to intermittently or
continuously convey sub atmospheric pressure through connecting tubing to a specialized wound dressing
(A6550) which includes a resilient, open-cell foam surface dressing, sealed with an occlusive dressing that is
meant to contain the sub atmospheric pressure at the wound site and thereby promote wound healing.
Drainage from the wound is collected in a canister (A7000).
- A stationary or portable NPWT electrical pump provides controlled sub atmospheric pressure that is
designed for use with NPWT dressings to promote wound healing. Such a NPWT pump is capable of being
selectively switched between continuous and intermittent modes of operation and is controllable to adjust
the degree of sub atmospheric pressure conveyed to the wound in a range from 23 to greater than 200 mm
Hg sub atmospheric pressure. The pump is capable of sounding an audible alarm when desired pressures
are not being achieved (that is, where there is a leak in the dressing seal) and when the wound drainage
canister is full. The pump is designed to fill the canister to full capacity.
Staging of Pressure Ulcers
The staging of pressure ulcers in this policy is as follows:
Stage I: non-blanchable erythema of intact light toned skin or darker or violet hue in darkly pigmented skin.
Stage II: partial thickness skin loss involving epidermis and or dermis.
Stage III: full thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend down to,
but not through, underlying fascia.
Stage IV: full thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone, or
supporting structures.
General Coverage Criteria (for all wound types):
- Documentation of the history and previous treatment regimens must be maintained in the member’s
medical record and available upon request. This documentation must include such elements as dressing
types and frequency of change, changes in wound conditions (including precise measurements) quantity of
exudates, presence of granulation and necrotic tissue and concurrent measures being addressed relevant to
wound therapy (debridement, nutritional concerns, support surfaces in use, positioning, incontinence
control, etc.).
- Coverage will be considered when the member has a chronic Stage IV pressure ulcer, neuropathic (for
example, diabetic) ulcer, venous or arterial insufficiency ulcer, a non-healing surgically created or traumatic
wound, or a chronic (being present for at least 30 days) ulcer of mixed etiology. See below for diagnosis
specific coverage criteria.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
77
- A complete wound therapy program described below, as applicable depending on the type of wound,
should have been tried prior to application of NPWT. NPWT should be attempted first in a hospital or
another health care facility prior to discharge to the home setting. In these continuing cases,
documentation should reflect member compliance and pain management during application of NPWT.
- Prior approval will be required after the initial 30 days if an extension of the treatment is justified. In
addition, documentation of the availability of licensed medical professionals to perform dressing changes
and cleaning of the devices should be maintained and/or submitted for all cases.
Diagnosis Specific Coverage Criteria:
All ulcers or wounds:
1. Documentation in the member’s medical record of evaluation, care, and wound measurements by the
treating physician, and
2. Application of dressings to maintain a moist wound environment, and
3. Debridement of necrotic tissue if present, and
4. Evaluation of and provision for adequate nutritional status.
Stage IV pressure ulcers:
1. The member has been appropriately turned and positioned, and
2. The member has used a support surface for pressure ulcers and the posterior trunk or pelvis (not required if
the ulcer is not on the trunk or pelvis) and
3. The member’s moisture and incontinence have been appropriately managed.
Neuropathic (for example, diabetic) ulcers:
1. The member has been on a comprehensive diabetic management program, and
2. Reduction in pressure on a foot ulcer has been accomplished with appropriate modalities.
Venous insufficiency ulcers:
1. Compression bandages and/or garments have been consistently applied, and
2. Leg elevation and ambulation have been encouraged.
Non-healing surgically created or traumatic wounds:
1. Documentation of medical necessity for accelerated formation of granulated tissue which cannot be
achieved by other topical wound treatments.
Non-covered conditions:
- The presence in the wound of necrotic tissue with eschar if debridement is not attempted
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
78
- Untreated osteomyelitis within the vicinity of the wound
- Cancer present in the wound
- The presence of a fistula to an organ or body cavity within the vicinity of the wound
Documentation requirements (for continuation of services):
- Documentation of wound evaluation and treatment, recorded in the member’s medical record, must
indicate regular evaluation and treatment of the member’s wounds and must be available upon request.
- Documentation of quantitative measurements of wound characteristics including wound length and width
(surface area), and depth and amount of wound exudate (drainage), indicating progress of healing must be
entered at least weekly.
- If treatment beyond the initial approved period of service is indicated by the treating physician upon review
of the clinical progress, this documentation must be submitted with the new prior approval request. Lack of
improvement of a wound is defined as a lack of progress in quantitative measurements of wound
characteristics including wound length and width (surface area), or depth measured serially and
documented, over the approved period of service.
- Wound healing is defined as improvement occurring in either surface area or depth of the wound. If
detailed documentation is insufficient or if any measurable degree of wound healing has failed to occur,
prior approval beyond the initial approved period of service will not be granted.
Speech Generating Devices
Prior approval (PA) is the process of evaluating the request for Durable Medical Equipment (DME) in order to
determine the medical necessity and appropriateness of the DME according to policies and regulations. Requests for
PA are submitted through DME providers enrolled in New York State Medicaid. The DME provider is responsible for
submitting all necessary documentation required for the PA request in accordance with 18 New York State Codes,
Rules, and Regulations (“NYCRR”) Part 513. Please refer to Title: Section 513.0 Policy, purpose, and scope at
https://regs.health.ny.gov/content/section-5130-policy-purpose-and-scope for further information.
The following guidelines were developed to assist DME providers, ordering practitioners, Medicaid members,
caregivers, and evaluating clinicians with the PA process for Speech Generating Devices (SGD). The purpose of these
guidelines is to provide detailed coverage criteria for SGDs and accessories so that medically necessary equipment is
provided to Medicaid members in a timely manner in compliance with applicable Federal. Laws, policies and New York
State Codes, Rules, and Regulations. These guidelines are the product of collaboration with practitioners, therapists,
medical equipment providers, advocates, and New York State Medicaid medical review staff, utilizing state and national
standards and are the basis for compliance with applicable Medicaid policies.
As outlined in 18 NYCRR Section 513.0(b)(2), the Department retains the authority and responsibility to exercise
administrative discretion in the supervision of the program and make decisions with respect to the application of the
rules, regulations and policies of the Medicaid program.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
79
SGDs are one strategy used for augmentative alternative communication (AAC). AAC employs strategies to assist
individuals who are unable to effectively use their own speech to communicate. Successful use of a device requires the
ability to functionally communicate using the device’s output in addition to physical ability to activate and manipulate
the device. A detailed and individualized assessment of a person’s communication, cognitive, language, motor, and
visual abilities is required to determine which device will meet the person’s medical needs and abilities.
New York State Medicaid coverage includes only dedicated devices. Dedicated AAC devices are limited to primarily
serve a medical need (e.g., solely for the purpose of expressive communication) such that they are generally NOT
useful in the absence of disability, illness, or injury. Non-dedicated devices are non-medical devices designed for a
non-medical purpose and are generally useful in the absence of disability, illness, or injury; however, they may also
include functionality for use as a communication tool.
Coverage Guidelines
1) Speech Generating Devices (SGDs) and Related Accessories
An SGD will be considered medically necessary when documentation demonstrates all of the following:
a) The member has a severe expressive communication impairment related to a medical condition or
developmental disability that interferes with the member’s ability to meet daily functional communication,
AND;
b) The member’s ability to communicate using speech and/or writing is insufficient to meet daily functional
communication needs, AND;
c) The member cannot meet daily functional communication needs with any unaided means of
communication, AND;
d) The recommended device can be used to communicate with multiple individuals in multiple settings within
the trial location while conveying varying message types without being fully dependent on prompting or
assistance in producing the communication, AND;
e) The member has the cognitive, auditory, visual, language, and physical abilities to use the recommended
SGD for functional communication, AND;
f) A licensed Speech Language Pathologist (SLP) experienced in AAC service delivery has made the
recommendation for the device and a licensed physician, nurse practitioner, or physician’s assistant
enrolled as a NY State Medicaid provider has prescribed the device or software, AND;
g) The member has demonstrated the ability to use the recommended device and accessories or software for
functional communication as evidenced by a data-driven device trial showing that skills can be
demonstrated repeatedly over time, beyond a single instance or evaluation session, AND;
h) The SGD and related accessories are the adequate, less expensive alternative to enable the member to
meet daily functional communication needs. There must be clear explanation of why other alternatives
were ruled out. (See 18 NYCRR 513.4(d), AND
i) The SGD and related accessories must allow members to improve their communication to a functional
level not achievable without an SGD or less costly device.
2) Eye Control/Eye Gaze Accessory
An eye gaze accessory should be considered only after all other methods of accessing the SGD have been evaluated
and ruled out. The recommendation for an eye gaze accessory must be based on an assessment by the SLP and either
a PT or OT. Other professionals also may be needed for members who present additional issues, such as vision
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
80
impairment that interferes with the ability to use eye gaze to access a SGD. An eye gaze accessory will be considered
medically necessary when objective documentation demonstrates the following:
a) Scanning and head pointing systems have been tried repeatedly over time (within a single evaluation
session or in several sessions) were ruled out as not appropriate.
b) The member demonstrates abilities to use eye gaze technology beyond cause-and-effect activation,
simple eye tracking activities, and learning tools. A recent vision assessment may be required.
c) The member has the physical ability to activate the system and demonstrate meaningful/functional use of
the device without being fully dependent on prompting or assistance in producing the communication.
d) A data driven objective trial with the requested eye gaze access device has occurred.
e) Documentation shows that other eye gaze access devices from multiple manufacturers have been
considered.
f) The member can use the eye gaze technology to communicate significantly beyond the capabilities of a
light technology eye gaze system such as an eye gaze board or E-Tran system with less partner assistance.
g) A PT and/or OT with assistive technology (AT) experience has explored the member’s positioning needs
and head control abilities and all potential less costly access methods, including non-voice output eye
gaze boards.
3) Mounts
Mounts are used to secure SGDs for access and safety. Reimbursement is for one mount that meets the member’s
needs in all customary environments. Selection should be based on medical necessity and 18 NYCRR Section 513.4(d)
Indication for Non-Coverage of SGD
1) The member fails to demonstrate during the trial period or at any subsequent time the ability to learn to
use the device or software functionally for communication.
2) The requested device does not meet the member’s current and reasonably foreseeable communication
abilities and needs.
3) The intention is to unlock the device for uses other than communication or for use by other individuals.
4) The request includes reimbursement for the installation of the software/program or technical support of a
non-dedicated device. (Communication software/program is a covered benefit when all other coverage
criteria are met.)
5) The request is for reimbursement for a device or maintenance of a device (e.g. laptop, tablet) for which
Medicaid-funded communication software has been installed.
6) The request is for reimbursement for repairs of a device and the minimum coverage requirements for the
SGD are not met.
7) The request is for repairs, cleaning, or other services for non-dedicated communication devices.
8) The request is for an upgrade to new technology that is not medically necessary.
9) The request is for replacement of a device due to new technology or replacement based on a
manufacturer’s recommended replacement schedule when the member’s current SGD meets his/her
medical and functional communication needs.
10) The request is for multiple devices, back-up, or duplicate accessories.
11) The request is for environmental control devices such as switches and control boxes.
Documentation Requirements
Each SGD request is reviewed on an individual basis. Please refer to 18NYCRR Section 513.0(b)(2). Medicaid reserves the
right to request an evaluation of a member from another licensed medical professional, other than the SLP, for
supporting the appropriateness of the device being recommended. In addition to the specific requirements stated
below, the documentation submitted in support of a funding request for a SGD, mount or related accessories must

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
81
establish that all the standards stated in the Coverage Guidelines are met. Documentation submitted should include
the following:
1) Detailed Fiscal Order including the make and model of equipment requested (see “Filling Orders for DMEPOS
at https://www.emedny.org/ProviderManuals/DME/PDFS/DME_Policy_Section.pdf)
2) A cost quote from the manufacturer of all the equipment and components as ordered (e.g., make, model).
Include the usual and customary price charged to the general public and all dealer discounts.
3) Individualized Education Plan (IEP) for school aged members
4) Formal face to face evaluation and assessment written by a SLP within 6 months prior to the date of PA
submission that includes:
a) Background information
i. Medical diagnosis; course and prognosis
ii. Significant history and medications
iii. Communication disorder(s)/diagnosis and severity; course and prognosis
iv. Past speech/ spoken language treatment
v. Member’s history, school, vocational status
vi. Member’s living environment
vii. Members’ attitude and motivation to communicate
b) Current communication abilities
i. Speech/articulation and intelligibility
ii. Expressive language skills
iii. Receptive language skills
iv. Current mode of communication including nonverbal communication methods
v. Current method of communicating pain, discomfort, or other medical emergencies
vi. Previous use of AAC including devices, dates utilized, and explanation why the currently used
device does not meet the member’s current and reasonably foreseeable daily functional
communication needs.
vii. Currently used functions of communication (e.g. requesting, protesting, commenting, describing,
etc.),
viii. Reading, writing, and spelling abilities
c) Sensory functioning
i. visual abilities (e.g. tracking ability, acuity for symbol size, etc.)

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
82
ii. auditory abilities as they relate to an SGD system
d) Psychometric or developmental assessment characterizing cognitive and learning abilities and levels of
function (include results of most recent evaluation, name of test, IQ or developmental levels, and date
performed). NOTE: Members who do not exhibit cognitive deficits may not need to participate in assessments,
however Medicaid reserves the right to request additional documentation regarding cognitive functioning
after initial review of PA submission.
e) Behavioral and Learning abilities:
i. Executive-functioning skills, including attention span
ii. Memory
iii. Problem solving skills
iv. Understanding of cause and effect
f) Motor abilities
i. Gross motor abilities: ambulatory, uses walker or wheelchair, head control and trunk mobility.
ii. Positioning and Seating: current DME used, positioning needs as related to SGD use including eye
gaze access if necessary (including primary positions in which the member spends a typical day
and percentage of time in each position).
iii. Fine Motor and upper extremity abilities and functional use (including strength and endurance for
carrying SGD).
iv. Alternative access (except for access via gaze), e.g., head mouse, single switch or multiple switch
scanning, or other alternative access method) should be evaluated by a PT, OT, or other health
professional when necessary.
g) Formal evaluation of AAC by evaluating SLP
i. Description of need, short and long-term goals for device use; primary communication partners;
current and reasonably foreseeable communication environments.
ii. Treatment options considered including past use of communication supports and why each does
not meet the member’s communication needs.
iii. Description of consideration of more than one device by multiple manufacturers within the same
HCPCS category that includes explanation of why devices were selected or ruled out.
iv. Data driven AAC device trial of the recommended device. The following items should be
addressed:
1) Length and dates of trial, amount of time device was accessed during the trial.
2) Time framed measurable goals for functional communication set for trial and criteria for
measurement.
3) Empirical data including baseline performance and results of trial period goals.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
83
4) Description of environments in which device was trialed such as, but not limited to, home, school,
and community.
5) Whether communication occurred in both structured and unstructured settings.
6) Manner in which the device was accessed (e.g. eye gaze, direct selection, scanning-type)
7) Description of the member’s ability to use the SGD for functional communication (ability to use
training software, including but not limited to cause-and-effect games does not demonstrate
functional communication).
8) Sampling of multiple messages communicated including the frequency, type (e.g. verbal, physical,
gesture), and level of cueing required.
9) Number of messages expressed in a time period including the type and level of cueing required.
10) Communicative intents and functions expressed.
11) If recommending eye gaze access: the member’s endurance to maintain gaze, ability to calibrate or
obstacles to calibration.
v. Description and rationale for the software or language system recommended including specific
page sets/layout/symbols per page/vocabulary organization.
vi. Description of recommended device; the rationale for the selection including a cost comparison
among devices considered from more than one manufacturer; and how the recommendation
meets the current communication needs of member.
vii. Description of environmental supports for SGD use: capacity of family/caregivers/friends to assist
in care and maintenance of SGD; need for their training.
viii. Documentation that device is configured to limit use to the purpose of communication.
ix. Explanation of how the device is the adequate, less expensive alternative to meet the member’s
medical need.
h) Outline of a training and implementation plan that will be used to ensure the most appropriate use of the
device over time, including plans for maintaining the system, implementing programming updates and
modifications due to changing language, environmental, or motoric needs.
i) A signed and dated attestation by the SLP that the licensed/certified medical professional (LCMP) has no
financial relationship with the Medicaid provider or SGD manufacturer.
j) Dated signature of SLP, license number and pertinent contact information.
k) All other professionals directly involved in the evaluation should sign, date, and provide their license numbers.
Documentation for Consideration for Coverage of:
1) Upgrade
The Medicaid-funded or member-owned device is no longer clinically effective at meeting functional communication
needs. Documentation must include:
a) Statement addressing why the device is no longer clinically effective in meeting member’s functional
communication needs.
b) Statement of significant changes that have occurred in the member’s physical or linguistic abilities, or
social environment, and how these changes impact the member’s ability to functionally communicate with
the currently owned device.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
84
c) Establish why the replacement device is required (not solely due to advances in technology or other
factors that are not medical in nature).
2) Repairs
a) The minimum coverage criteria for SGDs are met.
b) The request includes a quote from the manufacturer of the initially covered device for the cost of the
repairs (The decision whether to repair or replace a device will be based on a determination of which will
be most cost effective.)
c) When repair is required due to accidental or non-accidental trauma to the device, the SLP or ordering
Physician must provide a statement indicating the cause of damage and what reasonable measures will be
taken to prevent a recurrence.
The reimbursement for a new SGD includes all necessary screen protectors, batteries, power source components,
software, stands (not including mounts: e.g. wheelchair or desk mounts) and any type of carrying case.
E2500
F2
‘-RR’
#Speech generating device, digitized speech, using pre-recorded messages, less than or equal
to 8 minutes recording time
E2502
F2
‘-RR’
#Speech generating device, digitized speech, using pre-recorded messages, greater than 8
minutes but less than or equal to 20 minutes recording time
E2504
F2
‘-RR’
#Speech generating device, digitized speech, using pre-recorded messages, greater than 20
minutes but less than or equal to 40 minutes recording time
E2506
F2
‘-RR’
#Speech generating device, digitized speech, using pre-recorded messages, greater than 40
minutes recording time
E2508
F2
‘-RR’
#Speech generating device, synthesized speech, requiring message formulation by spelling and
access by physical contact with the device
E2510
F2
Speech generating device, synthesized speech, permitting multiple methods of message
formulation and multiple methods of device access
E2511
F2
Speech generating software program, for personal computer or personal digital assistant
E2512
F3
Accessory for speech generating device, mounting system
E2599
F3
Accessory for speech generating device, not otherwise classified
References
- American Speech-Language Hearing Association (ASHA) Practice Portal: Augmentative and Alternative
Communication available at
http://www.asha.org/PRPSpecificTopic.aspx?folderid=8589942773§ion=Key_Issues
.
- ASHA Position Statement on Access to Communication Services and Supports: Concerns Regarding the
Application of Restrictive “Eligibility” Policies available at http://www.asha.org/policy/PS2003-00227/
.
- ASHA Medical Necessity for Speech-Language Pathology and Audiology Services available at
https://www.asha.org/practice/reimbursement/medical-necessity-for-audiology-and-SLP-services/
- MassHealth Guidelines for Medical Necessity Determination for Augmentative and Alternative
Communication Devices and Speech Generation Devices.
https://www.mass.gov/doc/guidelines-for-
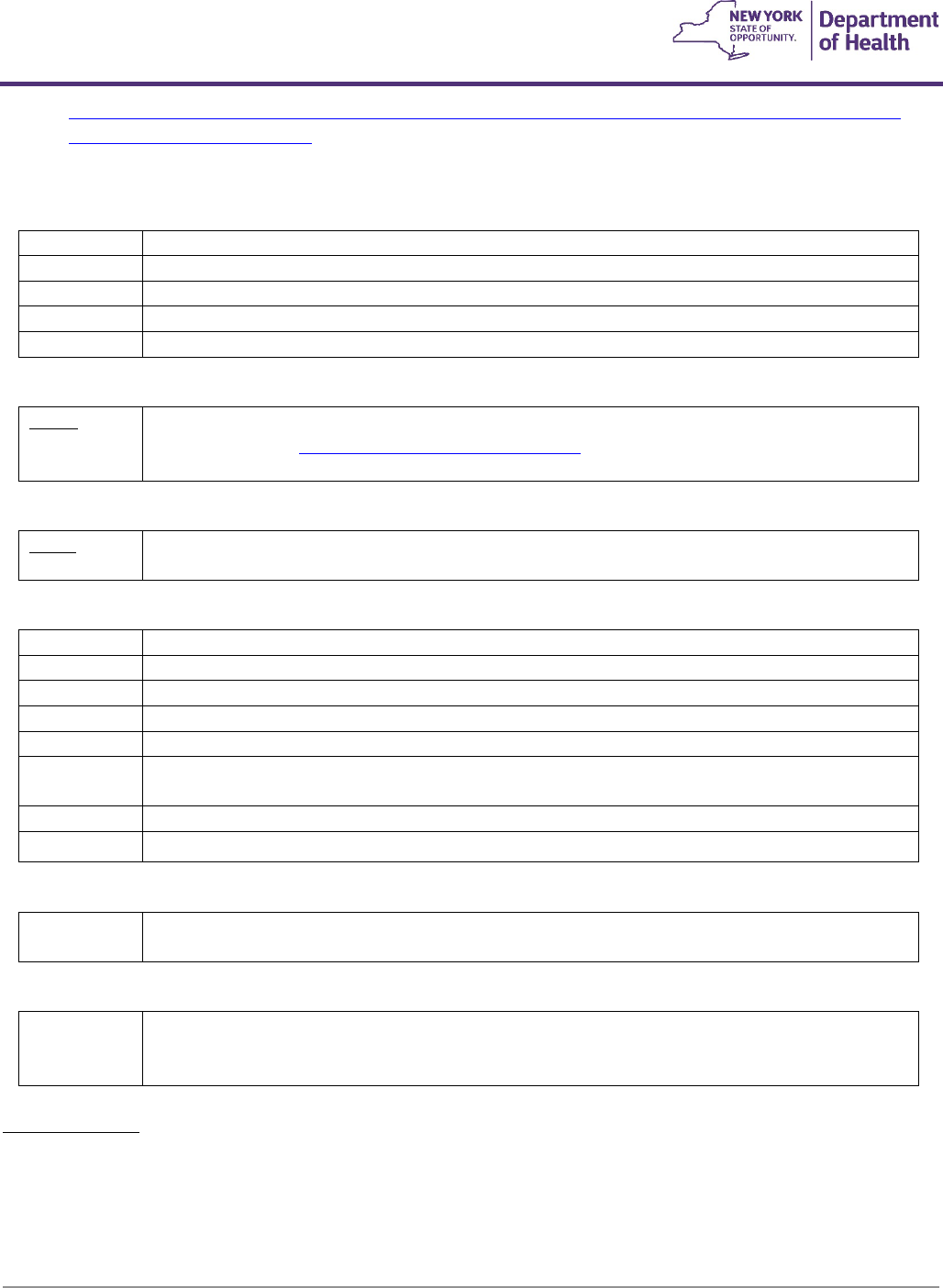
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
85
medical-necessity-determination-for-augmentative-and-alternative-communication-devices-including-
speech-generating-devices-1/
External Infusion Pump Batteries
K0601
F8
#Replacement battery for external infusion pump owned by patient, silver oxide, 1.5 volt, each
K0602
F8
#Replacement battery for external infusion pump owned by patient, silver oxide, 3 volt, each
K0603
F8
#Replacement battery for external infusion pump owned by patient, alkaline, 1.5 volt, each
K0604
F8
#Replacement battery for external infusion pump owned by patient, lithium, 3.6 volt, each
K0605
F8
#Replacement battery for external infusion pump owned by patient, lithium, 4.5 volt, each
Automatic External Defibrillator
K0606
F9
Automatic external defibrillator, with integrated electrocardiogram analysis, garment type
See following link: K0606 General Coverage Guidelines
*Reimbursement is prorated based on daily use of 20 hours or more
Vacuum Erection Device
L7900
F2
Vacuum erection system
Limited to diagnosis of impotence, with an order from a urologist or neurologist
Larynx and Trachea Prosthetics and Accessories
L8500
F2
#Artificial larynx, any type
L8501
F7
#Tracheostomy speaking valve
L8505
F7
#Artificial larynx replacement battery/accessory, any type
L8507
F10
Tracheo-esophageal voice prosthesis, patient inserted, any type, each
L8510
F3
#Voice amplifier
L8511
F7
#Insert for indwelling tracheoesophageal prosthesis, with or
without valve, replacement only, each
L8514
F7
#Tracheoesophageal puncture dilator, replacement only, each
L8515
F5
#Gelatin capsule, application device for use with tracheoesophageal voice prosthesis, each
Enuresis Alarm
S8270
F1
#Enuresis alarm, using auditory buzzer and/or vibration device (Prior approval required over
age 20)
Positioning Car Seat
T5001
F2
#Positioning seat for persons with special orthopedic needs,
(Adjustable, for use in vehicles, able to accommodate users up to 60 inches, prior approval
required for ages less than 2 or over 10)
Coverage Criteria
- Member's postural needs cannot be safely met by less costly alternatives such as the vehicles restraint
system or other restraint systems such as an EZ on vest.
- Member's size or postural support needs restricts the use of a standard/commercially available car seat.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
86
- Car seat is used in the primary caregiver’s personal vehicle.
Reimbursement amount includes the following features/accessories (any type/size):
• Head support
• Trunk positioning pads/supports
• Harness or safety belts (with or without safety cover)
• Abductor pommel
• Any positioning wedges, cushions, or padding
• Tilt and/or recline (fixed or adjustable)
• All LATCH/tether straps
Additional, medically necessary accessories will require prior approval under miscellaneous code E1399.
SERVICING, PARTS, REPAIRS
- Repair requests must include, at minimum; the specific part(s) being requested with associated cost quote(s) or
invoice(s), list of other repairs being provided not requiring prior approval and anticipated useful life of the
device with the requested repairs. If NYS Medicaid did not fund the device originally and this is the first repair
request submitted for paper prior approval, the device’s serial number, date provided, funding source, and
original supporting documentation must be provided.
HCPCS Codes, RB modifier, K0739
a) For replacement parts that have a specific HCPCS code:
1. Report the replacement part code, and
2. Report K0739 for labor component.
b) For replacement parts to base equipment with a specific HCPCS code:
1. Report the base equipment code with the -RB modifier (e.g., wheelchair base code with -RB, hospital
bed code with -RB), for the replacement part(s) and
2. Report K0739 for the labor component.
c) For miscellaneous DME with no specific or base code to report:
1. Report the appropriate miscellaneous code, E1399 or K0108 or A9900 with the –RB modifier for the
replacement part(s), and
2. Report K0739 for labor component.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
87
d) The fee for K0739 Repair or non-routine service for durable medical equipment requiring the skill of a
technician, labor component, per 15 minutes (more than 2 hours requires prior approval) is $18.00.
e) Payment for pick-up and delivery of DME for repair is included in the payment for replacement equipment and
parts.
f) Repairs (labor, replacement equipment and parts) covered under the manufacturer’s warranty are not to be
billed to Medicaid.
g) When labor is performed by a manufacturer; Medicaid pays the Medicaid DMEPOS provider the line-item
labor cost on the manufacturer’s invoice and the applicable Medicaid fee for the parts. If labor and parts
charges are not separately itemized on the manufacturer invoice as required by 18NYCRR505.5, the DMEPOS
provider will be paid the invoice cost of parts and labor.
A9900
F7
Miscellaneous DME supply, accessory, and/or service component of another HCPCS code
A9999
Miscellaneous DME supply or accessory, not otherwise specified
K0739
F9
#Repair or non routine service for Durable Medical Equipment other than oxygen equipment
requiring the skill of a technician, labor component, per 15 minutes
(more than 2 hours requires
prior approval)
4.5 Orthotics
General Coverage Criteria
1. This schedule is applicable to both children and adults.
2. Base codes are covered when the physician’s order and supporting documentation clearly establish the
medical and functional need being met by the prescribed device. Where applicable, code specific coverage
criteria must be met.
3. L Code “additions” are covered only when both the base codes coverage criteria have been met and specific
documentation exists establishing the medical necessity of the addition code.
4. When providing a custom fabricated device, the documentation should establish specific reason(s) why a
prefabricated alternative was not medically indicated. This should include, where applicable, the
documented failure of prefabricated alternatives. A prefabricated orthosis is one which is manufactured in
quantity without a specific member in mind. It is pre-formed with a shape that generally conforms to the
body part. A prefabricated orthosis may be trimmed, bent, molded (with or without heat), or otherwise
modified for use by a specific member (i.e.: custom fitted). A custom fabricated orthosis is one which is
individually made for a specific member (no other patient would be able to use this orthosis) starting with
basic materials including, but not limited to, plastic, metal, leather, or cloth in the form of sheets, bars, etc.
5. The providers shall be responsible for any needed repairs or replacements due to defects in quality or
workmanship that appear within three months of delivery. This does not include adjustments or
replacements necessitated by anatomical changes.
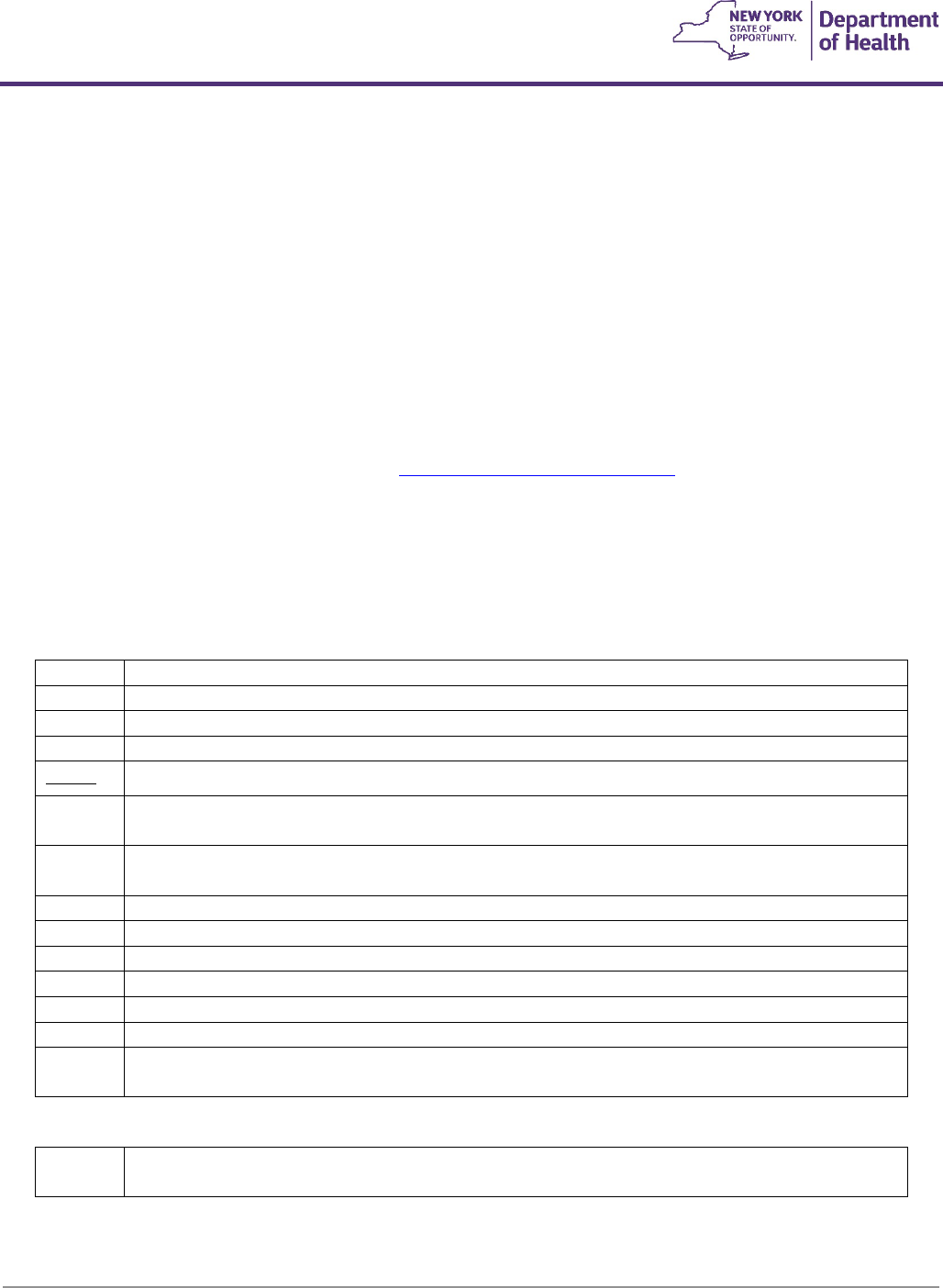
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
88
6. Replacements and repairs: used to indicate replacement and repair of orthotic and prosthetic devices which
have been in use for some time. Prior approval is not required when the charge is over $35.00 and is less
than 25% of the price listed on the code for the device. When specific replacement and repair codes are
available, they should be used instead of the code for the device with ‘-RB’. For charges $35.00 and under,
use L4210.
7. The fees contained in this schedule will be paid under State-administered programs and are to be
considered full payment for the services rendered. The provider shall make no additional charge to the
member.
8. Unless otherwise specified all fees are for the unilateral, single unit or “each.”
9. All normal necessary pads, straps and stops are included in the prices quoted.
10. Consideration for coverage of Functional Electrical Stimulation devices (e.g.: foot drop systems) is limited to
qualifying conditions. Please refer to the September 2013 Medicaid Update
for specific coverage guidance.
Qualifying devices submitted for prior approval should be billed using HCPCS code E1399. Please note,
replacement accessories (e.g.: A4556 electrodes, A4557 lead wires) are only to be billed for covered FES
devices.
Orthotic Devices Spinal
Cervical
A8000
F6
#Helmet, protective, soft, prefabricated, includes all components and accessories
A8001
F6
#Helmet, protective, hard, prefabricated, includes all components and accessories
A8002
F6
#Helmet, protective, soft, custom fabricated, includes all components and accessories
A8003
F6
#Helmet, protective, hard, custom fabricated, includes all components and accessories
A8004
F6
Soft interface for helmet, replacement only
L0112
F3
#Cranial cervical orthosis, congenital torticollis type, with or without soft interface material,
adjustable range of motion joint, custom fabricated
L0113
F3
#Cranial cervical orthosis, torticollis type, with or without joint, with or without soft interface
material, prefabricated, includes fitting and adjustment
L0130
F3
#Cervical, flexible, thermoplastic collar, molded to patient
L0140
F3
#Cervical, semi-rigid, adjustable (plastic collar)
L0150
F3
#Cervical, semi-rigid, adjustable molded chin cup (plastic collar with mandibular/occipital piece)
L0160
F3
#Cervical, semi-rigid, wire frame occipital/mandibular support, prefabricated, off-the-shelf
L0170
F3
#Cervical, collar, molded to patient model
L0172
F3
#Cervical, collar, semi-rigid thermoplastic foam, two-piece, prefabricated, off-the-shelf
L0174
F3
#Cervical, collar, semi-rigid, thermoplastic foam, two piece with thoracic extension,
prefabricated, off-the-shelf
Cranial Remolding Orthosis
S1040
F1
#Cranial remolding orthosis, rigid, with soft interface material, custom fabricated, includes fitting
and adjustment(s)
Covered when:

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
89
- The member has moderate to severe positional head deformities associated with premature birth,
restrictive intrauterine positioning, cervical abnormalities, birth trauma, torticollis and/or sleeping positions
in children.
- Anthropometric measurements verify that a moderate to severe plagiocephaly is documented by a
physician experienced in such measurements.
- The member is between the ages of 3-18 months old and is considered to have a reasonable likelihood of
continued skull growth.
- There is documentation of, at minimum, a 2-month trial of repositioning and stretching exercises as follows:
1. Alternating back and side sleeping
2. Supervised tummy time
3. Rearranging the crib relative to the primary light source
4. Limiting time spent in a supine position
5. Limiting time in strollers, carriers, and swings
6. Rotating chair activity
7. Neck motion exercises
- The member has a diagnosis of craniosynostosis and has had surgical intervention of either calvarial vault
reconstruction or minimally invasive, endoscopic-assisted craniectomy.
Not covered for:
- Members over the age of 24 months.
- Unmanaged hydrocephalus.
- Craniosynostosis (without surgical intervention).
Documentation requirements:
- A valid fiscal order signed by a pediatrician, a general surgeon with specialty in pediatrics, and/or a
craniofacial surgeon.
- Anthropometric measurements.
- Documentation of medical necessity from a pediatric neurosurgeon or a craniofacial surgeon.
Documented trial of repositioning and stretching exercises as outlined above.
Multiple Post Collar
L0180
F3
#Cervical, multiple post collar, occipital/mandibular supports, adjustable
L0190
F3
#Cervical, multiple post collar, occipital/mandibular supports, adjustable cervical bars (Somi,
Guilford, Taylor types)
L0200
F3
#Cervical, multiple post collar, occipital/mandibular supports, adjustable cervical bars, and
thoracic extension
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
90
Thoracic
L0220
F6
#Thoracic, rib belt, custom fabricated
Thoracic-Lumbar-Sacral Orthosis (TLSO)
Covered when ordered for the following indications:
1. To reduce pain by restricting mobility of the trunk; or
2. To facilitate healing following an injury, or surgical procedure, to the spine or related soft tissues; or
3. To support weak spinal muscles and/or a spinal deformity.
L0450
F4
#TLSO, flexible, provides trunk support, upper thoracic region, produces intracavitary pressure
to reduce load on the intervertebral disks with rigid stays or panel(s), includes shoulder straps
and closures, prefabricated, off-the-shelf
L0452
F4
#TLSO, flexible, provides trunk support, upper thoracic region, produces intracavitary pressure
to reduce load on the intervertebral disks with rigid stays or panel(s), includes shoulder straps
and closures, custom fabricated
L0454
F4
#TLSO, flexible, provides trunk support, extends from sacrococcygeal junction to above T-9
vertebra, restricts gross trunk motion in the sagittal plane, produces intracavitary pressure to
reduce load on the intervertebral disks with rigid stays or panel(s), includes shoulder straps and
closures, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise
customized to fit a specific patient by an individual with expertise
L0455
F4
#TLSO, flexible, provides trunk support, extends from sacrococcygeal junction to above T-9
vertebra, restricts gross trunk motion in the sagittal plane, produces intracavitary pressure to
reduce load on the intervertebral disks with rigid stays or panel(s), includes shoulder straps and
closures, prefabricated, off-the-shelf
L0456
F4
#TLSO, flexible, provides trunk support, thoracic region, rigid posterior panel and soft anterior
apron, extends from the sacrococcygeal junction and terminates just inferior to the scapular
spine, restricts gross trunk motion in the sagittal plane, produces intracavitary pressure to
reduce load on the intervertebral disks, includes straps and closures, prefabricated item that has
been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an
individual with expertise
L0457
F4
#TLSO, flexible, provides trunk support, thoracic region, rigid posterior panel and soft anterior
apron, extends from the sacrococcygeal junction and terminates just inferior to the scapular
spine, restricts gross trunk motion in the sagittal plane, produces intracavitary pressure to
reduce load on the intervertebral disks, includes straps and closures, prefabricated, off-the-shelf
L0458
F4
#TLSO, triplanar control, modular segmented spinal system, two rigid plastic shells, posterior
extends from the sacrococcygeal junction and terminates just inferior to the scapular spine,
anterior extends from the symphysis pubis to the xiphoid, soft liner, restricts gross trunk motion
in the sagittal, coronal, and transverse planes, lateral strength is provided by overlapping plastic
and stabilizing closures, includes straps and closures, prefabricated, includes fitting and
adjustment
L0460
F4
#TLSO, triplanar control, modular segmented spinal system, two rigid plastic shells, posterior
extends from the sacrococcygeal junction and terminates just inferior to the scapular spine,
anterior extends from the symphysis pubis to the sternal notch, soft liner, restricts gross trunk
motion in the sagittal, coronal, and transverse planes, lateral strength is provided by overlapping
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
91
plastic and stabilizing closures, includes straps and closures, prefabricated item that has been
trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an
individual with expertise
L0462
F4
#TLSO, triplanar control, modular segmented spinal system, three rigid plastic shells, posterior
extends from the sacrococcygeal junction and terminates just inferior to the scapular spine,
anterior extends from the symphysis pubis to the sternal notch, soft liner, restricts gross trunk
motion in the sagittal, coronal, and transverse planes, lateral strength
is provided by overlapping plastic and stabilizing closures, includes straps and closures,
prefabricated, includes fitting and adjustment
L0464
F4
#TLSO, triplanar control, modular segmented spinal system, four rigid plastic shells, posterior
extends from sacrococcygeal junction and terminates just inferior to scapular spine, anterior
extends from symphysis pubis to the sternal notch, soft liner, restricts gross trunk motion in the
sagittal, coronal, and transverse planes, lateral strength is provided by overlapping plastic and
stabilizing closures, prefabricated, includes fitting and adjustment
L0466
F4
#TLSO, sagittal control, rigid posterior frame and flexible soft anterior apron with straps,
closures and padding, restricts gross trunk motion in sagittal plane, produces intracavitary
pressure to reduce load on intervertebral disks, includes fitting and shaping the frame,
prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized
to fit a specific patient by an individual with expertise
L0467
F4
#TLSO, sagittal control, rigid posterior frame and flexible soft anterior apron with straps,
closures and padding, restricts gross trunk motion in sagittal plane, produces intracavitary
pressure to reduce load on intervertebral disks, prefabricated, off-the-shelf
L0468
F4
#TLSO, sagittal-coronal control, rigid posterior frame and flexible soft anterior apron with straps,
closures and padding, extends from sacrococcygeal junction over scapulae, lateral strength
provided by pelvic, thoracic, and lateral frame pieces, restricts gross trunk motion in sagittal, and
coronal planes, produces intracavitary pressure to reduce load on intervertebral disks, includes
fitting and shaping the frame, prefabricated item that has been trimmed, bent, molded,
assembled, or otherwise customized to fit a specific patient by an individual with expertise
L0469
F4
#TLSO, sagittal-coronal control, rigid posterior frame and flexible soft anterior apron with straps,
closures and padding, extends from sacrococcygeal junction over scapulae, lateral strength
provided by pelvic, thoracic, and lateral frame pieces, restricts gross trunk motion in sagittal and
coronal planes, produces intracavitary pressure to reduce load on intervertebral disks,
prefabricated, off-the-shelf
L0470
F4
#TLSO, triplanar control, rigid posterior frame and flexible soft anterior apron with straps,
closures and padding, extends from sacrococcygeal junction to scapula, lateral strength
provided by pelvic, thoracic, and lateral frame pieces, rotational strength provided by
subclavicular extensions, restricts gross trunk motion in sagittal, coronal, and transverse planes,
produces intracavitary pressure to reduce load on the intervertebral disks, includes filling and
shaping the frame, prefabricated, includes fitting and adjustment
L0472
F4
#TLSO, triplanar control, hyperextension, rigid anterior and lateral frame extends from
symphysis pubis to sternal notch with two anterior components (one pubic and one sternal),
posterior and lateral pads with straps and closures, limits spinal flexion, restricts gross trunk
motion in sagittal, coronal, and transverse planes, includes fitting and shaping the frame,
prefabricated, includes fitting and adjustment
L0480
F6
#TLSO, triplanar control, one piece rigid plastic shell without interface liner, with multiple straps
and closures posterior extends from sacrococcygeal junction and terminates just inferior to
scapular spine, anterior extends from symphysis pubis to sternal notch, anterior or posterior
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
92
opening, restricts gross trunk motion in sagittal, coronal, and transverse planes, includes a
carved plaster or CAD-CAM model, custom fabricated
L0482
F6
#TLSO, triplanar control, one piece rigid plastic shell with interface liner, multiple straps and
closures, posterior extends from sacrococcygeal junction and terminates just inferior to scapular
spine, anterior extends from symphysis pubis to sternal notch, anterior or posterior opening,
restricts gross trunk motion in sagittal, coronal, and transverse planes, includes a carved plaster
or CAD-CAM model, custom fabricated
L0484
F6
#TLSO, triplanar control, two piece rigid plastic shell without interface liner, with multiple straps
and closures, posterior extends from sacrococcygeal junction and terminates just inferior to
scapular spine, anterior extends from symphysis pubis to sternal notch, lateral strength is
enhanced by overlapping plastic, restricts gross trunk motion in the sagittal, coronal, and
transverse planes, includes a carved plaster or CAD-CAM model, custom fabricated
L0486
F6
#TLSO, triplanar control, two piece rigid plastic shell with interface liner, multiple straps and
closures, posterior extends from sacrococcygeal junction and terminates just inferior to scapular
spine, anterior extends from symphysis pubis to sternal notch, lateral strength is enhanced by
overlapping plastic, restricts gross trunk motion in the sagittal, coronal, and transverse planes,
includes a carved plaster or CAD-CAM model, custom fabricated
L0488
F6
#TLSO, triplanar control, one piece rigid plastic shell with interface liner, multiple straps and
closures, posterior extends from sacrococcygeal junction and terminates just inferior to scapular
spine, anterior extends from symphysis pubis to sternal notch, anterior or posterior opening,
restricts gross trunk motion in sagittal, coronal, and transverse planes, prefabricated, includes
fitting and adjustment
L0490
F6
#TLSO, sagittal-coronal control, one piece rigid plastic shell, with overlapping reinforced
anterior, with multiple straps and closures, posterior extends from symphysis pubis to xiphoid,
anterior opening, restricts gross trunk motion in sagittal and coronal planes, prefabricated,
includes fitting and adjustment
L0491
F4
#TLSO, sagittal-coronal control, modular segmented spinal system, two rigid plastic shells,
posterior extends from the sacrococcygeal junction and terminates just inferior to the scapular
spine, anterior extends from the symphysis pubis to the xiphoid, soft liner, restricts gross trunk
motion in the sagittal and coronal planes, lateral strength is provided by overlapping plastic and
stabilizing closures, includes straps and closures, prefabricated, includes fitting and adjustment
L0492
F4
#TLSO, sagittal-coronal control, modular segmented spinal system, three rigid plastic shells,
posterior extends from the sacrococcygeal junction and terminates just inferior to the scapular
spine, anterior extends from the symphysis pubis to the xiphoid, soft liner, restricts gross trunk
motion in the sagittal and coronal planes, lateral strength is provided by overlapping plastic and
stabilizing closures, includes straps and closures, prefabricated, includes fitting and adjustment
Cervical-Thoracic-Lumbar-Sacral Orthosis (CTLSO)
L0621
F4
#Sacroiliac orthosis, flexible, provides pelvic-sacral support, reduces motion about the sacroiliac
joint, includes straps, closures, may include pendulous abdomen design, prefabricated, off-the-
shelf
L0622
F4
#Sacroiliac orthosis, flexible, provides pelvic-sacral support, reduces motion about the sacroiliac
joint includes straps, closures, may include pendulous abdomen design, custom fabricated
L0623
F4
#Sacroiliac orthosis provides pelvic-sacral support, with rigid or semi-rigid panels over the
sacrum and abdomen, reduces motion about the sacroiliac joint, includes straps, closures, may
include pendulous abdomen design, prefabricated, off-the-shelf

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
93
L0624
F4
#Sacroiliac orthosis provides pelvic-sacral support, with rigid or semi-rigid panels placed over
the sacrum and abdomen, reduces motion about the sacroiliac joint, includes straps, closures,
may include pendulous abdomen design, custom fabricated
Lumbar Orthosis
Covered when ordered for the following indications:
1. To reduce pain by restricting mobility of the trunk; or
2. To facilitate healing following an injury, or surgical procedure, to the spine or related soft tissues; or
3. To support weak spinal muscles and/or a spinal deformity.
L0625
F4
#Lumbar Orthosis, flexible, provides lumbar support, posterior extends from L-1 to below L-5
vertebra, produces intracavitary pressure to reduce load on the intervertebral discs, includes
straps, closures, may include pendulous abdomen design, shoulder straps, stays, prefabricated,
off-the-shelf
L0626
F4
#Lumbar Orthosis, sagittal control, with rigid posterior panel(s), posterior extends from L-1 to
below L-5 vertebra, produces intracavitary pressure to reduce load on the intervertebral discs,
includes straps, closures, may include padding, stays, shoulder straps, pendulous abdomen
design, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise
customized to fit a specific patient by an individual with expertise
L0627
F4
#Lumbar Orthosis, sagittal control, with rigid anterior and posterior panels, posterior extends
from L-1 to below L-5 vertebra, produces intracavitary pressure to reduce load on the
intervertebral discs, includes straps, closures, may include padding, shoulder straps, pendulous
abdomen design, prefabricated item that has been trimmed, bent, molded, assembled, or
otherwise customized to fit a specific patient by an individual with expertise
L0641
F4
#Lumbar orthosis, sagittal control, with rigid posterior panel(s), posterior extends from L-1 to
below L-5 vertebra, produces intracavitary pressure to reduce load on the intervertebral discs,
includes straps, closures, may include padding, stays, shoulder straps, pendulous abdomen
design, prefabricated, off-the-shelf
L0642
F4
#Lumbar orthosis, sagittal control, with rigid anterior and posterior panels, posterior extends
from L-1 to below L-5 vertebra, produces intracavitary pressure to reduce load on the
intervertebral discs, includes straps, closures, may include padding, shoulder straps, pendulous
abdomen design, prefabricated, off-the-shelf
Lumbar-Sacral Orthosis
Covered when ordered for the following indications:
1. To reduce pain by restricting mobility of the trunk; or
2. To facilitate healing following an injury, or surgical procedure, to the spine or related soft tissues; or
3. To support weak spinal muscles and/or a spinal deformity.
L0628
F4
#Lumbar sacral orthosis, flexible, provides lumbo-sacral support, posterior extends from
sacrococcygeal junction to T-9 vertebra, produces intracavitary pressure to reduce load on the
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
94
intervertebral discs, includes straps, closures, may include stays, shoulder straps, pendulous
abdomen design, prefabricated, off-the-shelf
L0629
F4
#Lumbar sacral orthosis, flexible, provides lumbo-sacral support, posterior extends from
sacrococcygeal junction to T-9 vertebra, produces intracavitary pressure to reduce load on the
intervertebral discs, includes straps,
closures, may include stays, shoulder straps, pendulous abdomen design, custom fabricated
L0630
F4
#Lumbar sacral orthosis, sagittal control, with rigid posterior panel(s), posterior extends from
sacrococcygeal junction to T-9 vertebra, produces intracavitary pressure to reduce load on the
intervertebral discs, includes straps, closures, may include padding, stays, shoulder straps,
pendulous abdomen design, prefabricated item that has been trimmed, bent, molded,
assembled, or otherwise customized to fit a specific patient by an individual with expertise
L0631
F4
#Lumbar sacral orthosis, sagittal control, with rigid anterior and posterior panels, posterior
extends from sacrococcygeal junction to T-9 vertebra, produces intracavitary pressure to reduce
load on the intervertebral discs, includes straps, closures, may include padding, shoulder straps,
pendulous abdomen design, prefabricated item that has been trimmed, bent, molded,
assembled, or otherwise customized to fit a specific patient by an individual with expertise
L0632
F4
#Lumbar sacral orthosis, sagittal-coronal control, with rigid anterior and posterior panels,
posterior extends from sacrococcygeal junction to T-9 vertebra, produces intracavitary pressure
to reduce load on the intervertebral discs, includes straps, closures, may include padding,
shoulder straps, pendulous abdomen design, custom fabricated
L0633
F4
#Lumbar sacral orthosis, sagittal-coronal control, with rigid posterior frame/panel(s), posterior
extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by rigid lateral
frame/panels, produces intracavitary pressure to reduce load on intervertebral discs, includes
straps, closures, may include padding, stays, shoulder straps, pendulous abdomen design,
prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized
to fit a specific patient by an individual with expertise
L0634
F4
#Lumbar sacral orthosis, sagittal-coronal control, with rigid posterior frame/panel(s), posterior
extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by rigid lateral
frame/panels, produces intracavitary pressure to reduce load on intervertebral discs, includes
straps, closures, may include padding, stays, shoulder straps, pendulous abdomen design,
custom fabricated
L0635
F4
#Lumbar sacral orthosis, sagittal-coronal control, lumbar flexion, rigid posterior frame/panels,
lateral articulating design to flex the lumbar spine, posterior extends from sacrococcygeal
junction to T-9 vertebra, lateral strength provided by rigid lateral frame/panels, produces
intracavitary pressure to reduce load on intervertebral discs, includes straps, closures, may
include padding, anterior panel, pendulous abdomen design, prefabricated, includes fitting and
adjustment
L0636
F4
#Lumbar sacral orthosis, sagittal-coronal control, lumbar flexion, rigid posterior frame/panels,
lateral articulating design to flex the lumbar spine, posterior extends from sacrococcygeal
junction to T-9 vertebra, lateral strength provided by rigid lateral frame/panels, produces
intracavitary pressure to reduce load on intervertebral discs, includes straps, closures, may
include padding, anterior panel, pendulous abdomen design, custom fabricated
L0637
F4
#Lumbar sacral orthosis, sagittal-coronal control, with rigid anterior and posterior frame/panels,
posterior extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by
rigid lateral frame/panels, produces intracavitary pressure to reduce load on intervertebral discs,
includes straps, closures, may include padding, shoulder straps, pendulous abdomen design,

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
95
prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized
to fit a specific patient by an individual with expertise
L0638
F4
#Lumbar sacral orthosis, sagittal-coronal control, with rigid anterior and posterior frame/panels,
posterior extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by
rigid lateral frame/panels, produces intracavitary pressure to reduce load on intervertebral discs,
includes straps, closures, may include padding, shoulder straps, pendulous abdomen design,
custom fabricated
L0639
F4
#Lumbar sacral orthosis, sagittal-coronal control, rigid shell(s)/panel(s) posterior extends from
sacrococcygeal junction to T-9 vertebra, anterior extends from symphysis pubis to xyphoid,
produces intracavitary pressure to reduce load on the intervertebral discs, overall strength is
provided by overlapping rigid material and stabilizing closures, includes straps, closures, may
include soft interface, pendulous abdomen design, prefabricated item that has been trimmed,
bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with
expertise
L0640
F4
#Lumbar sacral orthosis, sagittal-coronal control, rigid shell(s)/panel(s), posterior extends from
sacrococcygeal junction to T-9 vertebra, anterior extends from symphysis pubis to xiphoid,
produces intracavitary pressure to reduce load on the intervertebral discs, overall strength is
provided by overlapping rigid material and stabilizing closures, includes straps, closures, may
include soft interface, pendulous abdomen design, custom fabricated
L0643
F4
#Lumbar-sacral orthosis, sagittal control, with rigid posterior panel(s), posterior extends from
sacrococcygeal junction to T-9 vertebra, produces intracavitary pressure to reduce load on the
intervertebral discs, includes straps, closures, may include padding, stays, shoulder straps,
pendulous abdomen design, prefabricated, off-the-shelf
L0648
F4
#Lumbar-sacral orthosis, sagittal control, with rigid anterior and posterior panels, posterior
extends from sacrococcygeal junction to T-9 vertebra, produces intracavitary pressure to reduce
load on the intervertebral discs, includes straps, closures, may include padding, shoulder straps,
pendulous abdomen design, prefabricated, off-the-shelf
L0649
F4
#Lumbar-sacral orthosis, sagittal-coronal control, with rigid posterior frame/panel(s), posterior
extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by rigid lateral
frame/panels, produces intracavitary pressure to reduce load on intervertebral discs, includes
straps, closures, may include padding, stays, shoulder straps, pendulous abdomen design,
prefabricated, off-the-shelf
L0650
F4
#Lumbar-sacral orthosis, sagittal-coronal control, with rigid anterior and posterior
frame/panel(s), posterior extends from sacrococcygeal junction to T-9vertebra, lateral strength
provided by rigid lateral frame/panel(s), produces intracavitary pressure to reduce load on
intervertebral discs, includes straps,closures, may include padding, shoulder straps, pendulous
abdomen design, prefabricated, off-the-shelf
L0651
F4
#Lumbar-sacral orthosis, sagittal-coronal control, rigid shell(s)/panel(s), posterior extends from
sacrococcygeal junction to T-9 vertebra, anterior extends from symphysis pubis to xyphoid,
produces intracavitary pressure to reduce load on the intervertebral discs, overall strength is
provided by overlapping rigid material and stabilizing closures, includes straps, closures, may
include soft interface, pendulous abdomen design, prefabricated, off-the-shelf
Anterior-Posterior-Lateral Control
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
96
L0700
F2
#Cervical-thoracic-lumbar-sacral orthosis (CTLSO), anterior-posterior-lateral control, molded to
patient model, (Minerva type)
L0710
F2
#Cervical-thoracic-lumbar-sacral orthosis (CTLSO), anterior-posterior-lateral-control, molded to
patient model, with interface material (Minerva type)
Halo Procedure
L0810
F2
#HALO procedure cervical halo incorporated into jacket vest
L0820
F2
#HALO procedure, cervical halo incorporated into plaster body jacket
L0830
F2
#HALO procedure, cervical halo incorporated into Milwaukee type orthosis
L0859
F14
#Addition to HALO procedure, magnetic resonance image compatible systems, rings and pins,
any material
L0861
F14
#Addition to halo procedure, replacement liner/interface material
Additions to Spinal Orthoses
L0970
F6
#TLSO, corset front
L0972
F6
#LSO, corset front
L0974
F6
#TLSO, full corset
L0976
F6
#LSO, full corset
L0978
F6
#Axillary crutch extension
L0980
F6
#Peritoneal straps, prefabricated, off-the-shelf, pair
L0982
F6
#Stocking supporter grips, prefabricated, off-the-shelf, set of four (4)
L0984
F16
#Protective body sock, prefabricated, off-the-shelf, each
L0999
F6
Addition to spinal orthosis, not otherwise specified
Orthotic Devices-Scoliosis Procedures
Note: The orthotic care of scoliosis differs from other orthotic care in that the treatment is more dynamic in nature and
utilizes ongoing, continual modification of the orthosis to the member’s changing condition. This coding structure uses
the proper names, or eponyms, of the procedures because they have historic and universal acceptance in the
profession. It should be recognized that variations to the basic procedures described by the founders/developers are
accepted in various medical and orthotic practices throughout the country.
Cervical-Thoracic-Lumbar-Sacral Orthosis (CTLSO)
L1000
F2
#Cervical-thoracic-lumbar-sacral orthosis (CTLSO) (Milwaukee), inclusive of furnishing initial
orthosis, including model
L1001
F2
Cervical-thoracic-lumbar-sacral orthosis (CTLSO), immobilizer, infant size, prefabricated,
includes fitting and adjustment
L1005
F3
Tension based scoliosis orthosis and accessory pads, includes fitting and adjustment
L1010
F6
#Addition to Cervical-thoracic-lumbar-sacral orthosis (CTLSO) or scoliosis orthosis, axilla sling
L1020
F6
#Addition to CTLSO or scoliosis orthosis, kyphosis pad, each
L1025
F6
#Addition to CTLSO or scoliosis orthosis, kyphosis pad, floating
L1030
F6
#Addition to CTLSO or scoliosis orthosis, lumbar bolster pad
L1040
F6
#Addition to CTLSO or scoliosis orthosis, lumbar or lumbar rib pad
L1050
F6
#Addition to CTLSO or scoliosis orthosis, sternal pad
L1060
F6
#Addition to CTLSO or scoliosis orthosis, thoracic pad
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
97
L1070
F6
#Addition to CTLSO or scoliosis orthosis, trapeze sling
L1080
F6
#Addition to CTLSO or scoliosis orthosis, outrigger
L1085
F6
#Addition to CTLSO or scoliosis orthosis, outrigger, bilateral with vertical extensions
L1090
F6
#Addition to CTLSO or scoliosis orthosis, lumbar sling
L1100
F6
#Addition to CTLSO or scoliosis orthosis, ring flange, plastic or leather
L1110
F6
#Addition to CTLSO or scoliosis orthosis, ring flange, plastic or leather, molded to patient
model
L1120
F6
#Addition to CTLSO, scoliosis orthosis, cover for upright, each
Thoracic-Lumbar-Sacral Orthosis (TLSO) (Low Profile)
L1200
F4
#Thoracic-lumbar-sacral orthosis (TLSO), inclusive of furnishing initial orthosis only
L1210
F4
#Addition to TLSO, (low profile), lateral thoracic extension
L1220
F4
#Addition to TLSO, (low profile), anterior thoracic extension
L1230
F4
#Addition to TLSO, (low profile), Milwaukee type superstructure
L1240
F16
#Addition to TLSO, (low profile), lumbar derotation pad
L1250
F16
#Addition to TLSO, (low profile), anterior ASIS pad
L1260
F16
#Addition to TLSO, (low profile), anterior thoracic derotation pad
L1270
F16
#Addition to TLSO, (low profile), abdominal pad
L1280
F16
#Addition to TLSO, (low profile), rib gusset (elastic), each
L1290
F16
#Addition to TLSO, (low profile), lateral trochanteric pad
Other Scoliosis Procedures
L1300
F4
#Other scoliosis procedure, body jacket molded to patient model
L1310
F2
#Other scoliosis procedure, postoperative body jacket
L1499
F10
Spinal orthosis, not otherwise specified
Orthotic Devices-Lower Limb
Note: Lower Limb: The procedures in L1600-L2999 are considered as “Base” or “Basic Procedures” and may be modified
by listing procedures from the “Additions” sections and adding them to the base procedure.
Hip Orthosis (HO)-Flexible
L1600
F2
#Hip Orthosis, abduction control of hip joints, flexible, Frejka type with cover, prefabricated
item that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific
patient by an individual with expertise
L1610
F2
#Hip Orthosis, abduction control of hip joints, flexible, (Frejka cover only), prefabricated item
that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific
patient by an individual with expertise
L1620
F2
#Hip Orthosis, abduction control of hip joints, flexible, (Pavlik harness), prefabricated item that
has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient
by an individual with expertise
L1630
F2
#Hip Orthosis, abduction control of hip joints, semi-flexible (Von Rosen type), custom
fabricated
L1640
F2
#Hip Orthosis, abduction control of hip joints, static, pelvic band or spreader bar, thigh cuffs
custom fabricated
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
98
L1650
F2
#Hip Orthosis, abduction control of hip joints, static, adjustable (Ilfled type), prefabricated,
includes fitting and adjustment
L1652
F2
#Hip orthosis, bilateral thigh cuffs with adjustable abductor spreader bar, adult size,
prefabricated, includes fitting and adjustment, any type
L1660
F2
#Hip Orthosis, abduction control of hip joints, static, plastic, prefabricated, includes fitting and
adjustment
L1680
F2
#HO, abduction control of hip joints, dynamic pelvic control, adjustable hip motion control,
thigh cuffs (Rancho hip action type) custom fabricated
L1685
F2
#Hip Orthosis, abduction control of hip joint, post-operative hip abduction type, custom
fabricated
L1686
F2
#Hip Orthosis, abduction control of hip joint, post-operative hip abduction type, prefabricated,
includes fitting and adjustments
L1690
F2
#Combination, bilateral, lumbo-sacral, hip, femur orthosis providing adduction and internal
rotation control, prefabricated, includes fitting and adjustment
Legg Perthes
L1700
F2
#Legg-Perthes orthosis, (Toronto type), custom fabricated
L1710
F2
#Legg-Perthes orthosis, (Newington type), custom fabricated
L1720
F2
#Legg-Perthes orthosis, trilateral, (Tachdijan type), custom fabricated
L1730
F2
#Legg-Perthes orthosis, (Scottish Rite type), custom fabricated
L1755
F2
#Legg-Perthes orthosis, (Patten Bottom type), custom fabricated
Knee Orthosis (KO)
A custom fabricated knee orthosis is covered when there is a documented physical characteristic which requires the
use of a custom fabricated orthosis instead of a prefabricated orthosis. Examples of situations which meet the
criterion for a custom fabricated orthosis include, but are not limited to:
1. Deformity of the leg or knee;
2. Size of thigh and calf;
3. Minimal muscle mass upon which to suspend an orthosis.
Although these are examples of potential situations where a custom fabricated orthosis may be appropriate,
suppliers must consider prefabricated alternatives such as pediatric knee orthoses in patients with small limbs,
straps with additional length for large limbs, etc.
Knee Orthosis (KO); L1810, L1820
Covered for:
1. Members who have weakness or deformity of the knee and require stabilization.
L1810
F16
#Knee orthosis, elastic with joints, prefabricated item that has been trimmed, bent, molded,
assembled, or otherwise customized to fit a specific patient by an individual with expertise
L1812
F16
#Knee orthosis, elastic with joints, prefabricated, off-the-shelf
L1820
F16
#Knee orthosis, elastic with condylar pads and joints, with or without patellar control,
prefabricated, includes fitting and adjustment
L1830
F2
#Knee orthosis, immobilizer, canvas longitudinal, prefabricated, off-the-shelf
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
99
L1831
F3
#Knee orthosis, locking knee joint(s), positional orthosis, prefabricated, includes fitting and
adjustment
Covered for members with flexion or extension contractures of the knee.
L1832
F3
#Knee orthosis, adjustable knee joints (unicentric or polycentric), positional orthosis, rigid
support, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise
customized to fit a specific patient by an individual with expertise
L1833
F3
#Knee orthosis, adjustable knee joints (unicentric or polycentric), positional orthosis, rigid
support, prefabricated, off-the shelf
L1834
F3
#Knee orthosis, without knee joint, rigid, custom fabricated
Covered when:
1. The coverage criteria for L1830 are met; and
2. The general criterion for a custom fabricated orthosis is met.
L1836
F3
#Knee orthosis, rigid, without joint(s), includes soft interface material, prefabricated, off-the-
shelf
L1840
F3
#Knee orthosis, derotation, medial-lateral, anterior cruciate ligament, custom fabricated
Covered for: Members with instability due to internal ligamentous disruption of the knee.
L1843
F3
#Knee orthosis, single upright, thigh and calf, with adjustable flexion and extension joint
(unicentric or polycentric), medial-lateral and rotation control, with or without varus/valgus
adjustment, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise
customized to fit a specific patient by an individual with expertise
L1844
F3
#Knee orthosis, single upright, thigh and calf, with adjustable flexion and extension joint
(unicentric or polycentric), medial-lateral and rotation control, with or without varus/valgus
adjustment, custom fabricated
Covered when:
1. The coverage criteria for L1843 is met; and
2. The general criterion for a custom fabricated orthosis is met.
L1845
F3
#Knee orthosis, double upright, thigh and calf, with adjustable flexion and extension joint
(unicentric or polycentric), medial-lateral and rotation control, with or without varus/valgus
adjustment, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise
customized to fit a specific patient by an individual with expertise
L1846
F3
#Knee orthosis, double upright, thigh and calf, with adjustable flexion and extension joint
(unicentric or polycentric), medial-lateral and rotation control, with or without varus/valgus
adjustment, custom fabricated
Covered when:
1. The coverage criteria for L1845 is met; and
2. The general criterion for a custom fabricated orthosis is met.
L1847
F3
#Knee orthosis, double upright with adjustable joint, with inflatable air support chamber(s),
prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized
to fit a specific patient by an individual with expertise
L1848
F3
#Knee orthosis, double upright with adjustable joint, with inflatable air support chamber(s),
prefabricated, off-the-shelf
L1850
F3
#Knee orthosis, Swedish type, prefabricated, off-the-shelf
Covered for:
Members with knee instability due to genu recurvatum.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
100
L1851
F3
#Knee Orthosis (KO), single upright, thigh and calf, with adjustable flexion and extension joint
(unicentric or polycentric), medial-lateral and rotation control, with or without varus/valgus
adjustment, prefabricated, off-the-shelf
L1852
F3
#Knee Orthosis (KO), double upright, thigh and calf, with adjustable flexion and extension joint
(unicentric or polycentric), medial-lateral and rotation control, with or without varus/valgus
adjustment, prefabricated, off-the-shelf
L1860
F3
#Knee orthosis, modification of supracondylar prosthetic socket, custom fabricated (SK)
Covered for:
Members with knee instability due to genu recurvatum.
Ankle-Foot Orthosis (AFO)
AFOs that are molded-to-patient-model, or custom-fabricated, are covered for members when the basic coverage
criteria listed above and one of the following criteria are met:
1. The patient could not be fit with a prefabricated AFO, or
2. The condition necessitating the orthosis is expected to be permanent or of longstanding duration (more
than 6 months), or
3. There is a need to control the knee, ankle, or foot in more than one plane, or
4. The patient has a documented neurological, circulatory, or orthopedic status that requires custom
fabricating over a model to prevent tissue injury, or
5. The patient has a healing fracture which lacks normal anatomical integrity or anthropometric proportions.
L4392
F16
#Replacement, soft interface material, static AFO
L4394
F16
#Replacement, soft interface material, foot drop splint
L4396
F6
#Static or dynamic ankle foot orthosis, including soft interface material, adjustable for fit, for
positioning, may be used for minimal ambulation, prefabricated item that has been trimmed,
bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with
expertise
L4397
F6
#Static or dynamic ankle foot orthosis, including soft interface material, adjustable for fit, for
positioning, may be used for minimal ambulation, prefabricated, off-the-shelf
L4398
F6
#Foot drop splint, recumbent positioning device, prefabricated, off-the-shelf
L4631
F6
#Ankle foot orthosis, walking boot type, varus/valgus correction, rocker bottom, anterior tibial
shell, soft interface, custom arch support, plastic or other material, includes straps and closures,
custom fabricated
(Charcot Restraint Orthotic Walker- CROW boot)
- No other codes may be billed for a CROW boot.
- There is no separate billing for any modifications, fitting, or adjustments.
- Ankle-foot orthoses (AFO) described by codes L1900-L1990 are covered for members with weakness or
deformity of the foot and ankle who have the potential to benefit functionally, and/or who require
stabilization for medical reasons. For non-ambulatory members requiring stabilization, the supporting
documentation from the prescriber or evaluating medical provider (e.g. Physical Therapist) must clearly
describe the location and degree of joint instability, in addition to medical necessity to utilize AFO’s.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
101
- The allowed frequency of “
F7
” for procedural codes L1907, L1960, and L1970 is intended for pediatric
members where growth and development may require more frequent replacement. The supporting
documentation on file must include evidence of growth or anatomical change warranting the replacement.
L1900
F6
#Ankle foot orthosis, spring wire, dorsiflexion assist calf band, custom fabricated
L1902
F2
#Ankle foot orthosis, ankle gauntlet, prefabricated, off-the-shelf
L1904
F2
#Ankle orthosis, ankle gauntlet, custom fabricated
L1906
F2
#Ankle foot orthosis, multiligamentous ankle support, prefabricated, off-the-shelf
L1907
F7
#Ankle orthosis, supramalleolar with straps, with or without interface/pads, custom fabricated
L1910
F6
#Ankle foot orthosis, posterior, single bar, clasp attachment to shoe counter, prefabricated,
includes fitting and adjustment
L1920
F6
#Ankle foot orthosis, single upright with static or adjustable stop (Phelps or Perlstein type),
custom fabricated
L1930
F6
#Ankle foot orthosis, plastic or other material, prefabricated, includes fitting and adjustment
L1932
F6
#Ankle foot orthosis, rigid anterior tibial section, total carbon fiber or equal material,
prefabricated, includes fitting and adjustment
L1940
F6
#Ankle foot orthosis, plastic or other material, custom fabricated
L1945
F6
#Ankle foot orthosis, molded to patient model, plastic, rigid anterior tibial section (floor
reaction), custom fabricated
L1950
F4
#Ankle foot orthosis, spiral (IRM type), plastic, custom fabricated
L1951
F4
#Ankle foot orthosis, spiral, (Institute of Rehabilitative Medicine type), plastic or other material,
prefabricated, includes fitting and adjustment
L1960
F7
#Ankle foot orthosis, posterior solid ankle, plastic, custom fabricated
L1970
F7
#Ankle foot orthosis, plastic, with ankle joint, custom fabricated
L1971
F6
#Ankle foot orthosis, plastic or other material with ankle joint, prefabricated, includes fitting
and adjustment
L1980
F6
#Ankle foot orthosis, single upright free plantar dorsiflexion, solid stirrup, calf band/cuff (single
bar “BK” orthosis), custom fabricated
L1990
F6
#Ankle foot orthosis, double upright free plantar dorsiflexion, solid stirrup, calf band/cuff
(double bar “BK” orthosis), custom fabricated
Knee-Ankle-Foot-Orthosis (KAFO) (or any combination)
KAFOs that are molded-to-patient-model, or custom-fabricated, are covered for members when the basic coverage
criteria listed above and one of the following criteria are met:
1. The patient could not be fit with a prefabricated KAFO, or
2. The condition necessitating the orthosis is expected to be permanent or of longstanding duration (more
than 6 months), or
3. There is a need to control the knee, ankle, or foot in more than one plane, or
4. The patient has a documented neurological, circulatory, or orthopedic status that requires custom
fabricating over a model to prevent tissue injury, or
5. The patient has a healing fracture which lacks normal anatomical integrity or anthropometric proportions.
Knee-ankle-foot orthoses (KAFO) described by codes L2000-L2038 are covered for members for whom an ankle-foot
orthosis is covered and for whom additional knee stability is required.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
102
L2000
F4
#Knee ankle foot orthosis, single upright, free knee, free ankle, solid stirrup, thigh and calf
bands/cuffs (single bar “AK” orthosis), custom fabricated
L2005
F4
#Knee ankle foot orthosis, any material, single or double upright, stance control, automatic
lock and swing phase release, mechanical activation, includes ankle joint, any type, custom
fabricated
L2010
F4
#Knee ankle foot orthosis, single upright, free ankle, solid stirrup, thigh and calf bands/cuffs
(single bar “AK” orthosis), without knee joint, custom fabricated
L2020
F4
#Knee ankle foot orthosis, double upright, free knee, free ankle, solid stirrup, thigh and calf
bands/cuffs (double bar “AK” orthosis), custom fabricated
L2030
F4
#Knee ankle foot orthosis, double upright, free ankle, solid stirrup, thigh and calf bands/cuffs,
(double bar “AK” orthosis), without knee joint, custom fabricated
L2034
F4
#Knee ankle foot orthosis, full plastic, single upright, with or without free motion knee, medial
lateral rotation control, with or without free motion ankle, custom fabricated
L2035
F4
#Knee ankle foot orthosis, full plastic, static (pediatric size), without free motion ankle,
prefabricated, includes fitting and adjustment
L2036
F4
#Knee ankle foot orthosis, full plastic, double upright, with or without free motion knee, with or
without free motion ankle, custom fabricated
L2037
F4
#Knee ankle foot orthosis, full plastic, single upright, with or without free motion knee, with or
without free motion ankle, custom fabricated
L2038
F4
#Knee ankle foot orthosis, full plastic, with or without free motion knee, multi-axis ankle,
custom fabricated
Torsion Control Hip-Knee-Ankle-Foot Orthosis (HKAFO)
L2040
F4
#Hip knee ankle foot orthosis, torsion control, bilateral rotation straps, pelvic
band/belt, custom fabricated
L2050
F4
#Hip knee ankle foot orthosis, torsion control, bilateral torsion cables, hip joint, pelvic
band/belt, custom fabricated
L2060
F4
#Hip knee ankle foot orthosis, torsion control, bilateral torsion cables, ball bearing hip
joint, pelvic band/belt, custom fabricated
L2070
F4
#Hip knee ankle foot orthosis, torsion control, unilateral rotation straps, pelvic
band/belt, custom fabricated
L2080
F4
#Hip knee ankle foot orthosis, torsion control, unilateral torsion cable, hip joint, pelvic
band/belt, custom fabricated
L2090
F4
#Hip knee ankle foot orthosis, torsion control, unilateral torsion cable, ball bearing hip
joint, pelvic band/belt, custom fabricated
Fracture Orthoses
- Ankle-foot orthoses (AFO) described by codes L2106 –L2116 are covered for ambulatory patients with
weakness or deformity of the foot and ankle, who require stabilization for medical reasons, and have the
potential to benefit functionally.
- Knee-ankle-foot orthoses (KAFO) described by codes L2126-L2136 are covered for ambulatory patients for
whom an ankle-foot orthosis is covered and for whom additional knee stability is required.
L2106
F2
#Ankle foot orthosis, fracture orthosis, tibial fracture cast orthosis, thermoplastic type casting
material, custom fabricated
L2108
F2
#Ankle foot orthosis, fracture orthosis, tibial fracture cast orthosis, custom fabricated
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
103
L2112
F2
#Ankle foot orthosis, fracture orthosis, tibial fracture orthosis, soft, prefabricated, includes
fitting and adjustment
L2114
F2
#Ankle foot orthosis, fracture orthosis, tibial fracture orthosis, semi-rigid, prefabricated,
includes fitting and adjustment
L2116
F2
#Ankle foot orthosis, fracture orthosis, tibial fracture orthosis, rigid, prefabricated, includes
fitting and adjustment
L2126
F2
#Knee ankle foot orthosis, fracture orthosis, femoral fracture cast orthosis, thermoplastic type
casting material, custom fabricated
L2128
F2
#Knee ankle foot orthosis, fracture orthosis, femoral fracture cast orthosis, custom fabricated
L2132
F2
#KAFO, fracture orthosis, femoral fracture cast orthosis, soft, prefabricated, includes fitting
and adjustment
L2134
F2
#KAFO, fracture orthosis, femoral fracture cast orthosis, semi-rigid, prefabricated, includes
fitting and adjustment
L2136
F2
#KAFO, fracture orthosis, femoral fracture cast orthosis, rigid, prefabricated, includes fitting
and adjustment
Additions to Fracture Orthosis
L2180
F2
#Addition to lower extremity fracture orthosis, plastic shoe insert with ankle joints
L2182
F2
#Addition to lower extremity fracture orthosis, drop lock knee joint
L2184
F2
#Addition to lower extremity fracture orthosis, limited motion knee joint
L2186
F2
#Addition to lower extremity fracture orthosis, adjustable motion knee joint, Lerman type
L2188
F2
#Addition to lower extremity fracture orthosis, quadrilateral brim
L2190
F2
#Addition to lower extremity fracture orthosis, waist belt
L2192
F2
#Addition to lower extremity fracture orthosis, hip joint, pelvic band, thigh flange, and pelvic
belt
Additions to Lower Extremity Orthoses: Shoe-Ankle-Shin-Knee
The allowed frequency of “
F7
” for procedural codes L2210, L2220, L2270, L2275, and L2280 is intended for pediatric
members where growth and development may require more frequent replacement. The supporting documentation on
file must include evidence of growth or anatomical change warranting the replacement.
L2200
F7
#Addition to lower extremity, limited ankle motion, each joint
L2210
F7
#Addition to lower extremity, dorsiflexion assist (plantar flexion
resist), each joint
L2220
F7
#Addition to lower extremity, dorsiflexion and plantar flexion assist/resist, each joint
L2230
F6
#Addition to lower extremity, split flat caliper stirrups and plate attachment
L2232
F6
#Addition to lower extremity orthosis, rocker bottom for total contact ankle foot orthosis, for
custom fabricated orthosis only
L2240
F6
#Addition to lower extremity, round caliper and plate attachment
L2250
F6
#Addition to lower extremity, foot plate, molded to patient model, stirrup attachment
L2260
F6
#Addition to lower extremity, reinforced solid stirrup (Scott-Craig type)
L2265
F6
#Addition to lower extremity, long tongue stirrup
L2270
F7
#Addition to lower extremity, varus/valgus correction (“T”) strap, padded/lined or malleolus
pad
L2275
F7
#Addition to lower extremity, varus/valgus correction, plastic modification, padded/lined
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
104
L2280
F7
#Addition to lower extremity, molded inner boot
L2300
F2
#Addition to lower extremity, abduction bar (bilateral hip involvement), jointed, adjustable
L2310
F2
#Addition to lower extremity, abduction bar-straight
L2320
F6
#Addition to lower extremity, non-molded lacer, for custom fabricated orthosis only
L2330
F6
#Addition to lower extremity, lacer molded to patient model, for custom fabricated orthosis
only
L2335
F4
#Addition to lower extremity, anterior swing band
L2340
F4
#Addition to lower extremity, pre-tibial shell, molded to patient model
L2350
F6
#Addition to lower extremity, prosthetic type, (BK) socket, molded to patient model, (used for
‘PTB’ ‘AFO’ orthosis)
L2360
F5
#Addition to lower extremity, extended steel shank
L2370
F3
#Addition to lower extremity, Patten bottom
L2375
F6
#Addition to lower extremity, torsion control ankle joint and half solid stirrup
L2380
F6
#Addition to lower extremity, torsion control straight knee joint, each joint
L2385
F6
#Addition to lower extremity, straight knee joint, heavy duty, each joint
Covered for members with documented weight of more than 300 pounds.
L2387
F4
#Addition to lower extremity, polycentric knee joint, for custom fabricated knee ankle foot
orthosis, each joint
L2390
F6
#Addition to lower extremity, offset knee joint, each joint
L2395
F6
#Addition to lower extremity, offset knee joint, heavy duty, each joint
Covered for members with documented weight of more than 300 pounds.
L2397
F7
#Addition to lower extremity orthosis, suspension sleeve
L2861
F3
Addition to lower extremity joint, knee or ankle, concentric adjustable torsion
Additions to Straight Knee or Offset Knee Joints
L2405
F4
#Addition to knee joint, drop lock, each
L2415
F4
#Addition to knee lock with integrated release mechanism (bail, cable, or equal), any material,
each joint
L2425
F4
#Addition to knee joint, disc or dial lock for adjustable knee flexion, each joint
L2430
F4
#Addition to knee joint, ratchet lock for active and progressive knee extension, each joint
L2492
F4
#Addition to knee joint, lift loop for drop lock ring
Additions: Thigh/Weightbearing- Gluteal/Ischial Weightbearing
L2500
F4
#Addition to lower extremity, thigh/weight bearing, gluteal/ischial weight bearing, ring
L2510
F4
#Addition to lower extremity, thigh/weight bearing, quadrilateral brim, molded to patient
model
L2520
F4
#Addition to lower extremity, thigh/weight bearing, quadrilateral brim, custom fitted
L2525
F4
#Addition to lower extremity, thigh/weight bearing, ischial containment/narrow M-L brim
molded to patient model
L2526
F4
#Addition to lower extremity, thigh/weight bearing, ischial containment/narrow M-L brim,
custom fitted
L2530
F4
#Addition to lower extremity, thigh/weight bearing, lacer, non-molded
L2540
F4
#Addition to lower extremity, thigh/weight bearing, lacer, molded to patient model
L2550
F4
#Addition to lower extremity, thigh/weight bearing, high roll cuff
Additions: Pelvic and Thoracic Control
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
105
L2570
F4
#Addition to lower extremity, pelvic control, hip joint, clevis type two position hip joint, each
L2580
F4
#Addition to lower extremity, pelvic control, pelvic sling
L2600
F4
#Addition to lower extremity, pelvic control, hip joint, Clevis type, or thrust bearing, free, each
L2610
F4
#Addition to lower extremity, pelvic control, hip joint, clevis or thrust bearing, lock, each
L2620
F4
#Addition to lower extremity, pelvic control, hip joint, heavy duty, each
Covered for members with documented weight of more than 300 pounds.
L2622
F4
#Addition to lower extremity, pelvic control, hip joint, adjustable flexion, each
L2624
F4
#Addition to lower extremity, pelvic control, hip joint, adjustable flexion, extension, abduction
control, each
L2627
F4
#Addition to lower extremity, pelvic control, plastic, molded to patient model, reciprocating
hip joint and cables
L2628
F4
#Addition to lower extremity, pelvic control, metal frame, reciprocating hip joint and cables
L2630
F4
#Addition to lower extremity, pelvic control, band and belt, unilateral
L2640
F4
#Addition to lower extremity, pelvic control, band and belt, bilateral
L2650
F4
#Addition to lower extremity, pelvic and thoracic control, gluteal pad, each
L2660
F4
#Addition to lower extremity, thoracic control, thoracic band
L2670
F4
#Addition to lower extremity, thoracic control, paraspinal uprights
L2680
F4
#Addition to lower extremity, thoracic control, lateral support uprights
Additions: General
L2750
F4
#Addition to lower extremity orthosis, plating chrome or nickel, per bar
L2755
F4
#Addition to lower extremity orthosis, high strength, lightweight material, all hybrid
lamination/prepreg composite, per segment, for custom fabricated orthosis only
L2760
F20
#Addition to lower extremity orthosis, extension, per extension, per bar (for lineal adjustment
for growth)
L2768
F4
#Orthotic side bar disconnect device, per bar
L2780
F4
#Addition to lower extremity orthosis, non-corrosive finish, per bar
L2785
F4
#Addition to lower extremity orthosis, drop lock retainer, each
L2795
F6
#Addition to lower extremity orthosis, knee control, full kneecap
L2800
F6
#Addition to lower extremity orthosis, knee control, knee cap, medial or lateral pull, for use
with custom fabricated orthosis only
L2810
F6
#Addition to lower extremity orthosis, knee control, condylar pad
L2820
F6
#Addition to lower extremity orthosis, soft interface for molded plastic, below knee section
Covered for a documented history of skin breakdown.
L2830
F6
#Addition to lower extremity orthosis, soft interface for molded plastic, above knee section
Covered for a documented history of skin breakdown.
L2840
F7
#Addition to lower extremity orthosis, tibial length sock, fracture or equal, each
L2850
F7
#Addition to lower extremity orthosis, femoral length sock, fracture or equal, each
L2999
F10
Lower extremity orthoses, not otherwise specified
Refer to “2010 Orthotics and Prosthetics Procedure Code Changes” update dated December
28, 2009 for specific items that are billable using L2999. Billing code L2999 is not limited to
only those items.
Orthotic Devices: Upper Limb
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
106
Note: Upper Limb: the procedures in this section are considered as “Base” or “Basic Procedures” and may be modified
by listing procedures from the “Additions” section and adding them to the base procedure.
Shoulder Orthosis (SO)
L3650
F2
#Shoulder orthosis, figure of “8” design abduction restrainer, prefabricated, off-the-shelf
L3660
F2
#Shoulder orthosis, figure of “8” design abduction restrainer, canvas and webbing,
prefabricated, off-the-shelf
L3670
F2
#Shoulder orthosis, acromio/clavicular (canvas and webbing type), prefabricated, off-the-shelf
L3671
F2
Shoulder orthosis, shoulder cap design, without joints, may include soft interface, straps,
custom fabricated, includes fitting and adjustment
L3674
F2
Shoulder orthosis, abduction positioning (airplane design), thoracic component and support
bar, with or without non torsion joint/turnbuckle, may include soft interface, straps, custom
fabricated, includes fitting and adjustment
L3675
F2
#Shoulder orthosis, vest type abduction restrainer, canvas webbing type, or equal,
prefabricated, off-the-shelf
L3677
F2
Shoulder orthosis, shoulder joint design, without joints, may include soft interface, straps,
prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized
to fit a specific patient by an individual with expertise
Elbow Orthosis (EO)
L3702
F4
#Elbow orthosis, without joints, may include soft interface, straps, custom fabricated, includes
fitting and adjustment
L3710
F4
#Elbow orthosis, elastic with metal joints, prefabricated, off-the-shelf
L3720
F4
#Elbow orthosis, double upright with forearm/arm cuffs, free motion, custom fabricated
L3730
F4
#Elbow orthosis, double upright with forearm/arm cuffs, extension/flexion assist, custom
fabricated
L3740
F4
#Elbow orthosis, double upright with forearm/arm cuffs, adjustable position lock with active
control, custom fabricated
L3760
F4
#Elbow orthosis (EO), with adjustable position locking joint(s), prefabricated, item that has
been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by
an individual with expertise
L3761
F4
#Elbow orthosis (EO), with adjustable position locking joint(s), prefabricated, off-the-shelf
L3762
F4
#Elbow orthosis, rigid, without joints, includes soft interface material, prefabricated, off-the-
shelf
L3763
F4
#EWHO, rigid, without joints, may include soft interface, straps, custom fabricated, includes
fitting and adjustment
L3764
F4
#EWHO, includes one or more nontorsion joints, elastic bands, turnbuckles, may include soft
interface, straps, custom fabricated, includes fitting and adjustment
L3765
F4
#EWHFO, rigid, without joints, may include soft interface, straps, custom fabricated, includes
fitting and adjustment
L3766
F4
#EWHFO, includes one or more nontorsion joints, elastic bands, turnbuckles, may include soft
interface, straps, custom fabricated, includes fitting and adjustment
Wrist-Hand-Finger Orthosis (WHFO)
L3806
F4
#Wrist hand finger orthosis, includes one or more nontorsion joint(s),
turnbuckles, elastic bands/springs, may include soft interface material, straps, custom
fabricated, includes fitting and adjustment

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
107
L3807
F16
#Wrist hand finger orthosis, without joint(s), prefabricated item that has been trimmed, bent,
molded, assembled, or otherwise customized to fit a specific patient by an individual with
expertise
L3808
F4
#Wrist hand finger orthosis, rigid without joints, may include soft interface material; straps,
custom fabricated, includes fitting and adjustment
L3809
F16
#Wrist hand finger orthosis, without joint(s), prefabricated, off-the-shelf, any type
Additions to Upper Extremity Orthosis
L3891
F4
Addition to upper extremity joint, wrist or elbow, concentric adjustable torsion
Dynamic Flexor Hinge, Reciprocal Wrist Extension/Flexion, Finger Flexion/Extension
L3900
F4
#Wrist hand finger orthosis, dynamic flexor hinge, reciprocal wrist extension/flexion, finger
flexion/extension, wrist or finger driven, custom fabricated
L3901
F4
#Wrist hand finger orthosis, dynamic flexor hinge, reciprocal wrist extension/flexion, finger
flexion/extension, cable driven, custom fabricated
External Power
L3904
F3
Wrist hand finger orthosis, external powered, electric, custom fabricated
Other WHFO’s: Custom-Fitted
L3905
F4
#Wrist hand orthosis, includes one or more nontorsion joints, elastic bands, turnbuckles, may
include soft interface, straps, custom fabricated, includes fitting and adjustment
L3906
F6
#Wrist hand orthosis, wrist hand orthosis, without joints, may include soft interface, straps,
custom fabricated, includes fitting and adjustment
L3908
F6
#Wrist hand orthosis, wrist extension control cock-up, non-molded, prefabricated, off-the-
shelf
L3912
F2
#Hand finger orthosis, flexion glove with elastic finger control, prefabricated, off-the-shelf
L3913
F4
#Hand finger orthosis, without joints, may include soft interface, straps, custom fabricated,
includes fitting and adjustment
L3915
F4
#Wrist hand orthosis, includes one or more nontorsion joint(s), elastic bands, turnbuckles,
may include soft interface, straps, prefabricated item that has been trimmed, bent, molded,
assembled, or otherwise customized to fit a specific patient by an individual with expertise
L3916
F4
#Wrist hand orthosis, includes one or more nontorsion joint(s), elastic bands, turnbuckles,
may include soft interface, straps, prefabricated, off-the-shelf
L3917
F2
#Hand orthosis, metacarpal fracture orthosis, prefabricated item that has been trimmed, bent,
molded, assembled, or otherwise customized to fit a specific patient by an individual with
expertise
L3918
F2
#Hand orthosis, metacarpal fracture orthosis, prefabricated, off-the-shelf
L3919
F4
#Hand orthosis, without joints, may include soft interface, straps, custom fabricated, includes
fitting and adjustment
L3921
F4
#Hand finger orthosis, includes one or more nontorsion joints, elastic bands, turnbuckles, may
include soft interface, straps, custom fabricated, includes fitting and adjustment
L3923
F16
#Hand finger orthosis, without joints, may include soft interface, straps, prefabricated item
that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific
patient by an individual with expertise

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
108
L3924
F16
#Hand finger orthosis, without joints, may include soft interface, straps, prefabricated, off-the-
shelf
L3925
F6
#Finger orthosis, proximal interphalangeal (pip)/distal interphalangeal (dip), nontorsion
joint/spring, extension/flexion, may include soft interface material, prefabricated, off-the-shelf
L3927
F6
#Finger orthosis, proximal interphalangeal (pip)/distal interphalangeal (dip), without
joint/spring, extension/flexion (e.g., static or ring type), may include soft interface material,
prefabricated, off-the-shelf
L3929
F6
#Hand finger orthosis, includes one or more nontorsion joint(s), turnbuckles, elastic
bands/springs, may include soft interface material, straps, prefabricated item that has been
trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an
individual with expertise
L3930
F6
#Hand finger orthosis, includes one or more nontorsion joint(s), turnbuckles, elastic
bands/springs, may include soft interface material, straps, prefabricated, off-the-shelf
L3931
F6
#Wrist hand finger orthosis, includes one or more nontorsion joint(s), turnbuckles, elastic
bands/springs, may include soft interface material, straps, prefabricated, includes fitting and
adjustment
L3933
F4
#FO, without joints, may include soft interface, custom fabricated, includes fitting and
adjustment
L3935
F4
#FO, nontorsion joint, may include soft interface, custom fabricated, includes fitting and
adjustment
Shoulder-Elbow–Wrist–Hand Orthosis (SEWHO) Abduction Position: Custom Fitted
Abduction Position: Custom Fitted
L3960
F2
#Shoulder elbow wrist hand finger orthosis, abduction positioning, airplane design,
prefabricated, includes fitting and adjustment
L3961
F2
Shoulder elbow wrist hand finger orthosis, shoulder cap design, without joints, may include
soft interface, straps, custom fabricated, includes fitting and adjustment
L3962
F2
#Shoulder elbow wrist hand finger orthosis, abduction positioning, Erbs Palsy design,
prefabricated, includes fitting and adjustment
L3967
F3
Shoulder elbow wrist hand finger orthosis, abduction positioning (airplane design), thoracic
component and support bar, without joints, may include soft interface, straps, custom
fabricated, includes fitting and adjustment
L3971
F3
Shoulder elbow wrist hand finger orthosis, shoulder cap design, includes one or more
nontorsion joints, elastic bands, turnbuckles, may include soft interface, straps, custom
fabricated, includes fitting and adjustment
L3973
F3
Shoulder elbow wrist hand finger orthosis, abduction positioning (airplane design), thoracic
component and support bar, includes one or more nontorsion joints, elastic bands,
turnbuckles, may include soft interface, straps, custom fabricated, includes fitting and
adjustment
L3975
F3
Shoulder elbow wrist hand finger orthosis, shoulder cap design, without joints, may include
soft interface, straps, custom fabricated, includes fitting and adjustment
L3976
F3
Shoulder elbow wrist hand finger orthosis, abduction positioning (airplane design), thoracic
component and support bar, without joints, may include soft interface, straps, custom
fabricated, includes fitting and adjustment
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
109
L3977
F3
Shoulder elbow wrist hand finger orthosis, shoulder cap design, includes one or more
nontorsion joints, elastic bands, turnbuckles, may include soft interface, straps, custom
fabricated, includes fitting and adjustment
L3978
F3
Shoulder elbow wrist hand finger orthosis, abduction positioning (airplane design), thoracic
component and support bar, includes one or more nontorsion joints, elastic bands,
turnbuckles, may include soft interface, straps, custom fabricated, includes fitting and
adjustment
Fracture Orthoses
L3980
F2
#Upper extremity fracture orthosis, humeral, prefabricated, includes fitting and adjustment
L3982
F2
#Upper extremity fracture orthosis, radius/ulnar, prefabricated, includes fitting and
adjustment
L3984
F2
#Upper extremity fracture orthosis, wrist, prefabricated, includes fitting and adjustment
L3995
F7
#Addition to upper extremity orthosis, sock, fracture or equal, each
L3999
F10
Upper limb orthosis, not otherwise specified
Refer to “2010 Orthotics and Prosthetics Procedure Code Changes” update dated December
28, 2009 for specific items that are billable using L3999. Billing code L3999 is not limited to
only those items.
Repairs, Replacements and Maintenance to Existing Orthoses
Note: The following codes are to be used only in billing for repair, maintenance and/or replacements to existing
orthoses. These codes are not to be billed in conjunction with codes for newly fitted orthoses.
Specific Repair
L4000
F6
#Replace girdle for spinal orthosis (CTLSO or SO) (e.g., Milwaukee)
L4002
F22
#Replacement strap, any orthosis, includes all components, any length, any type
L4010
F6
#Replace trilateral socket brim
L4020
F6
#Replace quadrilateral socket brim, molded to patient model
L4030
F6
#Replace quadrilateral socket brim, custom fitted
L4040
F6
#Replace molded thigh lacer, for custom fabricated orthosis only
L4045
F6
#Replace non-molded thigh lacer, for custom fabricated orthosis only
L4050
F6
#Replace molded calf lacer, for custom fabricated orthosis only
L4055
F6
#Replace non-molded calf lacer, for custom fabricated orthosis only
L4060
F6
#Replace high roll cuff
L4070
F6
#Replace proximal and distal upright for KAFO
L4080
F6
#Replace metal bands KAFO, proximal thigh
L4090
F6
#Replace metal bands KAFO-AFO, calf or distal thigh
L4100
F6
#Replace leather cuff KAFO, proximal thigh
L4110
F6
#Replace leather cuff KAFO-AFO, calf or distal thigh
L4130
F6
#Replace pretibial shell
Repairs
L4205
F9
#Repair of orthotic device, labor component, per 15 minutes
More than 2 hours requires prior approval
L4210
F7
#Repair of orthotic device, repair or replace minor parts
Not to be billed in conjunction with L4205
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
110
4.6 Prescription Footwear
Orthopedic Footwear
- Orthopedic footwear are shoes, shoe modifications or shoe additions that are covered when used to
correct, accommodate, or prevent a physical deformity or range of motion malfunction in a diseased or
injured part of the ankle or foot; to support a weak or deformed structure of the ankle or foot or to form an
integral part of a brace.
- Minimum orthopedic shoe specifications consist of Blucher or Bal construction, leather construction or
synthetic material of equal quality, welt construction with a cement-attached outsole or sewn on outsole,
upper portion properly fitted as to length and width, no unit sole, bottom sized to the last, closure
appropriate to foot condition (Velcro strap or lace closure preferred), full range of width; not just narrow,
medium, wide; extended medial counter and firm heel counter.
- The additional charge for split size (mis-mating) orthopedic footwear may be billed using code L3257
(MEVS dispensing validation required).
Non-Covered Indications:
Sneakers and athletic shoes are not considered orthopedic shoes by the Medicaid Program and therefore are not
Medicaid reimbursable.
Insert, Removable, Molded to Patient Model
L3000
F7
#Foot, insert, removable, molded to patient model, “UCB” type, Berkeley shell, each
L3001
F7
#Foot, insert, removable, molded to patient model, Spenco, each
L3002
F6
#Foot, insert, removable, molded to patient model, plastazote or equal, each
L3003
F7
#Foot, insert, removable, molded to patient model, silicone gel, each
L3010
F6
#Foot, insert, removable, molded to patient model, longitudinal arch support, each
L3020
F6
#Foot, insert, removable, molded to patient model, longitudinal/metatarsal support, each
L3030
F7
#Foot, insert, removable, formed to patient foot, each
L3031
F6
#Foot, insert/plate, removable, addition to lower extremity orthosis, high strength, lightweight
material, all hybrid lamination/prepreg composite, each
Arch Support, Removable, Pre-molded
L3040
F6
#Foot, arch support, removable, premolded, longitudinal, each
L3050
F7
#Foot, arch support, removable, premolded, metatarsal, each
L3060
F6
#Foot, arch support, removable, premolded, longitudinal/metatarsal, each
Arch Support, Non-Removable, Attached to Shoe
L3070
F7
#Foot, arch support, non-removable attached to shoe, longitudinal, each
L3080
F7
#Foot, arch support, non-removable attached to shoe, metatarsal, each
L3090
F7
#Foot, arch support, non-removable attached to shoe, longitudinal/metatarsal, each
L3100
F7
#Hallus-valgus night dynamic splint
Abduction And Rotation Bars
L3140
F7
#Foot, abduction rotation bars, including shoes (Dennis Browne type)
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
111
L3150
F7
Foot, abduction rotation bars, without shoe(s) (Dennis Browne type)
L3160
F7
Foot, adjustable shoe-styled positioning device
L3170
F7
#Foot, plastic, silicone or equal, heel stabilizer, each
Orthopedic Footwear
L3201
F7
#Orthopedic shoe, oxford with supinator or pronator, infant (each)
L3202
F7
#Orthopedic shoe, oxford with supinator or pronator, child (each)
L3203
F7
#Orthopedic shoe, oxford with supinator or pronator, junior (each)
L3204
F7
#Orthopedic shoe, hightop with supinator or pronator, infant (each)
L3206
F7
#Orthopedic shoe, hightop with supinator or pronator, child (each)
L3207
F7
#Orthopedic shoe, hightop with supinator or pronator, junior (each)
L3208
F7
#Surgical boot, each, infant
L3209
F7
#Surgical boot, each, child
L3211
F7
#Surgical boot, each, junior
L3212
F7
#Benesch boot, pair, infant
L3213
F7
#Benesch boot, pair, child
L3214
F7
#Benesch boot, pair, junior
L3215
F7
#Orthopedic footwear, ladies shoe, oxford, each
L3216
F7
#Orthopedic footwear, ladies shoe, depth inlay, each
L3217
F7
#Orthopedic footwear, ladies shoe, hightop, depth inlay, each
L3219
F7
#Orthopedic footwear, mens shoe, oxford, each
L3221
F7
#Orthopedic footwear, mens shoe, depth inlay, each
L3222
F7
#Orthopedic footwear, mens shoe, hightop, depth inlay, each
L3224
F7
#Orthopedic footwear, woman’s shoe, oxford, used as an integral part of a brace (orthosis)
(each)
L3225
F7
#Orthopedic footwear, man’s shoe, oxford, used as an integral part of a brace (orthosis)
(each)
L3230
F7
#Orthopedic footwear, custom (molded to patient) shoe, depth inlay, each
L3250
F7
#Orthopedic footwear, custom molded shoe, removable inner mold, prosthetic shoe, each
L3252
F7
#Foot, shoe molded to patient model, plastazote (or similar), custom fabricated, each
L3253
F7
#Foot, molded shoe, plastazote (or similar), custom fitted, each
L3254
F7
#Non-standard size or width
L3255
F7
#Non-standard size or length
L3257
F7
#Orthopedic footwear, additional charge for split size
L3260
F7
#Surgical boot/shoe, each
L3265
F7
#Plastazote sandal, each
Shoe Modification: Lifts
L3300
F7
#Lift, elevation, heel, tapered to metatarsals, per inch
L3310
F7
#Lift, elevation, heel and sole, neoprene, per inch
L3320
F7
#Lift, elevation, heel and sole, cork, per inch
L3330
F7
#Lift, elevation, metal extension (skate)
L3332
F7
#Lift, elevation, inside shoe, tapered, up to one-half inch
L3334
F7
#Lift, elevation, heel, per inch
Shoe Modification: Wedges
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
112
L3340
F7
#Heel wedge, SACH
L3350
F7
#Heel wedge
L3360
F7
#Sole wedge, outside sole
L3370
F7
#Sole wedge, between sole
L3380
F7
#Clubfoot wedge
L3390
F7
#Outflare wedge
L3400
F7
#Metatarsal bar wedge, rocker
L3410
F7
#Metatarsal bar wedge, between sole
L3420
F7
#Full sole and heel wedge, between sole
Shoe Modification: Heels
L3430
F7
#Heel, counter, plastic reinforced
L3440
F7
#Heel, counter, leather reinforced
L3450
F7
#Heel, SACH cushion type
L3455
F7
#Heel, new leather, standard
L3460
F7
#Heel, new rubber, standard
L3465
F7
#Heel, Thomas with wedge
L3470
F7
#Heel, Thomas extended to ball
L3480
F7
#Heel, pad and depression for spur
L3485
F7
#Heel, pad, removable for spur
Miscellaneous Shoe Additions
L3500
F7
#Orthopedic shoe addition, insole, leather
L3510
F7
#Orthopedic shoe addition, insole, rubber
L3520
F7
#Orthopedic shoe addition, insole, felt covered with leather
L3530
F7
#Orthopedic shoe addition, sole, half
L3540
F7
#Orthopedic shoe addition, sole, full (each)
L3550
F7
#Orthopedic shoe addition, toe tap standard
L3560
F7
#Orthopedic shoe addition, toe tap, horseshoe
L3570
F7
Orthopedic shoe addition, special extension to instep (leather with eyelets)
L3580
F7
Orthopedic shoe addition, convert instep to Velcro closure
L3590
F7
#Orthopedic shoe addition, convert firm shoe counter to soft counter
L3595
F7
#Orthopedic shoe addition, March bar
Transfers or Replacement
L3600
F7
Transfer of an orthosis from one shoe to another, caliper plate, existing
L3610
F7
Transfer of an orthosis from one shoe to another, caliper plate, new
Shoe Corrections and Modifications
L3620
F7
Transfer of an orthosis from one shoe to another, solid stirrup, existing
L3630
F7
Transfer of an orthosis from one shoe to another, solid stirrup, new
L3640
F7
Transfer of an orthosis from one shoe to another, Dennis Browne splint (Riveton), both shoes
L3649
F7
#Orthopedic shoe, modification, addition, or transfer, not otherwise specified (more than two
procedures require prior approval)
Diabetic Shoes, Fitting, and Modifications
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
113
Covered as a component of a comprehensive diabetic treatment plan to treat amputation, or pre-ulcerative calluses, or
peripheral neuropathy with evidence of callus formation of either foot,
or a foot deformity, or poor circulation. Limited
to shoe codes, inserts, and/or modifications designated
for diabetics only.
Billing in conjunction with other orthopedic footwear codes may be considered a duplication of service and result in a
claim denial.
A5500
F7
#For diabetics only, fitting (including follow-up), custom preparation and supply of off-the-
shelf depth-inlay shoe manufactured to accommodate multi-density insert(s), per shoe
A5501
F7
#For diabetics only, fitting (including follow-up), custom preparation and supply of shoe
molded from cast(s) of patient’s foot (custom-molded shoe), per shoe
A5503
F7
#For diabetics only, modification (including fitting) of off-the-shelf depth-inlay shoe or
custom-molded shoe with roller or rigid rocker bottom, per shoe
A5504
F7
#For diabetics only, modification (including fitting) of off-the-shelf depth-inlay shoe or
custom-molded shoe with wedge(s), per shoe
A5505
F7
#For diabetics only, modification (including fitting) of off-the-shelf depth-inlay shoe or
custom-molded shoe with metatarsal bar, per shoe
A5506
F7
#For diabetics only, modification (including fitting) of off-the-shelf depth-inlay shoe or
custom-molded shoe with off-set heel(s), per shoe
A5507
F7
#For diabetics only, not otherwise specified modification (including fitting) of off-the-shelf
depth-inlay shoe or custom-molded shoe, per shoe
A5512
F7
#For diabetics only, multiple density insert, direct formed, molded to foot after external heat
source of 230 degrees Fahrenheit or higher, total contact with patient’s foot, including arch,
base layer minimum of ¼ inch material of shore a 35 durometer or 3/16 inch material of
shore a 40 durometer (or higher), prefabricated, each
A5513
F7
#For diabetics only, multiple density insert, custom molded from model of patient’s foot,
total contact with patient’s foot, including arch, base layer minimum of 1/4 inch material of
shore a 35 durometer or 3/16 inch material of shore a 40 durometer (or higher), includes
arch filler and other shaping material, custom fabricated, each
A5514
F7
#For diabetics only, multiple density insert, made by direct carving with CAM technology
from a rectified CAD model created from a digitized scan of the patient, total contact with
patient’s foot, including arch, base layer minimum of 3/16 inch material of shore a 35
durometer (or higher), includes arch filler and other shaping material, custom fabricated,
each
4.7 Prosthetics
1. This schedule is applicable to both children and adults.

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
114
2. Base codes are covered when the physician’s order and supporting documentation clearly establish the medical
and functional need being met by the prescribed device. Where applicable, code specific coverage criteria must
be met.
3. L Code “additions” are covered only when both the base codes coverage criteria have been met and specific
documentation exists establishing the medical necessity of the addition code.
4. The providers shall be responsible for any needed repairs or replacements due to defects in quality or
workmanship that appear within three months of delivery. This does not include adjustments or replacements
necessitated by anatomical changes.
5. Replacements and repairs: used to indicate replacement and repair of orthotic and prosthetic devices which
have been in use for some time. Prior approval is not required when the charge is over $35.00 and is less than
25% of the price listed on the code for the device. When specific replacement and repair codes are available,
they should be used instead of the code for the device with ‘-RB’. For charges $35.00 and under, use L7510.
6. The fees contained in this schedule will be paid under State-administered programs and are to be considered
full payment for the services rendered. The provider shall make no additional charge to the member.
7. Unless otherwise indicated all fees are for the unilateral, single unit or “each”.
8. All normal necessary pads and straps are included in the prices quoted.
9. Polypropylene (ultra-light) should be used only when judged a medical necessity because of bilateral or
multiple disabilities, frailty, cardiac disability, etc.
10. For home visit, see code L9900.
11. Only one prosthetic and its components can be obtained from the automated authorization system, the
dispensing validation system (DVS). If bilateral prosthetics are necessary, prior approval must be obtained.
Lower Limb
Note: The procedures in this section are considered as “Base” or “Basic Procedures” and may be modified by listing
items/procedures or special materials from the “Additions” section, adding them to the “Base” Procedure.
A lower limb prosthesis is covered when the member:
1. Will reach or maintain a defined functional state within a reasonable amount of time; and
2. Is motivated to ambulate.
FUNCTIONAL LEVELS:
- A determination of the medical necessity for certain components/additions to the prosthesis is based on the
patient's potential functional abilities. Potential functional ability is based on the reasonable expectations of the
prosthetist, and treating physician, considering factors including, but not limited to:
a) The patient's past history (including prior prosthetic use if applicable); and
b) The patient's current condition including the status of the residual limb and the nature of other medical
problems; and
c) The patient's desire to ambulate.
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
115
- Clinical assessments of patient rehabilitation potential must be based on the following classification levels:
Level 0: Does not have the ability or potential to ambulate or transfer safely with or without assistance and a
prosthesis does not enhance their quality of life or mobility.
Level 1: Has the ability or potential to use a prosthesis for transfers or ambulation on level surfaces at fixed
cadence. Typical of the limited and unlimited household ambulator.
Level 2: Has the ability or potential for ambulation with the ability to traverse low level environmental barriers
such as curbs, stairs, or uneven surfaces. Typical of the limited community ambulator.
Level 3: Has the ability or potential for ambulation with variable cadence. Typical of the community
ambulator who has the ability to traverse most environmental barriers and may have vocational,
therapeutic, or exercise activity that demands prosthetic utilization beyond simple locomotion.
Level 4: Has the ability or potential for prosthetic ambulation that exceeds basic ambulation skills, exhibiting
high impact, stress, or energy levels. Typical of the prosthetic demands of the child, active adult, or
athlete.
- The records must document the patient's current functional capabilities and his/her expected functional
potential, including an explanation for the difference, if that is the case. It is recognized, within the functional
classification hierarchy, that bilateral amputees often cannot be strictly bound by functional level classifications.
- The determination of coverage for selected prostheses and components with respect to potential functional
levels represents the usual case. Exceptions will be considered in an individual case if additional documentation
is included which justifies the medical necessity. Prostheses will be denied as not reasonable and necessary if
the patient's potential functional level is 0.
- A determination of the type of foot, or knee for the prosthesis will be made by the treating physician and the
prosthetist based upon the functional needs of the patient. Basic lower extremity prostheses include a SACH
foot. Basic lower extremity prostheses include a single axis, constant friction knee. Other prosthetic feet and/or
knees are considered for coverage based upon functional classification.
Partial Foot
L5000
F4
#Partial foot, shoe insert with longitudinal arch, toe filler
L5010
F4
#Partial foot, molded socket, ankle height, with toe filler
L5020
F4
#Partial foot, molded socket, tibial tubercle height, with toe filler
Ankle
L5050
F4
#Ankle, Symes, molded socket, SACH foot
Below Knee
L5100
F4
#Below knee, molded socket, shin, SACH foot
L5105
F4
#Below knee, plastic socket, joints and thigh lacer, SACH foot
Knee Disarticulation
L5150
F4
#Knee disarticulation (or through knee), molded socket, external knee joints, shin, SACH foot
L5160
F4
#Knee disarticulation (or through knee), molded socket, bent knee configuration, external
knee joints, shin, SACH foot
Above Knee
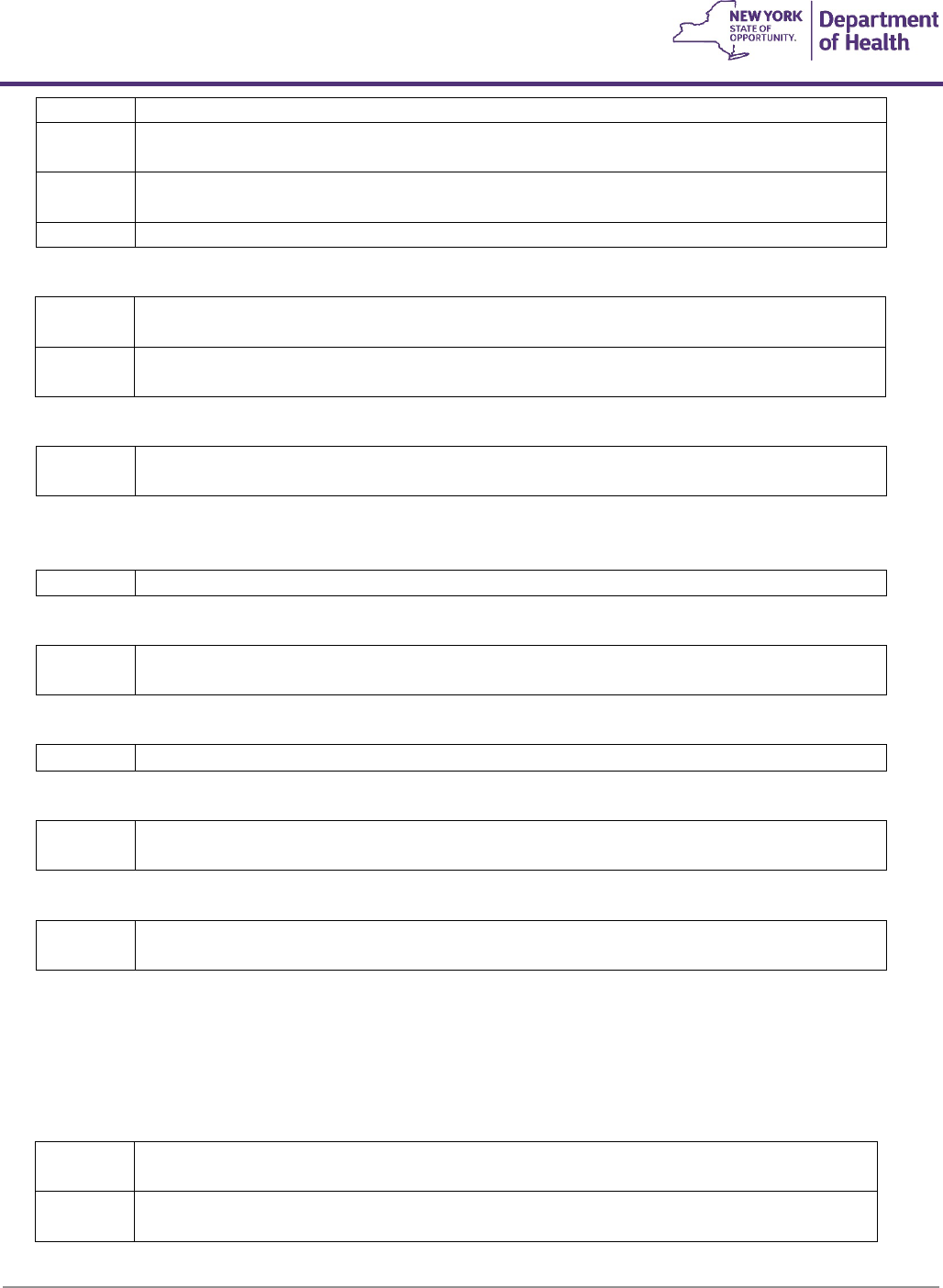
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
116
L5200
F4
#Above knee, molded socket, single axis constant friction knee, shin, SACH foot
L5210
F4
#Above knee, short prosthesis, no knee joint (“stubbies”), with foot blocks, no ankle joints,
each
L5220
F4
#Above knee, short prosthesis, no knee joint (“stubbies”), with articulated ankle/foot,
dynamically aligned, each
L5230
F4
#Above knee, for proximal femoral focal deficiency, constant friction knee, shin, SACH foot
Hip Disarticulation
L5250
F4
#Hip disarticulation, Canadian type; molded socket, hip joint, single axis constant friction
knee, shin, SACH foot
L5270
F4
#Hip disarticulation, tilt table type; molded socket, locking hip joint, single axis constant
friction knee, shin, SACH foot
Hemipelvectomy
L5280
F4
#Hemipelvectomy, Canadian type; molded socket, hip joint, single axis constant friction
knee, shin, SACH foot
Endoskeletal: Below Knee
For prosthetic covers, see codes L5704-L5707
L5301
F4
#Below knee, molded socket, shin, SACH foot, endoskeletal system
Endoskeletal: Knee Disarticulation
L5312
F4
#Knee disarticulation (or through knee), molded socket, single axis knee, pylon, SACH foot,
endoskeletal system
Endoskeletal: Above Knee
L5321
F4
#Above knee, molded socket, open end, SACH foot, endoskeletal system, single axis knee
Endoskeletal: Hip Disarticulation
L5331
F4
#Hip disarticulation, Canadian type, molded socket, endoskeletal system, hip joint, single axis
knee, SACH foot
Endoskeletal: Hemipelvectomy
L5341
F4
#Hemipelvectomy, Canadian type, molded socket, endoskeletal system, hip joint, single axis
knee, SACH foot
Immediate Post-Surgical or Early Fitting Procedures
Note: The immediate post-surgical procedure components will at all times remain the property of the prosthetic facility
and will be used only on a loan basis. It is estimated that the period of use by the amputee in each case will not exceed
one month.
L5400
F2
#Immediate post surgical or early fitting, application of initial rigid dressing, including
fitting, alignment, suspension, and one cast change, below knee
L5410
F2
#Immediate post surgical or early fitting, application of initial rigid dressing, including
fitting, alignment and suspension, below knee, each additional cast change and realignment
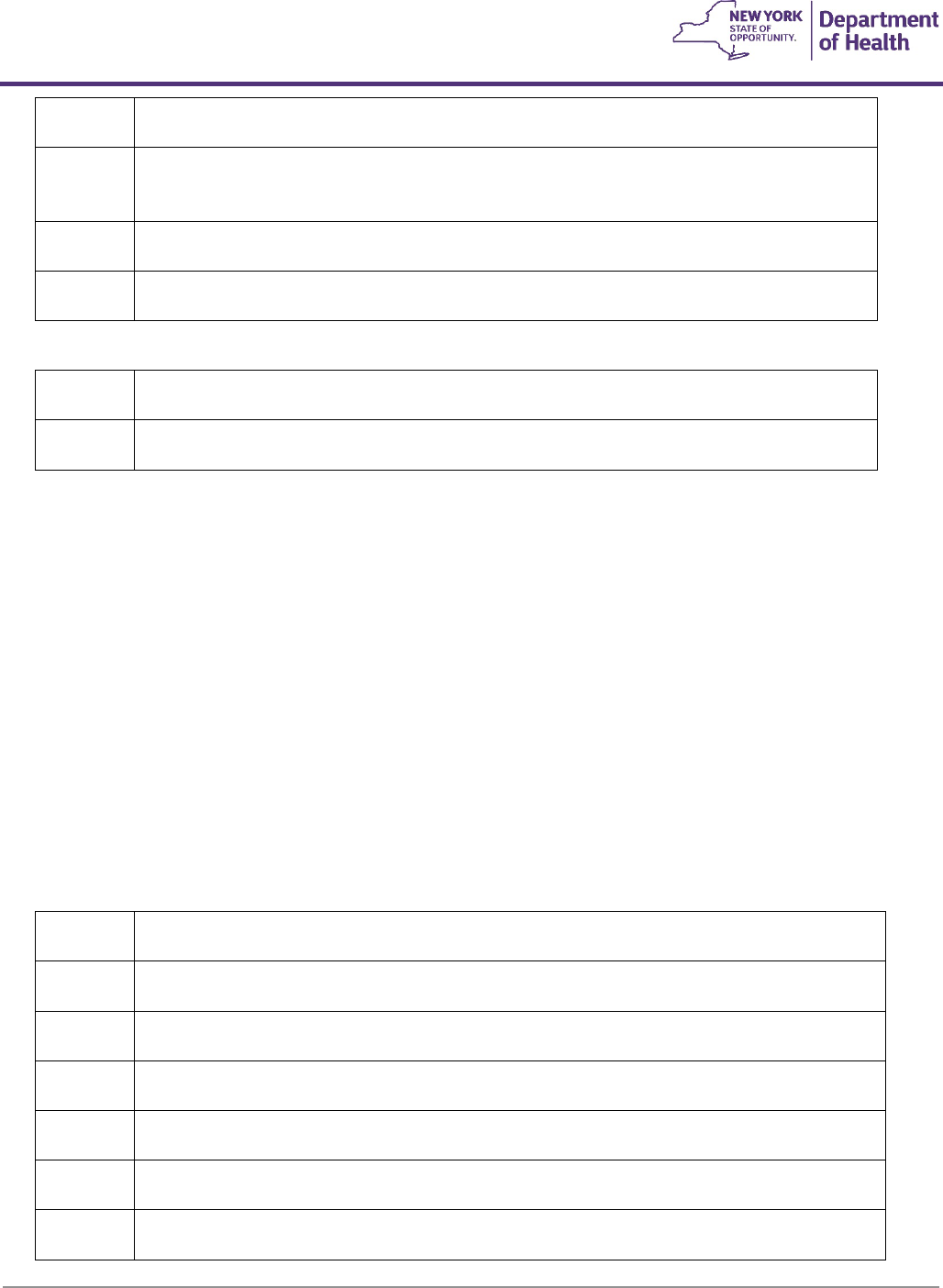
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
117
L5420
F2
#Immediate post surgical or early fitting, application of initial rigid dressing, including
fitting, alignment and suspension and one cast change “AK” or knee disarticulation
L5430
F2
#Immediate post surgical or early fitting, application of initial rigid dressing, including
fitting, alignment and suspension, “AK” or knee disarticulation, each additional cast change
and realignment
L5450
F18
#Immediate post surgical or early fitting, application of non-weight bearing rigid dressing,
below knee
L5460
F18
#Immediate post surgical or early fitting, application of non-weight bearing rigid dressing,
above knee
Initial Prosthesis
L5500
F2
#Initial, below knee “PTB” type socket, non-alignable system, pylon, no cover, SACH foot,
plaster socket, direct formed
L5505
F2
#Initial, above knee – knee disarticulation, ischial level socket, non-alignable system, pylon,
no cover, SACH foot, plaster socket, direct formed
Preparatory Prosthesis
Lower limb prostheses, preparatory, may be considered medically necessary for a new or revised amputation when ALL
the following criteria are met:
- The individual has had an above or below knee amputation; and
- The preparatory prosthesis is provided to an individual starting a rehabilitation program; and
- The preparatory prosthesis is provided after the surgical incision has healed; and
- The individual is motivated to ambulate using the prosthesis; and
- The preparatory prosthesis is prescribed by an eligible professional provider (i.e., physician with training and
expertise in the functional evaluation of individuals with amputations) and fitted/made by an orthotist or
prosthetist.
Lower limb prostheses, preparatory, are complete and all-inclusive; therefore, additional components, add-ons,
upgrades, adjustments, modifications, or substitutions of components, etc., are not separately reimbursable.
L5510
F2
#Preparatory, below knee “PTB” type socket, non-alignable system, pylon, no cover, SACH
foot, plaster socket, molded to model
L5520
F2
#Preparatory, below knee “PTB” type socket, non-alignable system, pylon, no cover, SACH
foot, thermoplastic or equal, direct formed
L5530
F2
#Preparatory, below knee “PTB” type socket, non-alignable system, pylon, no cover, SACH
foot, thermoplastic or equal, molded to model
L5535
F2
#Preparatory, below knee “PTB” type socket, non-alignable system, pylon, no cover, SACH
foot, prefabricated, adjustable open end socket
L5540
F2
#Preparatory, below knee “PTB” type socket, non-alignable system, pylon, no cover, SACH
foot, laminated socket, molded to model
L5560
F2
#Preparatory, above knee – knee disarticulation, ischial level socket, non-alignable system,
pylon, no cover, SACH foot, plaster socket, molded to model
L5570
F2
#Preparatory, above knee – knee disarticulation, ischial level socket, non-alignable system,
pylon, no cover, SACH foot, thermoplastic or equal, direct formed
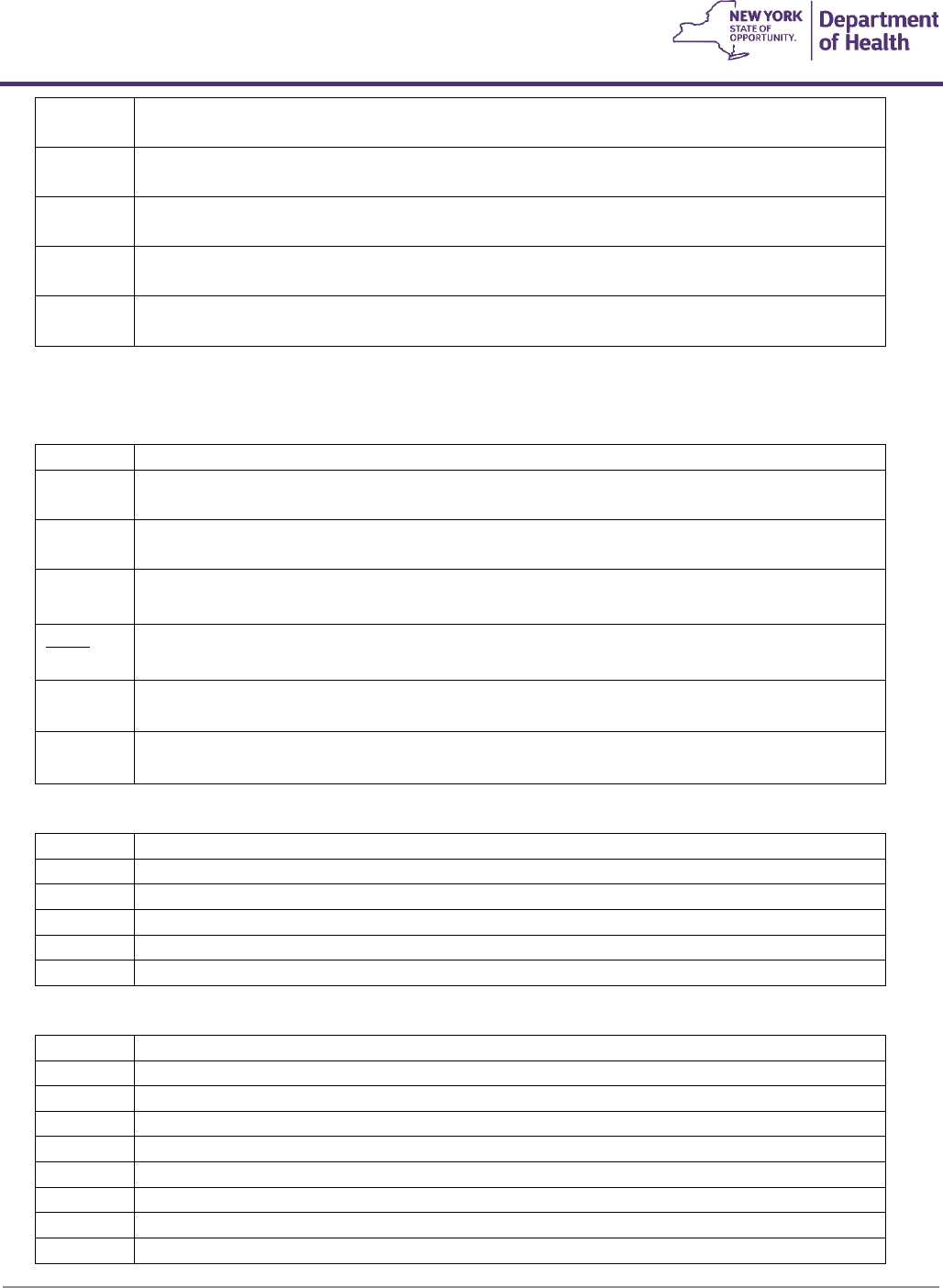
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
118
L5580
F2
#Preparatory, above knee – knee disarticulation, ischial level socket, non-alignable system,
pylon, no cover, SACH foot, thermoplastic or equal, molded to model
L5585
F2
#Preparatory, above knee – knee disarticulation, ischial level socket, non-alignable system,
pylon, no cover, SACH foot, prefabricated adjustable open end socket
L5590
F2
#Preparatory, above knee – knee disarticulation, ischial level socket, non-alignable system,
pylon, no cover, SACH foot, laminated socket, molded to model
L5595
F2
#Preparatory, hip disarticulation – hemipelvectomy, pylon, no cover, SACH foot,
thermoplastic or equal, molded to patient model
L5600
F2
#Preparatory, hip disarticulation-hemipelvectomy, pylon, no cover, SACH foot, laminated
socket, molded to patient model
Additions To Lower Extremity
A fluid or pneumatic knee (L5610, L5613, L5614) is covered for member’s whose functional level is 3 or above.
L5610
F4
#Addition to lower extremity, endoskeletal system, above knee, hydracadence system
L5611
F4
#Addition to lower extremity, endoskeletal system, above knee–knee disarticulation, 4-bar
linkage, with friction swing phase control
L5613
F4
#Addition to lower extremity, endoskeletal system, above knee–knee disarticulation, 4-bar
linkage, with hydraulic swing phase control
L5614
F4
#Addition to lower extremity, exoskeletal system, above knee–knee disarticulation, 4-bar
linkage, with pneumatic swing phase control
L5615
F4
Addition, endoskeletal knee-shin system, 4 bar linkage or multiaxial, fluid swing and stance
phase control
L5616
F4
#Addition to lower extremity, endoskeletal system, above knee, universal multiplex system,
friction swing phase control
L5617
F4
#Addition to lower extremity, quick change self-aligning unit, above knee or below knee,
each
Additions: Test Sockets
L5618
F4
#Addition to lower extremity, test socket, Symes
L5620
F4
#Addition to lower extremity, test socket, below knee
L5622
F4
#Addition to lower extremity, test socket, knee disarticulation
L5624
F4
#Addition to lower extremity, test socket, above knee
L5626
F4
#Addition to lower extremity, test socket, hip disarticulation
L5628
F4
#Addition to lower extremity, test socket, hemipelvectomy
Additions: Socket Variations
L5629
F4
#Addition to lower extremity, below knee, acrylic socket
L5630
F4
#Addition to lower extremity, Symes type, expandable wall socket
L5631
F4
#Addition to lower extremity, above knee or knee disarticulation, acrylic socket
L5632
F4
#Addition to lower extremity, Symes type, “PTB” Brim design socket
L5634
F4
#Addition to lower extremity, Symes type, posterior opening (Canadian) socket
L5636
F4
#Addition to lower extremity, Symes type, medial opening socket
L5637
F4
#Addition to lower extremity, below knee, total contact
L5638
F4
#Addition to lower extremity, below knee, leather socket
L5639
F4
#Addition to lower extremity, below knee, wood socket
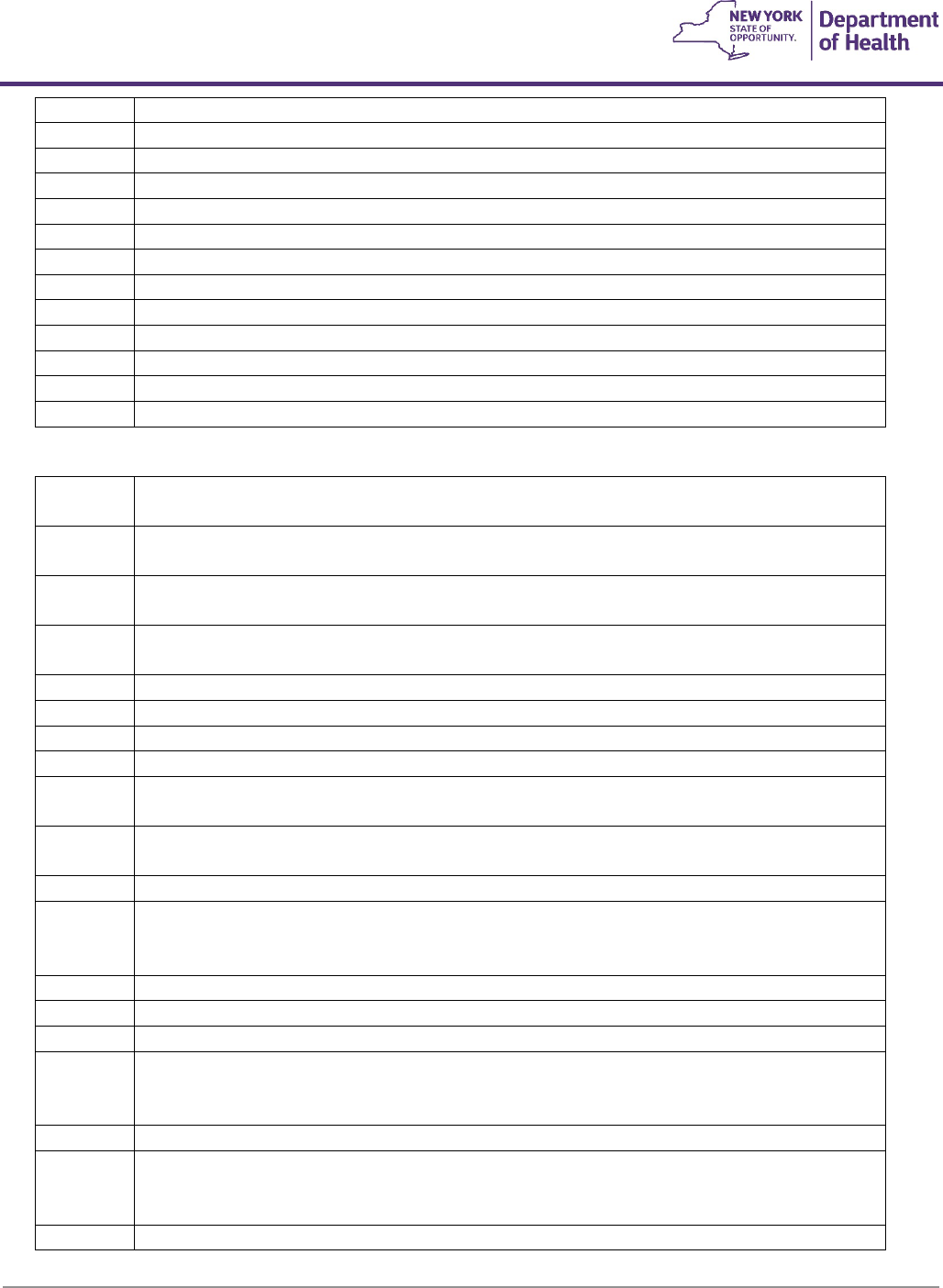
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
119
L5640
F4
#Addition to lower extremity, knee disarticulation, leather socket
L5642
F4
#Addition to lower extremity, above knee, leather socket
L5643
F4
#Addition to lower extremity, hip disarticulation, flexible inner socket, external frame
L5644
F4
#Addition to lower extremity, above knee, wood socket
L5645
F4
#Addition to lower extremity, below knee, flexible inner socket, external frame
L5646
F4
#Addition to lower extremity, below knee, air, fluid, gel, or equal, cushion socket
L5647
F4
#Addition to lower extremity, below knee, suction socket
L5648
F4
#Addition to lower extremity, above knee, air, fluid, gel or equal, cushion socket
L5649
F4
#Addition to lower extremity, ischial containment/narrow M-L socket
L5650
F4
#Addition to lower extremity, total contact, above knee or knee disarticulation socket
L5651
F4
#Addition to lower extremity, above knee, flexible inner socket, external frame
L5652
F4
#Addition to lower extremity, suction suspension, above knee or knee disarticulation socket
L5653
F4
#Addition to lower extremity, knee disarticulation, expandable wall socket
Additions: Socket Insert and Suspension
L5654
F6
#Addition to lower extremity, socket insert, Symes, (Kemblo, Pelite, Aliplast, Plastazote or
equal)
L5655
F6
#Addition to lower extremity, socket insert, below knee (Kemblo, Pelite, Aliplast, Plastazote
or equal)
L5656
F6
#Addition to lower extremity, socket insert, knee disarticulation (Kemblo, Pelite, Aliplast,
Plastazote or equal)
L5658
F6
#Addition to lower extremity, socket insert, above knee (Kemblo, Pelite, Aliplast, Plastazote
or equal)
L5661
F6
#Addition to lower extremity, socket insert, multi-durometer Symes
L5665
F6
#Addition to lower extremity, socket insert, multi-durometer, below knee
L5666
F6
#Addition to lower extremity, below knee, cuff suspension
L5668
F6
#Addition to lower extremity, below knee, molded distal cushion
L5670
F6
#Addition to lower extremity, below knee, molded supraconydlar suspension (“PTS” or
similar)
L5671
F6
#Addition to lower extremity, below knee/above knee suspension locking mechanism
(shuttle, lanyard or equal), excludes socket insert
L5672
F6
#Addition to lower extremity, below knee, removable medial brim suspension
L5673
F6
#Addition to lower extremity, below knee/above knee, custom fabricated from existing mold
or prefabricated, socket insert, silicone gel, elastomeric or equal, for use with locking
mechanism
L5676
F4
#Additions to lower extremity, below knee, knee joints, single axis, pair
L5677
F4
#Additions to lower extremity, below knee, knee joints, polycentric, pair
L5678
F6
#Additions to lower extremity, below knee, joint covers, pair
L5679
F6
#Addition to lower extremity, below knee/above knee, custom fabricated from existing mold
or prefabricated, socket insert, silicone gel, elastomeric or equal, not for use with locking
mechanism
L5680
F6
#Addition to lower extremity, below knee, thigh lacer, non-molded
L5681
F6
#Addition to lower extremity, below knee/above knee, custom fabricated socket insert for
congenital or atypical traumatic amputee, silicone gel, elastomeric or equal, for use with or
without locking mechanism; initial only (for use other than initial, use code L5673 or L5679)
L5682
F6
#Addition to lower extremity, below knee, thigh lacer, gluteal/ischial, molded
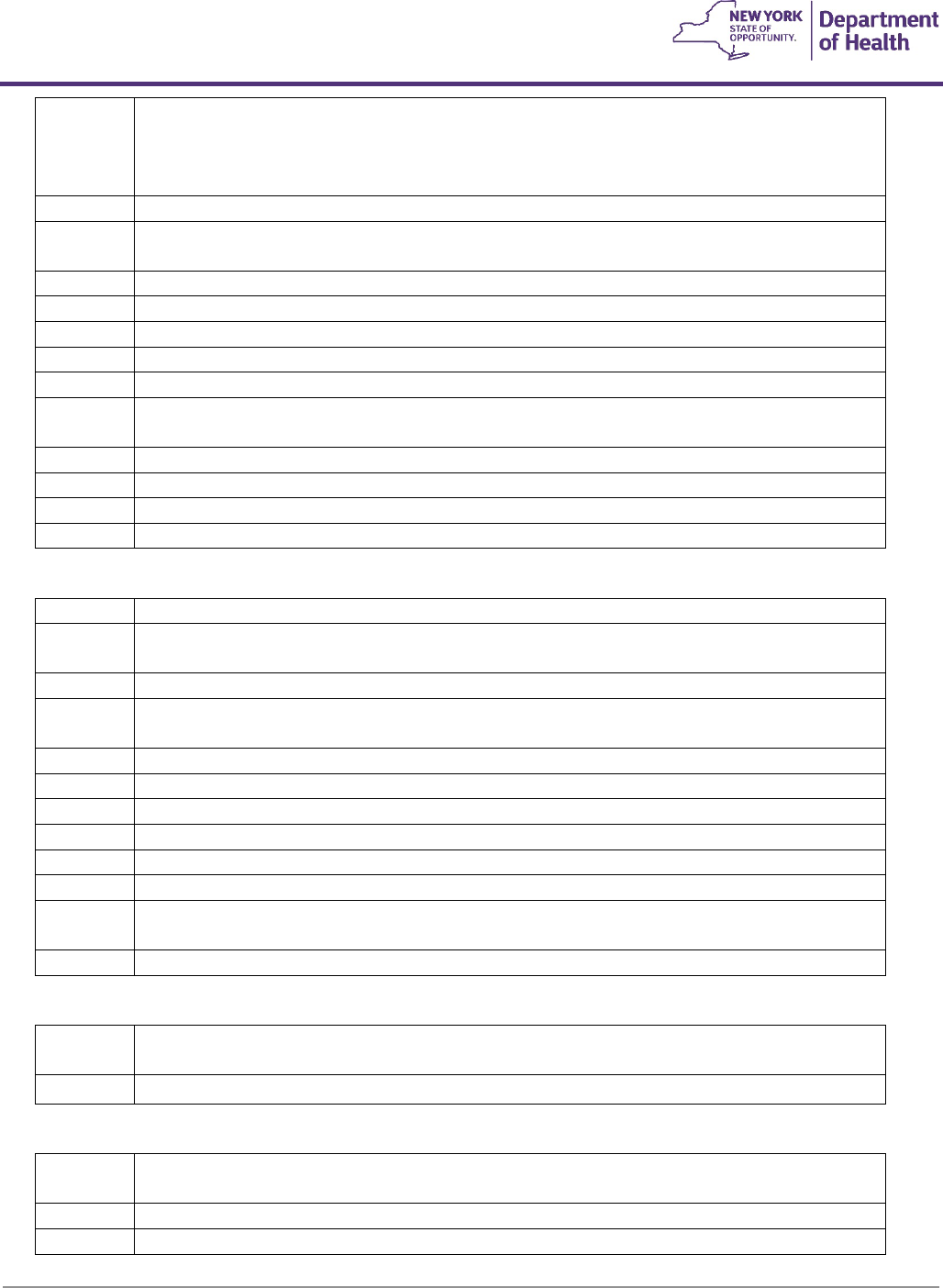
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
120
L5683
F6
#Addition to lower extremity, below knee/above knee, custom fabricated socket insert for
other than congenital or atypical traumatic amputee, silicone gel, elastomeric or equal, for
use with or without locking mechanism, initial only
(for other than initial, use code L5673 or L5679)
L5684
F6
#Addition to lower extremity, below knee, fork strap
L5685
F6
#Addition to lower extremity prosthesis, below knee, suspension/sealing sleeve, with or
without valve, any material, each
L5686
F6
#Addition to lower extremity, below knee, back check (extension control)
L5688
F7
#Addition to lower extremity, below knee, waist belt, webbing
L5690
F7
#Addition to lower extremity, below knee, waist belt, padded and lined
L5692
F7
#Addition to lower extremity, above knee, pelvic control belt, light
L5694
F7
#Addition to lower extremity, above knee, pelvic control belt, padded and lined
L5695
F7
#Addition to lower extremity, above knee, pelvic control, sleeve suspension, neoprene or
equal, each
L5696
F4
#Addition to lower extremity, above knee or knee disarticulation, pelvic joint
L5697
F7
#Addition to lower extremity, above knee or knee disarticulation, pelvic band
L5698
F7
#Addition to lower extremity, above knee or knee disarticulation, Silesian bandage
L5699
F7
#All lower extremity prostheses, shoulder harness
Additions: Feet Ankle Units
L5700
F4
#Replacement, socket, below knee, molded to patient model
L5701
F4
#Replacement, socket, above knee/knee disarticulation, including attachment plate, molded
to patient model
L5702
F4
#Replacement, socket, hip disarticulation, including hip joint, molded to patient model
L5703
F4
#Ankle, symes, molded to patient model, socket without solid ankle cushion heel (SACH)
foot, replacement only
L5704
F6
#Custom shaped protective cover, below knee
L5705
F6
#Custom shaped protective cover, above knee
L5706
F6
#Custom shaped protective cover, knee disarticulation
L5707
F6
#Custom shaped protective cover, hip disarticulation
L5710
F6
#Addition, exoskeletal knee-shin system, single axis, manual lock
L5711
F6
#Additions exoskeletal knee-shin system, single axis, manual lock, ultra-light material
L5712
F6
#Addition, exoskeletal knee-shin system, single axis, friction swing and stance phase control
(safety knee)
L5714
F6
#Addition, exoskeletal knee-shin system, single axis, variable friction swing phase control
Additions: Knee-Shin System
L5716
F6
#Addition, exoskeletal knee-shin system, polycentric, mechanical stance phase lock
L5718
F4
#Addition, exoskeletal knee-shin system, polycentric, friction swing and stance phase control
A fluid or pneumatic knee (L5722-L5780) is covered for member’s whose functional level is 3 or above.
L5722
F4
#Addition, exoskeletal knee-shin system, single axis, pneumatic swing, friction stance phase
control
L5724
F4
#Addition, exoskeletal knee-shin system, single axis, fluid swing phase control
L5726
F4
#Addition, exoskeletal knee-shin system, single axis, external joints, fluid swing phase control
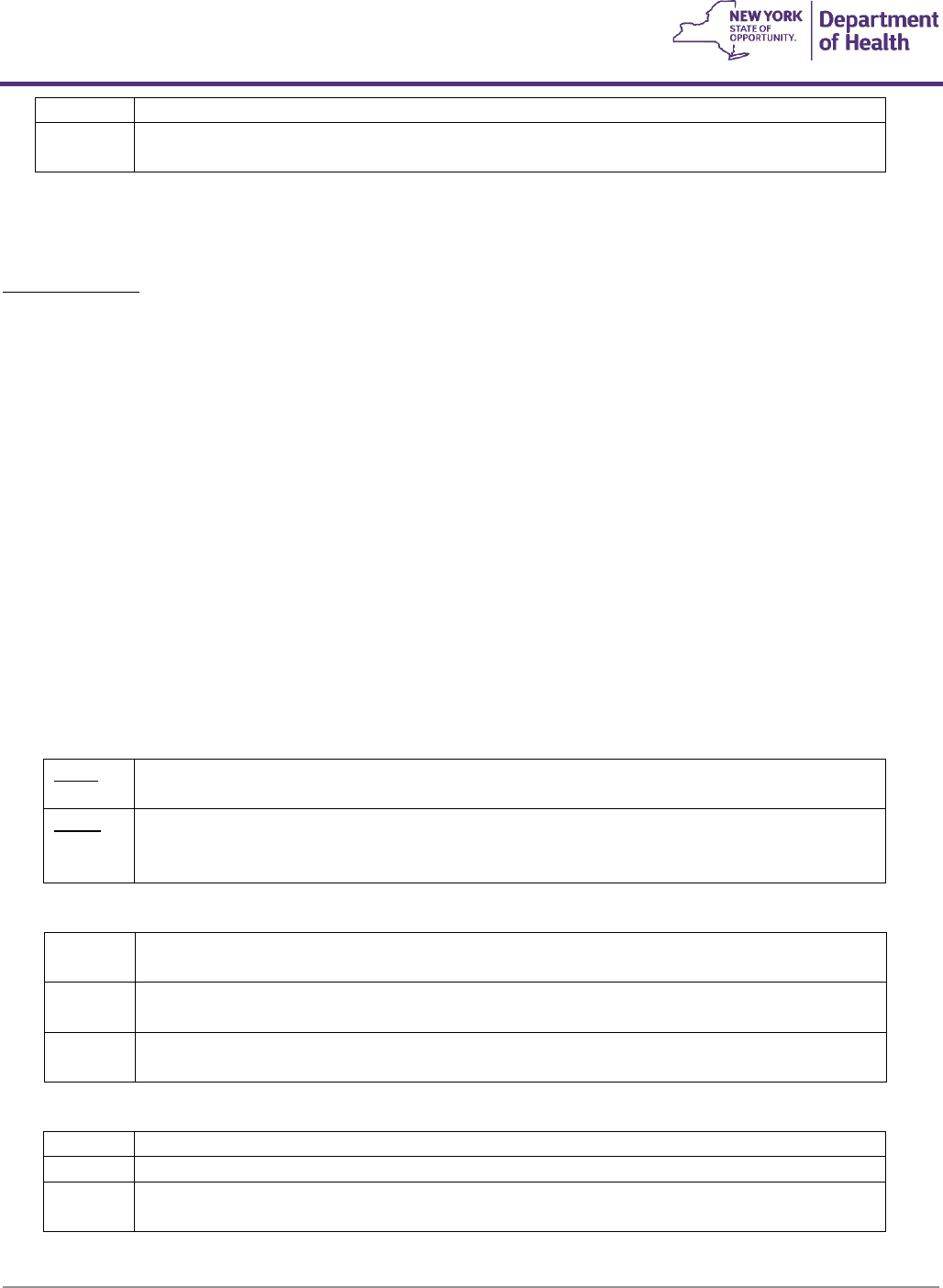
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
121
L5728
F4
#Addition, exoskeletal knee-shin system, single axis, fluid swing and stance phase control
L5780
F4
#Addition, exoskeletal knee-shin system, single axis, pneumatic/hydra pneumatic swing
phase control
Vacuum Pump
Vacuum pump suspension systems may be considered medically necessary when ALL of the following criteria are met:
Coverage Criteria
a. There is a documented clinical condition of volume variation with objective measurements of the residual
limb provided over a period of time (excluding weight gain, weight loss, the normal atrophy process,
growth or systemic issues such as vascular or cardiac issues which would cause volume changes despite
the use of vacuum technology).
b. The need to control residual limb volume is documented (see a. above) and there is a contraindication to
or a failure of other socket suspension systems.
c. The member has adequate cognitive ability to safely and effectively use a vacuum pump and care for it as
required.
d. The member has the physical ability, including adequate cardiovascular and pulmonary capacity for
independent ambulation with a prosthesis in the community (use of the limb in the home or for basic
community ambulation is not sufficient to justify a vacuum pump unless all other less costly alternatives
have been adequately trialed and ruled out with the rationale clearly documented); and
e. There is excessive pistoning of the socket to the residual limb interface that cannot be resolved by
adjustments in the current suspension system; or
f. Excessive residual limb hyperemia from prior socket use; or
g. Excessive skin hyperhidrosis from prior socket use; or
h. Safety issues such as multiple falls in below knee amputees (transtibial amputation).
L5781
F4
Addition to lower limb prosthesis, vacuum pump, residual limb volume management and
moisture evacuation system
L5782
F4
Addition to lower limb prosthesis, vacuum pump, residual limb volume management and
moisture evacuation system, heavy duty
Covered for members with documented weight of more than 300 pounds.
Component Modification
L5785
F4
#Addition, exoskeletal system, below knee, ultra light material (titanium, carbon fiber or
equal)
L5790
F4
#Addition, exoskeletal system, above knee, ultra light material (titanium, carbon fiber or
equal)
L5795
F4
#Addition, exoskeletal system, hip disarticulation, ultra-light material (titanium, carbon fiber
or equal)
Endoskeletal
L5810
F4
#Addition, endoskeletal knee-shin system, single axis, manual lock
L5811
F4
#Addition, endoskeletal knee-shin system, single axis, manual lock, ultra-light material
L5812
F4
#Addition, endoskeletal knee-shin system, single axis, friction swing and stance phase
control (safety knee)
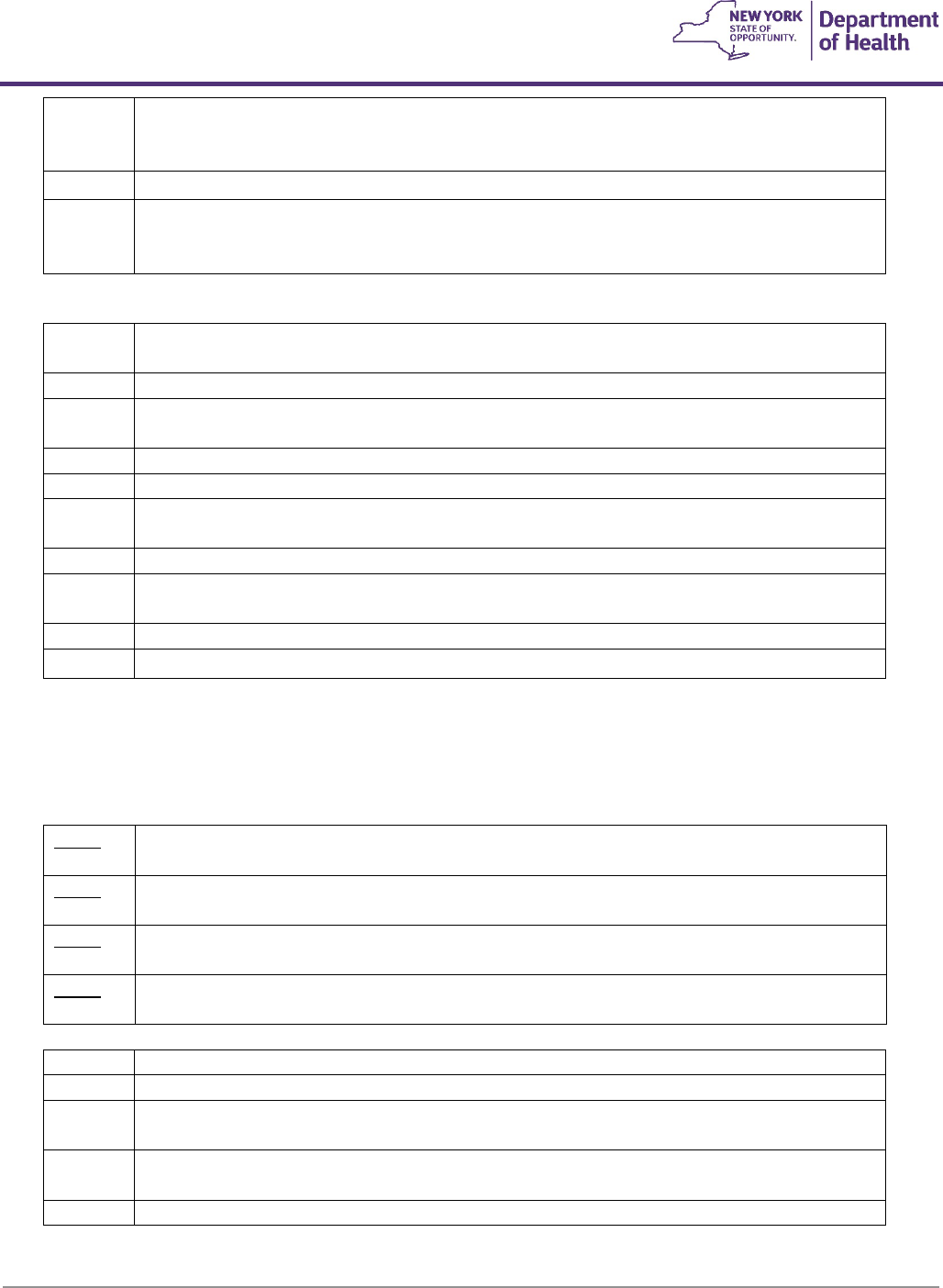
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
122
L5814
F4
#Addition, endoskeletal knee-shin system, polycentric, hydraulic swing phase control,
mechanical stance phase lock
•
Covered for member’s whose functional level is 3 or above.
L5816
F4
#Addition, endoskeletal knee-shin system, polycentric, mechanical stance phase lock
L5818
F4
#Addition, endoskeletal knee-shin system, polycentric, friction swing and stance phase
control
A fluid or pneumatic knee (L5822-L5840) is covered for member’s whose functional level is 3 or above.
L5822
F4
#Addition, endoskeletal knee-shin system, single axis, pneumatic swing, friction stance phase
control
L5824
F4
#Addition, endoskeletal knee-shin system, single axis, fluid swing phase control
L5826
F4
#Addition, endoskeletal knee-shin system, single axis, hydraulic swing phase control, with
miniature high activity frame
L5828
F4
#Addition, endoskeletal knee-shin system, single axis, fluid swing and stance phase control
L5830
F4
#Addition, endoskeletal knee-shin system, single axis, pneumatic/swing phase control
L5840
F4
#Addition, endoskeletal knee-shin system, 4 bar linkage or multiaxial, pneumatic swing
phase control
L5845
F4
#Addition, endoskeletal, knee-shin system, stance flexion feature, adjustable
L5848
F4
#Addition to endoskeletal knee-shin system, fluid stance extension, dampening feature, with
or without adjustability
L5850
F4
#Addition, endoskeletal system, above knee or hip disarticulation, knee extension assist
L5855
F4
#Addition, endoskeletal system, hip disarticulation, mechanical hip extension assist
Electric knees (L5856-L5859) are covered for member’s whose functional level is 3 or above, and when the clinical
documentation establishes why a non-electric knee fails to meet the member’s medical needs and the member’s
maximum functional level cannot be achieved through the use of a non-electric knee. Documentation should include,
at minimum, a detailed specialist (Physiatrist, Therapist, etc.) evaluation and specific objective measures taken during
the trial of both the electric knee and non-electric knee.
L5856
F3
Addition to lower extremity prosthesis, endoskeletal knee-shin system, microprocessor
control feature, swing and stance phase, includes electronic sensor(s), any type
L5857
F3
Addition to lower extremity prosthesis, endoskeletal knee-shin system, microprocessor
control feature, swing phase only, includes electronic sensor(s), any type
L5858
F3
Addition to lower extremity prosthesis, endoskeletal knee shin system, microprocessor
control feature, stance phase only, includes electronic sensor(s), any type
L5859
F3
Addition to lower extremity prosthesis, endoskeletal knee-shin system, powered and
programmable flexion/extension assist control, includes any type motor(s)
L5910
F4
#Addition, endoskeletal system, below knee, alignable system
L5920
F4
#Addition, endoskeletal system, above knee or hip disarticulation, alignable system
L5925
F4
#Addition, endoskeletal system, above knee, knee disarticulation or hip disarticulation,
manual lock
L5926
F4
#Addition to lower extremity prosthesis, endoskeletal, knee disarticulation, above knee, hip
disarticulation, positional rotation unit, any type
L5930
F4
#Addition, endoskeletal system, high activity knee control frame
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
123
A high activity knee control frame (L5930) is covered for patients whose functional
level is 4.
L5940
F4
#Addition, endoskeletal system, below knee, ultra-light material (titanium, carbon fiber or
equal)
L5950
F4
#Addition, endoskeletal system, above knee, ultra-light material (titanium, carbon fiber or
equal)
L5960
F4
#Addition, endoskeletal system, hip disarticulation, ultra-light material (titanium, carbon fiber
or equal)
L5961
F4
#Addition, endoskeletal system, polycentric hip joint, pneumatic or hydraulic control,
rotation control, with or without flexion and/or extension control
L5962
F4
#Addition, endoskeletal system, below knee, flexible protective outer surface covering
system
L5964
F4
#Addition, endoskeletal system, above knee, flexible protective outer surface covering
system
L5966
F4
#Addition, endoskeletal system, hip disarticulation, flexible protective outer surface covering
system
L5968
F3
#Addition to lower limb prosthesis, multiaxial ankle with swing phase active dorsiflexion
feature
Ankle-Foot Systems
- An external keel SACH foot (L5970) or single axis ankle/foot (L5974) is covered for patients whose
functional level is 1 or above.
- A flexible-keel foot or multiaxial ankle/foot (L5978) is covered for patients whose functional level is 2 or
above.
- A microprocessor-controlled ankle foot system (L5973), energy storing foot (L5976), dynamic response foot
with multiaxial ankle (L5979), flex foot system (L5980), flex-walk system or equal (L5981), or shank foot
system with vertical loading pylon (L5987) is covered for patients whose functional level is 3 or above.
- Coverage is extended only if there is sufficient clinical documentation of functional need for the technologic
or design feature of a given type of foot. This information must be retained in the physician's and
prosthetist's files and be available upon request.
L5970
F4
#All lower extremity prostheses, foot, external keel, SACH foot
L5971
F4
#All lower extremity prostheses, solid ankle cushion heel (SACH) foot, replacement only
L5972
F4
#All lower extremity prostheses, foot, flexible keel
L5973
F3
Endoskeletal ankle foot system, microprocessor controlled feature, dorsiflexion
L5974
F4
#All lower extremity prostheses, foot, single axis ankle/foot
L5975
F4
#All lower extremity prostheses, combination single axis ankle and flexible keel foot
L5976
F4
#All lower extremity prostheses, energy storing foot (Seattle Carbon Copy II or equal)
L5978
F4
#All lower extremity prostheses, foot, multi-axial ankle/foot (Gressinger or equal)
L5979
F4
#All lower extremity prostheses, multi-axial ankle, dynamic response foot, one piece system
L5980
F3
All lower extremity prostheses, flex foot system
L5981
F3
All lower extremity prostheses, flex-walk system or equal
L5982
F4
#All exoskeletal lower extremity prostheses, axial rotation unit
L5984
F4
#All endoskeletal lower extremity prostheses, axial rotation unit, with or without adjustability
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
124
L5985
F3
#All endoskeletal lower extremity prostheses, dynamic prosthetic pylon
L5986
F4
#All lower extremity prostheses, multi-axial rotation unit (“MCP” or equal)
L5987
F3
All lower extremity prosthesis, shank foot system with vertical loading pylon
L5988
F4
#Addition to lower limb prosthesis, vertical shock reducing pylon feature
L5990
F4
#Addition to lower extremity prosthesis, user adjustable heel height
L5999
F10
Lower extremity prosthesis, not otherwise specified
Upper Limb
The procedures in this section are considered as base or basic procedures and may be modified by listing procedures
from the “Additions” sections. The base procedures include only standard friction wrist and control cable system unless
otherwise specified.
Partial Hand
L6000
F3
#Partial hand, Robin-Aids, thumb remaining (or equal)
L6010
F3
#Partial hand, Robin-Aids, little and/or ring finger remaining (or equal)
L6020
F3
#Partial hand, Robin-Aids, no finger remaining (or equal)
L6026
F3
Transcarpal/metacarpal or partial hand disarticulation prosthesis, external power, self-
suspended, inner socket with removable forearm section, electrodes and cables, two
batteries, charger, myoelectric control of terminal device, excludes terminal device(s)
Wrist Articulation
L6050
F3
#Wrist disarticulation, molded socket, flexible elbow hinges, triceps pad
L6055
F3
#Wrist disarticulation, molded socket with expandable interface, flexible elbow hinges,
triceps pad
Below Elbow
L6100
F3
#Below elbow, molded socket, flexible elbow hinge, triceps pad
L6110
F3
#Below elbow, molded socket, (Muenster or Northwestern suspension types)
L6120
F3
#Below elbow, molded double wall split socket, step-up hinges, half cuff
L6130
F3
#Below elbow, molded double wall split socket, stump activated locking hinge, half cuff
Elbow Disarticulation
L6200
F3
#Elbow disarticulation, molded socket, outside locking hinge, forearm
L6205
F3
#Elbow disarticulation, molded socket with expandable interface, outside locking hinges,
forearm
Above Elbow
L6250
F3
#Above elbow, molded double wall socket, internal locking elbow, forearm
Shoulder Disarticulation
L6300
F3
#Shoulder disarticulation, molded socket, shoulder bulkhead, humeral section, internal
locking elbow, forearm
L6310
F3
#Shoulder disarticulation, passive restoration (complete prosthesis)
L6320
F3
#Shoulder disarticulation, passive restoration (shoulder cap only)
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
125
Interscapular Thoracic
L6350
F3
#Interscapular thoracic, molded socket, shoulder bulkhead, humeral section, internal locking
elbow, forearm
L6360
F3
#Interscapular thoracic, passive restoration (complete prosthesis)
L6370
F3
#Interscapular thoracic, passive restoration (shoulder cap only)
Immediate and Early Post-Surgical Procedures
L6380
F2
#Immediate post surgical or early fitting, application of initial rigid dressing, including fitting
alignment and suspension of components, and one cast change, wrist disarticulation or
below elbow
L6382
F2
#Immediate post surgical or early fitting, application of initial rigid dressing, including fitting
alignment and suspension of components, and one cast change, elbow disarticulation or
above elbow
L6384
F2
#Immediate post surgical or early fitting, application of initial rigid dressing, including fitting
alignment and suspension of components, and one cast change, shoulder disarticulation or
interscapular thoracic
L6386
F2
#Immediate post surgical or early fitting, each additional cast change and realignment
L6388
F2
#Immediate post surgical or early fitting, application of rigid dressing only
Endoskeletal: Below Elbow
L6400
F2
#Below elbow, molded socket, endoskeletal system, including soft prosthetic tissue shaping
L6883
F3
Replacement socket, below elbow/wrist disarticulation, molded to patient model, for use
with or without external power
Endoskeletal: Elbow Disarticulation
L6450
F2
#Elbow disarticulation, molded socket, endoskeletal system, including soft prosthetic tissue
shaping
Endoskeletal: Above Elbow
L6500
F2
#Above elbow, molded socket, endoskeletal system, including soft prosthetic tissue shaping
L6884
F3
Replacement socket, above elbow/elbow disarticulation, molded to patient model, for use
with or without external power
Endoskeletal: Shoulder Disarticulation
L6550
F2
#Shoulder disarticulation, molded socket endoskeletal system, including soft prosthetic
tissue shaping
L6885
F3
Replacement socket, shoulder disarticulation/interscapular thoracic, molded to patient
model, for use with or without external power
Endoskeletal: Interscapular Thoracic
L6570
F2
#Interscapular thoracic, molded socket, endoskeletal system, including soft prosthetic tissue
shaping
L6580
F2
#Preparatory, wrist disarticulation or below elbow, single wall plastic socket, friction wrist,
flexible elbow hinges, figure of eight harness, humeral cuff, Bowden cable control, "USMC"
or equal pylon, no cover, molded to patient model
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
126
L6582
F2
#Preparatory, wrist disarticulation or below elbow, single wall socket, friction wrist, flexible
elbow hinges, figure of eight harness, humeral cuff, Bowden cable control, “USMC” or equal
pylon, no cover, direct formed
L6584
F2
#Preparatory, elbow disarticulation or above elbow, single wall plastic socket, friction wrist,
locking elbow, figure of eight harness, fair lead cable control, “USMC” or equal pylon, no
cover, molded to patient model
L6586
F2
#Preparatory, elbow disarticulation or above elbow, single wall socket, friction wrist, locking
elbow, figure of eight harness, fair lead cable control, “USMC” or equal pylon, no cover,
direct formed
L6588
F2
#Preparatory, shoulder disarticulation or interscapular thoracic, single wall, plastic socket,
shoulder joint, locking elbow, friction wrist, chest strap, fair lead cable control, “USMC” or
equal pylon, no cover, molded to patient model
L6590
F2
#Preparatory, shoulder disarticulation or interscapular thoracic, single wall socket, shoulder
joint, locking elbow, friction wrist, chest strap, fair lead cable control, “USMC” or equal pylon,
no cover, direct formed
Additions: Upper Limb
Note: The following procedures/modifications/components may be added to other base procedures. The items in this
section should reflect the additional complexity of each modification procedure, in addition to the base procedure, at
the time of the original order.
L6600
F3
#Upper extremity additions, polycentric hinge, pair
L6605
F3
#Upper extremity additions, single pivot hinge, pair
L6610
F3
#Upper extremity additions, flexible metal hinge, pair
L6611
F3
#Addition to upper extremity prosthesis, external powered, additional switch, any type
L6615
F3
#Upper extremity addition, disconnect locking wrist unit
L6616
F3
#Upper extremity addition, additional disconnect insert for locking wrist unit, each
L6620
F3
#Upper extremity addition, flexion-friction wrist unit, with or without friction
L6621
F3
Upper extremity prosthesis addition, flexion/extension wrist with or without friction, for use
with external powered terminal device
L6623
F3
#Upper extremity addition, spring assisted rotational wrist unit with latch release
L6624
F3
Upper extremity addition, flexion/extension and rotation wrist unit
L6625
F3
#Upper extremity addition, rotation wrist unit with cable lock
L6628
F3
#Upper extremity addition, quick disconnect hook adapter, Otto Bock or equal
L6629
F3
#Upper extremity addition, quick disconnect lamination collar with coupling piece, Otto Bock
or equal
L6630
F3
#Upper extremity addition, stainless steel, any wrist
L6632
F3
#Upper extremity addition, latex suspension sleeve, each
L6635
F3
#Upper extremity addition, lift assist for elbow
L6637
F3
#Upper extremity addition, nudge control elbow lock
L6638
F3
Upper extremity addition to prosthesis, electric locking feature, only for use with manually
powered elbow
L6640
F3
#Upper extremity additions, shoulder abduction joint, pair
L6641
F3
#Upper extremity addition, excursion amplifier, pulley type
L6642
F3
#Upper extremity addition, excursion amplifier, lever type
L6645
F3
#Upper extremity addition, shoulder flexion-abduction joint, each
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
127
L6646
F3
Upper extremity addition, shoulder joint, multipositional locking, flexion, adjustable
abduction friction control, for use with body powered or external powered system
L6647
F3
Upper extremity addition, shoulder lock mechanism, body powered actuator
L6648
F3
Upper extremity addition, shoulder lock mechanism, external powered actuator
L6650
F4
#Upper extremity addition, shoulder universal joint, each
L6655
F4
#Upper extremity addition, standard control cable, extra
L6660
F4
#Upper extremity addition, heavy duty control cable
L6665
F6
#Upper extremity addition, Teflon, or equal, cable lining
L6670
F4
#Upper extremity addition, hook to hand, cable adapter
L6672
F4
#Upper extremity addition, harness, chest or shoulder, saddle type
L6675
F4
#Upper extremity addition, harness, (e.g. figure of eight type) single cable design
L6676
F4
#Upper extremity addition, harness, (e.g. figure of eight type) dual cable design
L6677
F4
#Upper extremity addition, harness, triple control, simultaneous operation of terminal device
and elbow
L6680
F3
#Upper extremity addition, test socket, wrist disarticulation or below elbow
L6682
F3
#Upper extremity addition, test socket, elbow disarticulation or above elbow
L6684
F3
#Upper extremity addition, test socket, shoulder disarticulation or interscapular thoracic
L6686
F3
#Upper extremity addition, suction socket
L6687
F3
#Upper extremity addition, frame type socket, below elbow or wrist disarticulation
L6688
F3
#Upper extremity addition, frame type socket, above elbow or elbow disarticulation
L6689
F3
#Upper extremity addition, frame type socket, shoulder disarticulation
L6690
F3
#Upper extremity addition, frame type socket, interscapular-thoracic
L6691
F6
#Upper extremity addition, removable insert, each
L6692
F6
#Upper extremity addition, silicone gel insert or equal, each
L6693
F3
Upper extremity addition, locking elbow, forearm counterbalance
L6694
F6
#Addition to upper extremity prosthesis, below elbow/above elbow, custom fabricated from
existing mold or prefabricated, socket insert, silicone gel, elastomeric or equal, for use with
locking mechanism
L6695
F6
#Addition to upper extremity prosthesis, below elbow/above elbow,
custom fabricated from existing mold or prefabricated, socket insert, silicone gel, elastomeric
or equal, not for use with locking mechanism
L6696
F6
Addition to upper extremity prosthesis, below elbow/above elbow, custom fabricated socket
insert for congenital or atypical traumatic amputee, silicone gel, elastomeric or equal, for use
with or without locking mechanism, initial only (for other than initial, use code L6694 or
L6695)
L6697
F6
Addition to upper extremity prosthesis, below elbow/above elbow, custom fabricated socket
insert for other than congenital or atypical traumatic amputee, silicone gel, elastomeric or
equal, for use with or without locking mechanism, initial only (for other than initial, use code
L6694 or L6695)
L6698
F6
#Addition to upper extremity prosthesis, below elbow/above elbow, lock mechanism,
excludes socket insert
Terminal Devices
Hooks
L6703
F3
#Terminal device, passive hand/mitt, any material, any size

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
128
L6706
F3
#Terminal device, hook, mechanical, voluntary opening, any material, any size, lined or
unlined
L6707
F3
#Terminal device, hook, mechanical, voluntary closing, any material, any size, lined or
unlined
L6708
F3
#Terminal device, hand, mechanical, voluntary opening, any material, any size
L6709
F3
#Terminal device, hand, mechanical, voluntary closing, any material, any size
L6711
F3
Terminal device, hook, mechanical, voluntary opening, any material, any size, lined or
unlined, pediatric
L6712
F3
Terminal device, hook, mechanical, voluntary closing, any material, any size, lined or unlined,
pediatric
L6713
F3
Terminal device, hand, mechanical, voluntary opening, any material, any size, pediatric
L6714
F3
Terminal device, hand, mechanical, voluntary closing, any material, any size, pediatric
L6715
F3
Terminal device, multiple articulating digit, includes motor(s), initial issue or replacement
L6721
F3
Terminal device, hook or hand, heavy duty, mechanical, voluntary opening, any material, any
size, lined or unlined
L6722
F3
Terminal device, hook or hand, heavy duty, mechanical, voluntary closing, any material, any
size, lined or unlined
L6805
F3
#Addition to terminal device, modifier wrist unit
L6810
F3
#Addition to terminal device, precision pinch device
Hands
L6880
F3
Electric hand, switch or myoelectric controlled, independently articulating digits, any grasp
pattern or combination of grasp patterns, includes motor(s)
L6881
F3
Automatic grasp feature, addition to upper limb electric prosthetic terminal device
L6882
F3
Microprocessor control feature, addition to upper limb prosthetic terminal device
Gloves For Above Hands
L6890
F6
#Addition to upper extremity prosthesis, glove for terminal device, any material,
prefabricated, includes fitting and adjustment
L6895
F6
#Addition to upper extremity prosthesis, glove for terminal device, any material, custom
fabricated
Hand Restoration
L6900
F3
#Hand restoration (casts, shading and measurements included), partial hand, with glove,
thumb or one finger remaining
L6905
F3
#Hand restoration (casts, shading and measurements included), partial hand, with glove,
multiple fingers remaining
L6910
F3
#Hand restoration (casts, shading and measurements included), partial hand, with glove, no
fingers remaining
L6915
F3
#Hand restoration (shading and measurements included), replacement glove for above
External Power
Base Devices
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
129
L6920
F3
Wrist disarticulation, external power, self-suspended inner socket, removable forearm shell,
Otto Bock or equal, switch, cables, two batteries and one charger, myoelectric control of
terminal device
L6925
F3
Wrist disarticulation, external power, self-suspended inner socket, removable forearm shell,
Otto Bock or equal electrodes, cables, two batteries and one charger, myoelectric control of
terminal device
L6930
F3
Below elbow, external power, self-suspended inner socket, removable forearm shell, Otto
Bock or equal switch, cables, two batteries and one charger, switch control of terminal device
L6935
F3
Below elbow, external power, self-suspended inner socket, removable forearm shell, Otto
Bock or equal electrodes, cables, two batteries and one charger, myoelectronic control of
terminal device
L6940
F3
Elbow disarticulation, external power, molded inner socket, removable humeral shell, outside
locking hinges, forearm, Otto Bock or equal switch, cables, two batteries and one charger,
switch control of terminal device
L6945
F3
Elbow disarticulation, external power, molded inner socket, removable humeral shell, outside
locking hinges, forearm, Otto Bock or equal electrodes, cables, two batteries and one
charger, myoelectronic control of terminal device
L6950
F3
Above elbow, external power, molded inner socket, removable humeral shell, internal locking
elbow, forearm, Otto Bock or equal switch, cables, two batteries and one charger, switch
control of terminal device
L6955
F3
Above elbow, external power, molded inner socket, removable humeral shell, internal locking
elbow, forearm, Otto Bock or equal electrodes, cables, two batteries and one charger,
myoelectronic control of terminal device
L6960
F3
Shoulder disarticulation, external power, molded inner socket, removable shoulder shell,
shoulder bulkhead, humeral section, mechanical elbow, forearm, Otto Bock or equal switch,
cables, two batteries and one charger, switch control of terminal device
L6965
F3
Shoulder disarticulation, external power, molded inner socket, removable shoulder shell,
shoulder bulkhead, humeral section, mechanical elbow, forearm, Otto Bock or equal
electrodes, cables, two batteries and one charger, myoelectric control of terminal device
L6970
F3
Interscapular-thoracic, external power, molded inner socket, removable shoulder shell,
shoulder bulkhead, humeral section, mechanical elbow, forearm, Otto Bock or equal switch,
cables, two batteries and one charger, switch control of terminal device
L6975
F3
Interscapular-thoracic, external power, molded inner socket, removable shoulder shell,
shoulder bulkhead, humeral section, mechanical elbow, forearm, Otto Bock or equal
electrodes, cables, two batteries and one charger, myoelectronic control of terminal device
L7007
F3
Electric hand, switch or myoelectric controlled, adult
L7008
F3
Electric hand, switch or myoelectric controlled, pediatric
L7009
F3
Electric hook, switch or myoelectric controlled, adult
L7040
F3
Prehensile actuator, switch controlled
L7045
F3
Electric hook, switch or myoelectric controlled, pediatric
Myoelectric
To be used only when medically necessary as determined by an approved amputee clinic.
Elbow
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
130
L7170
F3
Electronic elbow, Hosmer or equal, switch controlled
L7180
F3
Electronic elbow, microprocessor sequential control of elbow and terminal device
L7181
F3
Electronic elbow, microprocessor simultaneous control of elbow and terminal device
L7185
F3
Electronic elbow, adolescent, Variety Village or equal, switch controlled
L7186
F3
Electronic elbow, child, Variety Village or equal, switch controlled
L7190
F3
Electronic elbow, adolescent, Variety Village or equal, myoelectronically controlled
L7191
F3
Electronic elbow, child, Variety Village or equal, myoelectronically controlled
L7259
F3
Electronic wrist rotator, any type
Battery Components
L7360
F7
#Six volt battery, each
L7362
F4
#Battery charger, six volt, each
L7364
F7
#Twelve volt battery, each
L7366
F4
#Battery charger, twelve volt, each
L7367
F7
#Lithium ion battery, rechargeable, replacement
L7368
F4
#Lithium ion battery charger (Replacement only)
Additions to Upper Extremity Prosthetics
L7400
F4
#Addition to upper extremity prosthesis, below elbow/wrist disarticulation, ultralight material
(titanium, carbon fiber or equal)
L7401
F4
#Addition to upper extremity prosthesis, above elbow disarticulation, ultralight material
(titanium, carbon fiber or equal)
L7402
F4
#Addition to upper extremity prosthesis, shoulder disarticulation/interscapular thoracic,
ultralight material (titanium, carbon fiber or equal)
L7403
F4
#Addition to upper extremity prosthesis, below elbow/wrist disarticulation, acrylic material
L7404
F4
#Addition to upper extremity prosthesis, above elbow disarticulation, acrylic material
L7405
F4
#Addition to upper extremity prosthesis, shoulder disarticulation/interscapular thoracic,
acrylic material
L7499
F10
Upper extremity prosthesis, not otherwise specified
Repairs
L7510
F7
#Repair of prosthetic device, repair or replace minor parts
(not to be billed in conjunction with L7520)
L7520
F9
#Repair prosthetic device, labor component, per 15 minutes
(includes evaluation) (more than 2 hours requires prior approval)
Prosthetic Supplies
L7700
F6
#Gasket or seal, for use with prosthetic socket insert, any type, each
Prosthetic Socks
L8400
F21
#Prosthetic sheath, below knee, each
L8410
F21
#Prosthetic sheath, above knee, each
L8415
F21
#Prosthetic sheath, upper limb, each
L8417
F21
#Prosthetic sheath/sock, including a gel cushion layer, below knee or above
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
131
L8420
F21
#Prosthetic sock, multiple ply, below knee, each
L8430
F21
#Prosthetic sock, multiple ply, above knee, each
L8435
F21
#Prosthetic sock, multiple ply, upper limb, each
L8440
F21
#Prosthetic shrinker, below knee, each
L8460
F21
#Prosthetic shrinker, above knee, each
L8465
F21
#Prosthetic shrinker, upper limb, each
L8470
F21
#Prosthetic sock, single ply, fitting, below knee, each
L8480
F21
#Prosthetic sock, single ply, fitting, above knee, each
L8485
F21
#Prosthetic sock, single ply, upper limb, each
L8499
F10
Unlisted procedure for miscellaneous prosthetic services
L9900
F12
#Orthotic and prosthetic supply, accessory, and/or service component of another HCPCS L
code (limited to home visit)
Breast And Hair Prosthesis
L8010
F21
#Breast prosthesis, mastectomy sleeve
L8035
F6
Custom breast prosthesis, post mastectomy, molded to patient model
- L8035 describes a molded-to-patient-model custom breast prosthesis.
- History of breast malignancy, post-mastectomy/partial mastectomy/lumpectomy, or
acquired absence of breast(s)
- Custom breast prosthetics will only be considered when all less costly prefabricated
off-the-shelf options have been trialed and have been demonstrated to not meet
the member’s medical needs.
- The medical necessity for the additional features of a custom fabricated prosthesis
compared to prefabricated must be clearly documented by the ordering provider.
- Custom breast prosthetics requested for cosmetic purposes only are not medically
necessary and are non-covered.
A9282
F2
Wig, any type, each (Coverage limited to medically-induced or congenital hair loss.)
Lower Extremity Compression Supports
Covered for venous or lymphatic impairment.
Non-Custom
- Prefabricated elastic support garment that applies varying pressure gradients to an area.
- Prefabricated garments are available in various sizes, and different levels of compression.
- Prefabricated garments with appropriate level of compression (determined by the ordering provider) should
be requested before custom is considered if the member’s limb measurements fit within the size ranges
specified by the manufacturers of the garment. Various manufacturers should be explored.
Custom
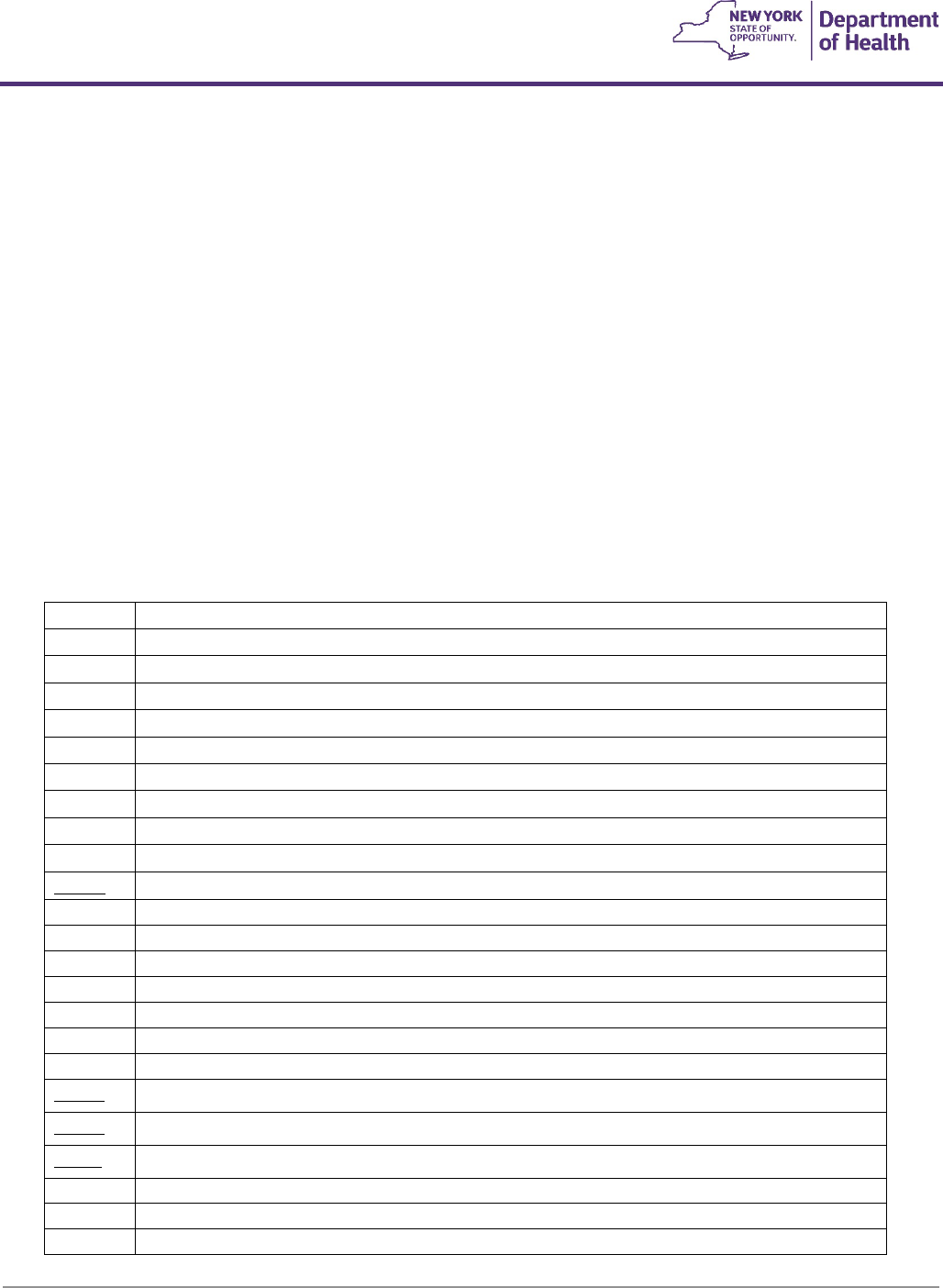
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
132
- Custom-made gradient compression stockings/garments are fabricated to the exact specifications of an
individual.
- Custom made are considered medically necessary when the degree of gradient pressure is one that cannot be
provided in a prefabricated garment, or the measurements fall outside the ranges of prefabricated garments.
- Custom HCPCS codes and fees include zippered compression garments.
Documentation Requirements
- A physician’s fiscal order indicating the specific level of compression in mm/Hg, specific style, type, and hosiery
knit, and any additional accessories/options.
- Ordering provider’s letter of medical necessity should include medical history, related diagnoses, duration and
extent of current symptoms, any neurological involvement of affected limbs, ambulation status and degree of
assistance required.
- Current and previous decompression treatment modalities utilized and member’s compliance and medical
outcomes.
- Detailed limb/body measurements obtained from a certified fitter or LANA certified therapist, and date
measured. Indicate the location and degree of edematous lobules, if present.
A6530
F7
#Gradient compression stocking, below knee, 18-30 mm Hg each
A6533
F7
#Gradient compression stocking, thigh length, 18-30 mm Hg, each
A6534
F7
#Gradient compression stocking, thigh length, 30-40 mm Hg, each
A6535
F7
#Gradient compression stocking, thigh length, 40-50 mm Hg, each
A6536
F7
#Gradient compression stocking, full length/chap style, 18-30 mm Hg
A6537
F7
#Gradient compression stocking, elastic, full length/chap style 30-40 mm Hg, each
A6538
F7
#Gradient compression stocking, full length/chap style, 40-50 mm Hg, each
A6539
F7
#Gradient compression stocking, waist length, 18-30 mm Hg, each (panty hose style)
A6540
F7
#Gradient compression stocking, waist length, 30-40 mm Hg, each (panty hose style)
A6541
F7
#Gradient compression stocking, waist length, 40-50 mm Hg, each (panty hose style)
A6549
F7
Gradient compression stocking, not otherwise specified
A6552
F7
#Gradient compression stocking, below knee, 30-40 mmhg, each
A6553
F7
#Gradient compression stocking, below knee, 30-40 mmhg, custom, each
A6554
F7
#Gradient compression stocking, below knee, 40 mmhg or greater, each
A6555
F7
#Gradient compression stocking, below knee, 40 mmhg or greater, custom, each
A6556
F7
#Gradient compression stocking, thigh length, 18-30 mmhg, custom, each
A6557
F7
#Gradient compression stocking, thigh length, 30-40 mmhg, custom, each
A6558
F7
#Gradient compression stocking, thigh length, 40 mmhg or greater, custom, each
A6559
F7
Gradient compression stocking, full length/chap style, 18-30 mmhg, custom, each
A6560
F7
Gradient compression stocking, full length/chap style, 30-40 mmhg, custom, each
A6561
F7
Gradient compression stocking, full length/chap style, 40 mmhg or greater, custom, each
A6562
F7
#Gradient compression stocking, waist length, 18-30 mmhg, custom, each
A6563
F7
#Gradient compression stocking, waist length, 30-40 mmhg, custom, each
A6564
F7
#Gradient compression stocking, waist length, 40 mmhg or greater, custom, each
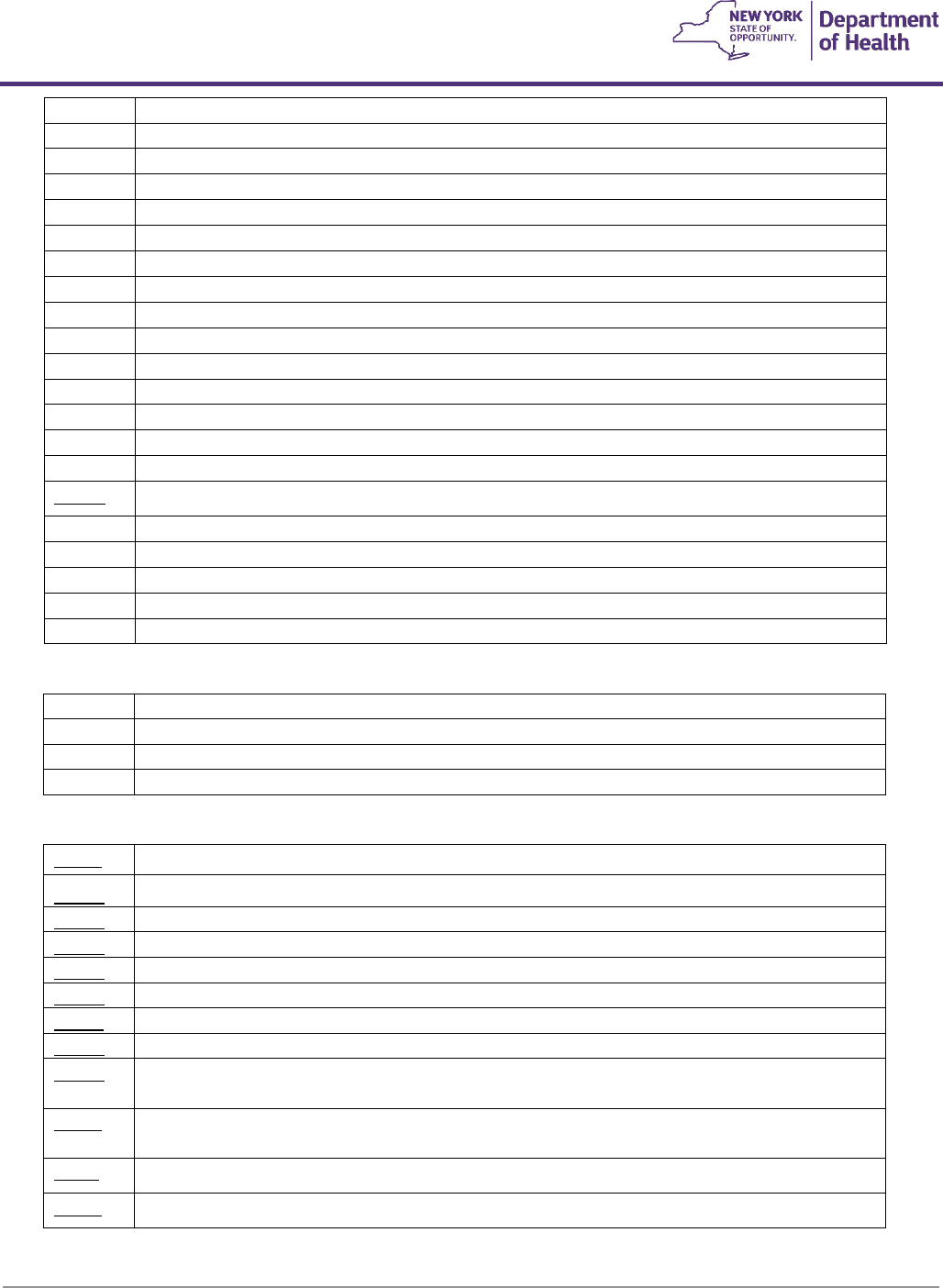
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
133
A6565
F7
#Gradient compression gauntlet, custom, each
A6568
F7
#Gradient compression garment, torso and shoulder, each
A6569
F7
#Gradient compression garment, torso/shoulder, custom, each
A6572
F7
#Gradient compression garment, toe caps, each
A6573
F7
#Gradient compression garment, toe caps, custom, each
A6574
F7
#Gradient compression arm sleeve and glove combination, custom, each
A6575
F7
#Gradient compression arm sleeve and glove combination, each
A6576
F7
#Gradient compression arm sleeve, custom, medium weight, each
A6577
F7
#Gradient compression arm sleeve, custom, heavy weight, each
A6578
F7
#Gradient compression arm sleeve, each
A6579
F7
#Gradient compression glove, custom, medium weight, each
A6580
F7
#Gradient compression glove, custom, heavy weight, each
A6581
F7
#Gradient compression glove, each
A6582
F7
#Gradient compression gauntlet, each
A6583
F7
#Gradient compression wrap with adjustable straps, below knee, 30-50 mmhg, each
A6584
F7
Gradient compression wrap with adjustable straps, not otherwise specified
A6585
F7
#Gradient pressure wrap with adjustable straps, above knee, each
A6586
F7
#Gradient pressure wrap with adjustable straps, full leg, each
A6587
F7
#Gradient pressure wrap with adjustable straps, foot, each
A6588
F7
#Gradient pressure wrap with adjustable straps, arm, each
A6610
F7
#Gradient compression stocking, below knee, 18-30 mmhg, custom, each
Trusses
L8300
F6
#Truss, single with standard pad
L8310
F6
#Truss, double with standard pads
L8320
F6
#Truss, addition to standard pad, water pad
L8330
F6
#Truss, addition to standard pad, scrotal pad
Burn Garments
A6501
F7
Compression burn garment, bodysuit (head to foot), custom fabricated
A6502
F7
Compression burn garment, chin strap, custom fabricated
A6503
F7
Compression burn garment, facial hood, custom fabricated
A6504
F7
Compression burn garment, glove to wrist, custom fabricated
A6505
F7
Compression burn garment, glove to elbow, custom fabricated
A6506
F7
Compression burn garment, glove to axilla, custom fabricated
A6507
F7
Compression burn garment, foot to knee length, custom fabricated
A6508
F7
Compression burn garment, foot to thigh length, custom fabricated
A6509
F7
Compression burn garment, upper trunk to waist including arm openings (vest), custom
fabricated
A6510
F7
Compression burn garment, trunk, including arms down to leg openings (leotard), custom
fabricated
A6511
F7
Compression burn garment, lower trunk including leg openings (panty), custom fabricated
A6512
F7
Compression burn garment, not otherwise classified
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
134
Definitions
As used in Medicaid Durable Medical Equipment Guidelines:
Actuator – A motor that operates a specific function of a power seating system – i.e., tilt, recline, power sliding back,
elevating leg rest(s), seat elevation, or standing
Alternative Control Device – A device that transforms a user’s drive commands by physical actions initiated by the
user to input control directions to a power wheelchair that replaces a standard proportional joystick. Includes: mini-
proportional, compact, or short throw joysticks, head arrays, sip and puff and other types of different input control
devices
Augmentative Communication Systems – A composite of communications components that may include, but are
not limited to, communication devices, manual signs, and communication strategies
Captain’s Chair – A one or two-piece automotive-style seat with rigid frame, cushioning material in both seat and
back sections, covered in cloth, vinyl, leather or equal as upholstery, and designed to serve as a complete seating,
support, and cushioning system for the user. It may have armrests that can be fixed, swing away, or detachable. It
may or may not have a headrest, either integrated or separate
Combination skin protection and positioning seat cushion – A standard or customized seat cushion which has the
following features listed in (a) or (b), and (c), (d), and (e):
(a) Two or more of the following features which must be at least 25 mm in height in the pre-loaded state. Included
in this definition are cushions which have a planar surface but have positioning features within the cushion which are
made of a firmer material than the surface material:
• A pre-ischial bar or ridge which is placed anterior to the ischial tuberosities and prevents forward migration
of the pelvis,
• Two lateral pelvic supports which are placed posterior to the trochanters and are intended to maintain the
pelvis in a centered position in the seat and/or provide lateral stability to the pelvis,
• A medial thigh support which is placed in contact with the adductor region of the thigh and provides the
prescribed amount of abduction and prevents adduction of the thighs,
• Two lateral thigh supports which are placed anterior to the trochanters and provide lateral stability to the
lower extremities and prevent unwanted abduction of the thighs, or
(b) It has two or more air compartments located in areas which address postural asymmetries, each of which must
have a cell height of at least 50 mm, must allow the user to add or remove air, and must have a valve which retains
the desired air volume.
(c) It has a removable vapor permeable or waterproof cover, or it has a waterproof surface; and
(d) It has a permanent label indicating the model and the manufacturer; and
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
135
(e) It has a warranty that provides for repair or full replacement if manufacturing defects are identified, or the surface
does not remain intact due to normal wear within 18 months
Communication Devices – A general term used to describe a primary unit such as communication
software/programs, speech generating device, manual board, or electro larynx, and accessories including but not
limited to application programs, language symbols, interfaces, overlays, cables, and mounts
Crash Testing – Successful completion of WC-19 testing
Cross Brace Chair – A type of construction for a power wheelchair in which opposing rigid braces hinge on pivot
points to allow the device to fold
Custom fabricated seat or back cushion – Individually made for a specific patient starting with basic materials, may
include certain prefabricated components (e.g., gel or multi-cellular air inserts) which may not be billed separately.
(a) liquid foam or a block of foam and
(b) sheets of fabric or liquid coating material.
(c) The cushion must be fabricated using molded-to-recipient-model technique, direct molded-to-recipient
technique, CAD-CAM technology, or detailed measurements of the recipient used to create a configured cushion.
(d) The cushion must have structural features that significantly exceed the minimum requirements for a seat or back
positioning cushion. The cushion must have a removable vapor permeable or waterproof cover, or it must have a
waterproof surface
Custom-fitted/customized – means componentry made or added to already existing model or device that is
assembled, adjusted, or modified to fit the member’s body
Custom-made – is fabricated solely for a particular patient from raw materials which cannot be readily changed to
conform to another patient. These materials are used to create the item from patient measurements or patterns.
Custom-made requires that the member be measured for the custom-made item so that it can be fabricated from
these measurements
Dedicated Speech Generating Device (DSGD) – Devices used as a medically necessary speech aid that is designed,
manufactured, and utilized for the sole purpose of generating speech, primarily and customarily used for medical
purposes, provides an individual who has a severe speech impairment with the ability to meet functional speaking
needs, and is used solely by the individual who has a severe speech impairment. The device is only intended to
perform speech generating functions for the life of the device and cannot by altered by the average consumer to
perform non-speech generating functions. DSGD’s may have digitized speech output using pre-recorded messages
with defined recording times or may have synthesized speech output, which requires message formulation by
spelling and device access by physical contact with the device-direct selection technique or multiple methods of
device access

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
136
Durable Medical Equipment – are devices and equipment, other than prosthetic or orthotic appliances, which have
been ordered by a practitioner in the treatment of a specific medical condition and which have all the following
characteristics:
• Can withstand repeated use for a protracted period of time,
• Are primarily and customarily used for medical purposes,
• Are generally not useful in the absence of an illness or injury,
• Are not usually fitted, designed, or fashioned for a particular individual’s use,
• Where equipment is intended for use by only one patient, it may be either custom-made or
customized
Dynamic Stability Incline – The minimum degree of slope at which the PMD in the most common seating and
positioning configuration(s) remains stable at the required patient weight capacity. If the PMD is stable at only one
configuration, the PMD may have protective mechanisms that prevent climbing inclines in configurations that may
be unstable
Expandable Controller – An electronic system that is capable of accommodating one or more of the following
additional functions:
• Proportional input devices (e.g., mini, compact, or short throw joysticks, touch pads, chin control, head
control, etc.) other than a standard proportional joystick.
• Non-proportional input devices (e.g., sip and puff, head array, etc.)
• Operate 3 or more powered seating actuators through the drive control. (Note: Control of the power
seating actuators though the Control Input Device would require the use of an additional component,
E2310 or E2311.)
An expandable controller may also be able to operate one or more of the following:
• A separate display (i.e., for alternate control devices)
• Other electronic devices (e.g., control of an augmentative speech device or computer through the chair’s
drive control)
• An attendant control
Foot-Ankle Padded Positioning Strap – A padded foot positioning strap that wraps around the ankle and attaches to
the wheelchair footplates. The purpose of a FAPPS is to prevent unwanted inversion, eversion, extension or lifting of
the foot, thereby reducing joint stress and increasing tolerance for positioning, creating a dynamic foot positioning
system
General Use Back Cushion – A prefabricated cushion, which is planar or contoured; and has a removable vapor
permeable or waterproof cover or it has a waterproof surface; and has a permanent label indicating the model and
the manufacturer; and has a warranty that provides for repair or full replacement if manufacturing defects are
identified, or the surface does not remain intact due to normal wear within 12 months

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
137
General Use Seat Cushion – A prefabricated cushion with a removable vapor permeable or waterproof cover or has
a waterproof surface; and has a permanent label indicating the model and the manufacturer; and has a warranty
that provides for repair or full replacement if manufacturing defects are identified, or the surface does not remain
intact due to normal wear within 12 months
Highway Use – Mobility devices that are powered and configured to operate legally on public streets
Integral Control System – Non-expandable wheelchair control system where the joystick is housed in the same box
as the controller. The entire unit is located and mounted near the hand of the user. A direct electrical connection is
made from the Integral Control box to the motors and batteries through a high-power wire harness
Multiple Power Options – A category of PWCs with the capability to accept and operate a combination power tilt
and recline seating system. It may also be able to accommodate power elevating leg rests. A PWC does not have to
accommodate all features to qualify for this code
No Power Options – A category of PWCs that is incapable of accommodating a power tilt, recline, seat elevation, or
standing system. If a PWC can only accept power elevating leg rests, it is considered to be a No Power Option chair
Non-Dedicated Speech Generating Device (non-DSGD) – Devices with one or more of the following characteristics:
a. The capability (locked or unlocked) of running software for purposes other than speech generation (e.g.: devices
that can also run work processing package, an accounting program, or perform other non-medical functions); or
b. Laptop computers, desktop computers, tablet computers, cell phones, or personal digital assistants, which may be
programmed to perform the same function as a speech generating device, and are therefore not primarily medical
in nature and do not meet the regulatory definition of Durable Medical Equipment
; or
c. A device that is useful to someone without severe speech impairment
Non-Expandable Controller – An electronic system that controls the speed and direction of the power wheelchair
drive mechanism. Only a standard proportional joystick (used for hand or chin control) can be used as the input
device. This system may be in the form of an integral controller or a remotely placed controller. The non-expandable
controller may have the ability to control up to 2 power seating actuators through the drive control (for example,
seat elevator and single actuator power elevating leg rests). (Note: Control of the power seating actuators though
the Control Input Device would require the use of an additional component, E2310 or E2311.) May also allow for the
incorporation of an attendant control
Non-Proportional Control Input Device – A device that transforms a user's discrete drive command (a physical
action initiated by the wheelchair user, such as activation of a switch) into perceptually discrete changes in the
wheelchair's speed, direction, or both
Obstacle Climb – Vertical height of a solid obstruction that can be climbed using the standing and/or 0.5-meter run-
up RESNA test

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
138
Patient Weight Capacity – The terms Standard Duty, Heavy Duty, etc., refer to weight capacity, not performance. For
example, the term Group 3 heavy duty power wheelchair denotes that the PWC has Group 3 performance
characteristics and patient weight handling capacity between 301 and 450 pounds. A device is not required to carry
all the weight listed in the class of devices but must have a patient weight capacity within the range to be included.
For example, a PMD that has a weight capacity of 400 pounds is coded as a Heavy-Duty device
Performance Testing – Term used to denote the RESNA based test parameters used to test PMDs. The PMD is
expected to meet or exceed the listed performance and durability figures for the category in which it is to be used
when tested. There is no requirement to test the PMD with all possible accessories
Portable – A category of devices with lightweight construction or ability to disassemble into lightweight components
that allows easy placement into a vehicle for use in a distant location
Positioning back cushion – A standard cushion customized to include materials or components that may be added,
removed and or fabricated from commercially available components to help address orthopedic deformities or
postural asymmetries. Included in this definition are cushions which have a planar surface but have positioning
features within the cushion which are made of a firmer material than the surface material. In addition, the back
cushion has the following characteristics:
(a) There is at least 25 mm of posterior contour in the pre-loaded state. A posterior contour is a backward curve
measured from a vertical line in the midline of the cushion; and
(b) For posterior-lateral cushions and for planar cushions with lateral supports there is at least 75 mm of lateral
contour in the pre-loaded state. A lateral contour is backward curve measured from a horizontal line connecting the
lateral extensions of the cushion; and
(c) For posterior pelvic cushions there is mounting hardware that is adjustable for vertical position, depth, and angle,
and
(d) It has a removable vapor permeable or waterproof cover, or it has a waterproof surface; and
(e) The cushion and cover meet the minimum standards of the California Bulletin 117 or 133 for flame resistance; and
(f) It has a permanent label indicating the model and the manufacturer; and
(g) It has a warranty that provides for repair or full replacement if manufacturing defects are identified, or the
surface does not remain intact due to normal wear within 18 months
Positioning seat cushion – May have materials or components that can be added or removed (customized) to help
address orthopedic deformities or postural asymmetries and has the following characteristics listed in a or b and c
and d:
(a) Two or more
of the following features which must be at least 25 mm in height in the pre-loaded state. Included
in this definition are cushions which have a planar surface but have positioning features within the cushion which are
made of a firmer material than the surface material:
• A pre-ischial bar or ridge (e.g., anti-thrust) which is placed anterior to the ischial tuberosities and prevents
forward migration of the pelvis,

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
139
• Two lateral pelvic supports which are placed posterior to the trochanters and are intended to maintain the
pelvis in a centered position in the seat and/or provide lateral stability to the pelvis,
• A medial thigh support (e.g., built-in pommel) which is placed in contact with the adductor region of the
thigh and provides the prescribed amount of abduction and prevents adduction of the thighs,
• Two lateral thigh supports which are placed anterior to the trochanters and provide lateral stability to the
lower extremities and prevent unwanted abduction of the thighs: or
(b) Two or more air compartments located in areas which address postural asymmetries, each of which must have a
cell height of at least 50 mm, must allow the user to add or remove air, and must have a valve which retains the
desired air volume; and
(c) A permanent label indicating the model and the manufacturer; and
(d) A warranty that provides for repair or full replacement if manufacturing defects are identified or the surface does
not remain intact due to normal wear within 18 months
Power Mobility Device (PMD) – Base codes include both integral frame and modular construction type power
wheelchairs (PWCs) and power operated vehicles (POVs)
Power Operated Vehicle – Chair-like battery powered mobility device for people with difficulty walking due to illness
or disability, with integrated seating system, tiller steering, and four-wheel non-highway construction
Power Options – Tilt, recline, elevating leg rests, seat elevators, or standing systems that may be added to a PWC to
accommodate a patient’s specific need for seating assistance
Power Wheelchair – Chair-like battery powered mobility device for people with difficulty walking due to illness or
disability, with integrated or modular seating system, electronic steering, and four or more wheels non-highway
construction
POV Basic Equipment Package – Each POV is to include all these items on initial issue (i.e., no separate
billing/payment at the time of initial issue)
Proportional Control Input Device – A device that transforms a user's drive command (a physical action initiated by
the wheelchair user) into a corresponding and comparative movement, both in direction and in speed, of the
wheelchair. The input device shall be considered proportional if it allows for both a non-discrete directional
command and a non-discrete speed command from a single drive command movement
Push-Rim Activated Power Assist – An option for a manual wheelchair in which sensors in specially designed wheels
determine the force that is exerted by the patient on the wheel. Additional propulsive and/or braking force is then
provided by motors in each wheel. Batteries are included
PWC Basic Equipment Package - Each power wheelchair code is required to include all these items on initial issue
(i.e., no separate billing/payment at the time of initial issue, unless otherwise noted)

Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
140
Radius Pivot Turn – The distance required for the smallest turning radius of the PMD base. This measurement is
equivalent to the “minimum turning radius” specified in the ANSI/RESNA bulletins
Range - Minimum distance acceptable for a given category of devices on a single charge of the batteries. It is to be
determined by the appropriate RESNA test for range
Remotely Placed Controller – Non-expandable or expandable wheelchair control system where the joystick (or
alternative control device) and the controller box are housed in separate locations. The joystick (or alternative
control device) is connected to the controller through a low power wire harness. The separate controller connects
directly to the motors and batteries through a high-power wire harness
Single Power Option – A category of PWC with the capability to accept and operate a power tilt or power recline,
but not a combination power tilt and recline seating system. It may be able to accommodate power elevating leg
rests in combination with a power tilt or power recline. A PMD does not have to be able to accommodate all
features to qualify for this code. For example, a power wheelchair that can only accommodate a power tilt could
qualify for this code
Skin Protection Seat Cushion – A prefabricated cushion with a removable vapor permeable or waterproof cover or a
waterproof surface; and a permanent label indicating the model and the manufacturer; and a warranty that provides
for repair or full replacement if manufacturing defects are identified or the surface does not remain intact due to
normal wear within 18 months
Sling Seat/Back – Flexible cloth, vinyl, leather or equal material designed to serve as the support for buttocks or back
of the user respectively. They may or may not have thin padding but are not intended to provide cushioning or
positioning for the user
Solid Seat Support Base – Used to support a seat cushion, a rigid piece of plastic or other material which is included
with a PWC base and pediatric seating or attached with hardware to the seat frame of a folding wheelchair in place
of a sling seat. A seat cushion is placed on top of the solid support base
Speech Generating Device Software – Programs used on a laptop computer, desktop computer, tablet, cell phone,
or personal digital assistant (PDA) that enable the user to improve their communication to a functional level
Stadium Style Seat – A one or two piece stadium style seat with rigid frame and cushioning material in both seat and
back sections, covered in cloth, vinyl, leather or equal as upholstery, and designed to serve as a complete seating,
support, and cushioning system for the user. It may have armrests that can be fixed, swing away, or detachable. It
will not have a headrest. Chairs with stadium style seats are billed using the Captain’s Chair codes
Standard Components – are those components that are not made solely for one individual. They are prefabricated
and readily available on the commercial market (off the shelf) and can be utilized by a variety of patients
Test Standards – Performance and durability acceptance criteria defined by ANSI/RESNA standard testing protocols
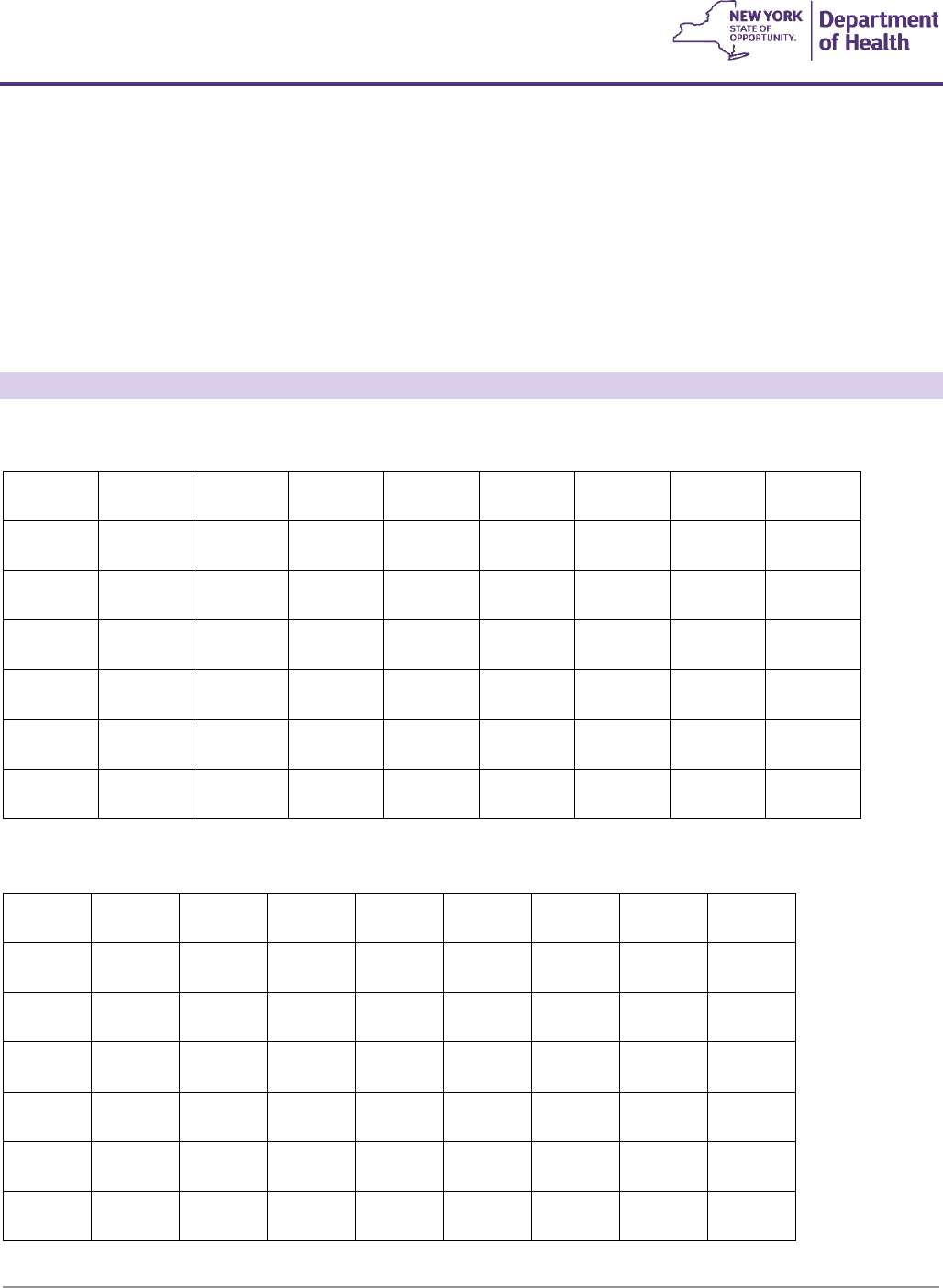
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
141
Top End Speed - Minimum speed acceptable for a given category of devices. It is to be determined by the RESNA
test for maximum speed on a flat hard surface
Upper Extremity Support System/Wheelchair tray – A flat surface across the abdominal area attached to a
wheelchair at the armrests used to support proper positioning of upper extremities. Padded foam or foam like
additions (i.e., protraction blocks, padding added to the flat surface) to a UESS are used to place the upper
extremities in a protracted position to address strong spasticity or exaggerated muscle activity
Appendix A
E2603
F5
#Skin protection wheelchair seat cushion, width less than 22 inches, any depth
(a)
L89.130
L89.131
L89.132
L89.133
L89.134
L89.139
L89.140
L89.141
L89.142
L89.143
L89.144
L89.149
L89.150
L89.151
L89.152
L89.153
L89.154
L89.159
L89.40
L89.41
L89.42
L89.43
L89.44
L89.45
L89.200
L89.201
L89.202
L89.203
L89.204
L89.209
L89.210
L89.211
L89.212
L89.213
L89.214
L89.219
L89.220
L89.221
L89.222
L89.223
L89.224
L89.229
L89.300
L89.301
L89.302
L89.303
L89.304
L89.309
L89.310
L89.311
L89.312
L89.313
L89.314
L89.319
L89.320
L89.321
L89.322
L89.323
L89.324
L89.329
E2603
F5
#Skin protection wheelchair seat cushion, width less than 22 inches, any depth
(b)
G82.50
G82.51
G82.52
G82.53
G82.54
G82.50
G04.1
G82.20
G82.21
G82.22
G95.0
G95.11
G95.19
G32.0
G99.2
G35
G36.0
G37.0
G37.5
G37.3
G36.1
G36.8
G37.1
G37.2
G37.4
G37.8
G36.9
G37.9
G80.1
G80.2
G80.0
G80.8
G80.4
G80.9
G12.0
G12.9
G12.1
G12.8
G12.21
G12.29
G12.20
G80.8
B91
G14
Q05.4
Q05.9
Q07.01
Q07.02
Q07.03
Q05.0
Q05.1
Q05.2
Q05.3
Q05.8
Q07.00
Q05.5
Q05.6
Q05.7
E75.23
E75.25
E75.29
E75.00
E75.01
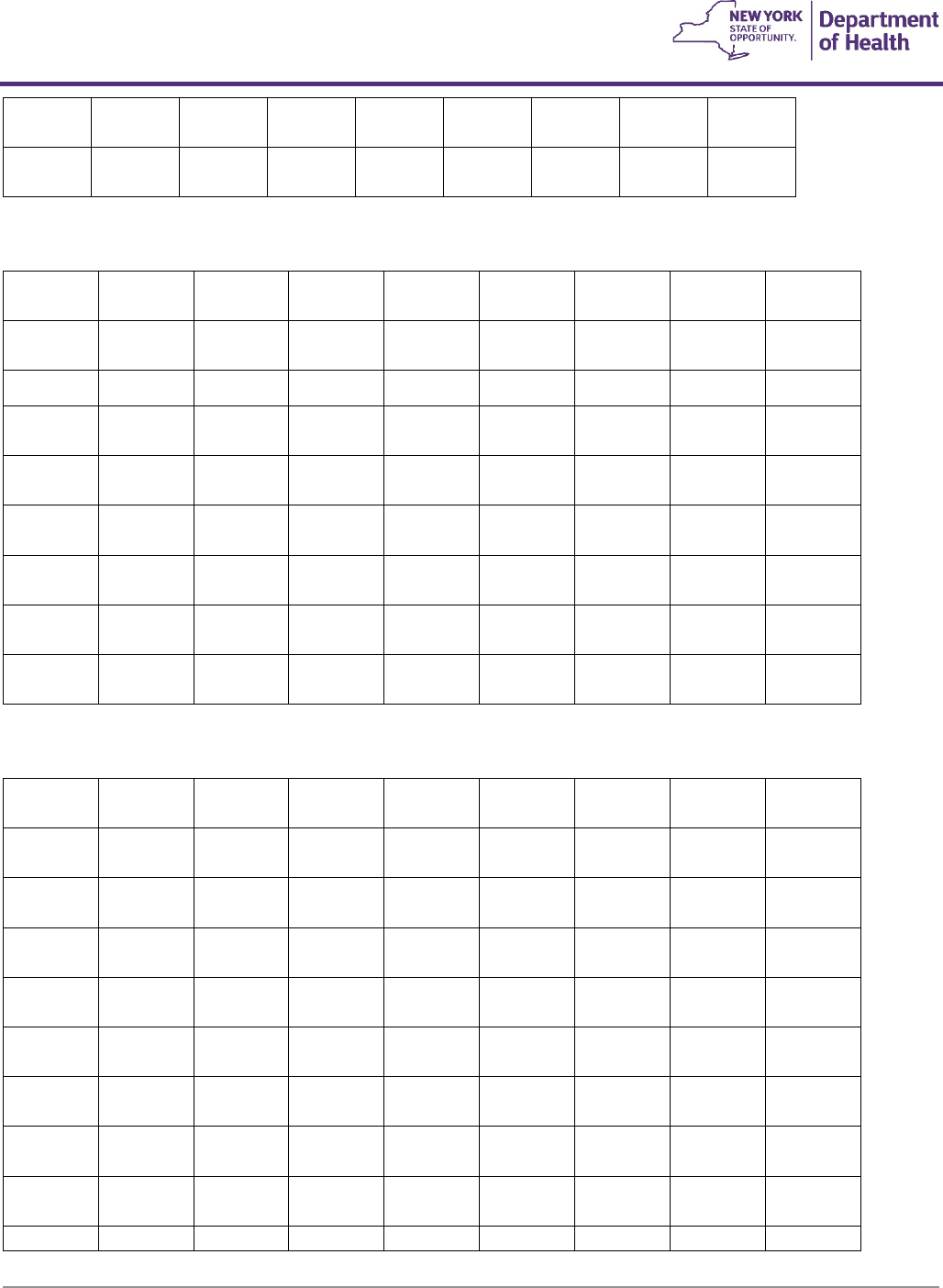
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
142
E75.02
E75.09
E75.10
E75.11
E75.19
E75.4
G93.89
G93.9
F84.2
G31.81
G31.82
G31.9
G30.0
G30.1
G30.8
G30.9
G20
G21.4
E2603
F5
#Skin protection wheelchair seat cushion, width less than 22 inches, any depth
(c)
G82.50
G82.51
G82.52
G82.53
G82.54
G82.50
G04.1
G82.20
G82.21
G82.22
G95.0
G95.11
G95.19
G32.0
G99.2
G35
G36.0
G37.0
G37.5
G37.3
G36.1
G36.8
G37.1
G37.2
G37.4
G37.8
G36.9
G37.9
G80.1
G80.2
G80.0
G80.8
G80.4
G80.9
G12.0
G12.9
G12.1
G12.8
G12.21
G12.29
G12.20
B91
G14
Q05.4
Q05.9
Q07.01
Q07.02
Q07.03
Q05.0
Q05.1
Q05.2
Q05.3
Q05.8
Q05.9
Q07.00
Q05.5
Q05.6
Q05.7
E75.23
E75.25
E75.29
E75.00
E75.01
E75.02
E75.09
E75.10
E75.11
E75.19
E75.4
G93.89
G93.9
F84.2
G31.8
G31.82
G31.9
G30.0
G30.1
G30.8
G30.9
G20
G21.4
E2605
F5
#Positioning wheelchair seat cushion, width less than 22 inches, any depth
(b)
G83.10
G83.11
G83.12
G83.13
G83.14
I69.049
I69.149
I69.249
I69.349
I69.849
I69.949
I69.041
I69.042
I69.141
I69.142
I69.241
I69.242
I69.341
I69.342
I69.841
I69.842
I69.941
I69.942
I69.043
I69.044
I69.143
I69.144
I69.243
I69.244
I69.343
I69.344
I69.843
I69.844
I69.943
I69.944
G81.00
G81.01
G81.02
G81.03
G81.04
G81.10
G81.11
G81.12
G81.13
G81.14
G81.90
G81.91
G81.92
G81.93
G81.94
I69.059
I69.159
I69.259
I69.359
I69.859
I69.959
I69.051
I69.052
I69.151
I69.152
I69.251
I69.252
I69.351
I69.352
I69.851
I69.852
I69.951
I69.952
I69.053
I69.054
I69.153
I69.154
I69.253
I69.254
I69.353
I69.354
I69.853
I69.854
I69.953
I69.954
G71.2
G71.0
G10
G24.1
G11.1
G11.4
G11.0
G11.2
G32.81
G11.3
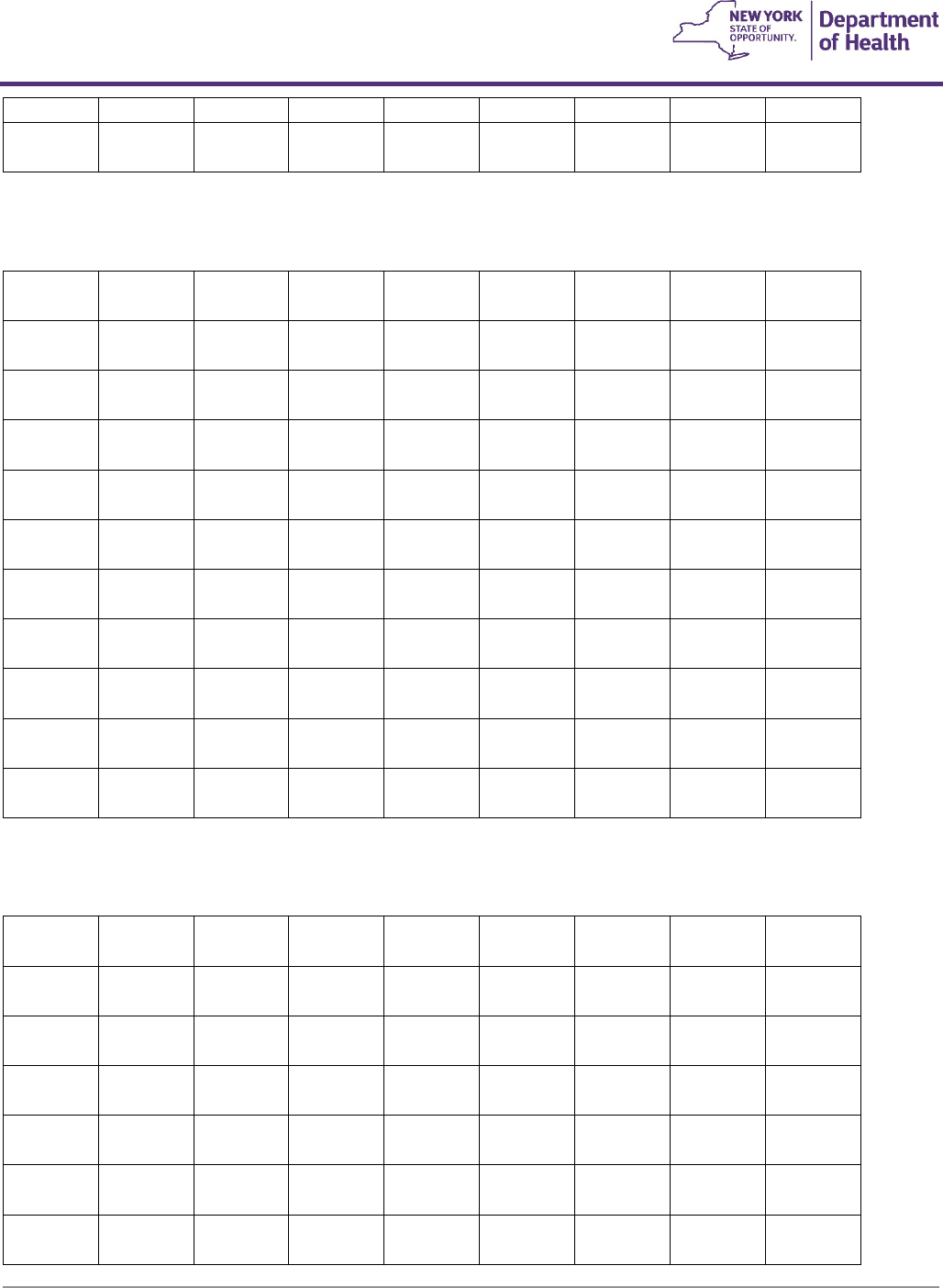
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
143
G11.8
G11.9
E2613
F5
#Positioning wheelchair back cushion, posterior, width less than 22 inches, any height,
including any type mounting hardware
(b)
G83.10
G83.11
G83.12
G83.13
G83.14
I69.049
I69.149
I69.249
I69.349
I69.849
I69.949
I69.041
I69.042
I69.141
I69.142
I69.241
I69.242
I69.341
I69.342
I69.841
I69.842
I69.941
I69.942
I69.043
I69.044
I69.143
I69.144
I69.243
I69.244
I69.343
I69.344
I69.843
I69.844
I69.943
I69.944
G81.00
G81.01
G81.02
G81.03
G81.04
G81.10
G81.11
G81.12
G81.13
G81.14
G81.90
G81.91
G81.92
G81.93
G81.94
I69.059
I69.159
I69.259
I69.359
I69.859
I69.959
I69.051
I69.052
I69.151
I69.152
I69.251
I69.252
I69.351
I69.352
I69.851
I69.852
I69.951
I69.952
I69.053
I69.054
I69.153
I69.154
I69.253
I69.254
I69.353
I69.354
I69.853
I69.854
I69.953
I69.954
G71.2
G71.0
G10
G24.1
G11.1
G11.4
G11.0
G11.2
G32.81
G11.3
G11.8
G11.9
E2615
F5
#Positioning wheelchair back cushion, posterior-lateral, width less than 22 inches, any
height, including any type mounting hardware
(b)
G83.10
G83.11
G83.12
G83.13
G83.14
I69.049
I69.149
I69.249
I69.349
I69.849
I69.949
I69.041
I69.042
I69.141
I69.142
I69.241
I69.242
I69.341
I69.342
I69.841
I69.842
I69.941
I69.942
I69.043
I69.044
I69.143
I69.144
I69.243
I69.244
I69.343
I69.344
I69.843
I69.844
I69.943
I69.944
G81.00
G81.01
G81.02
G81.03
G81.04
G81.10
G81.11
G81.12
G81.13
G81.14
G81.90
G81.91
G81.92
G81.93
G81.94
I69.059
I69.159
I69.259
I69.359
I69.859
I69.959
I69.051
I69.052
I69.151
I69.152
I69.251
I69.252
I69.351
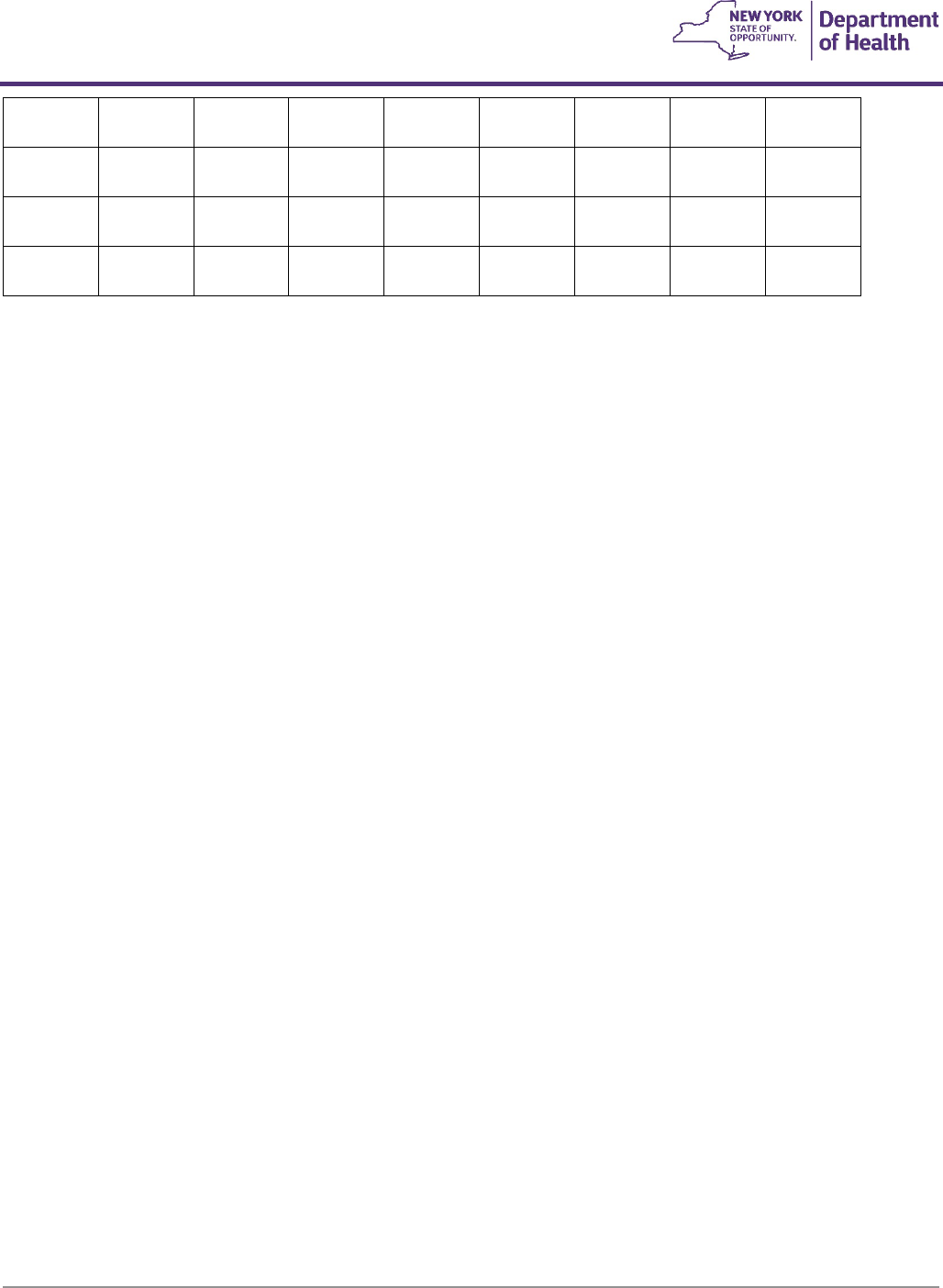
Coverage Guidelines
Durable Medical Equipment, Prosthetics, and Orthotics
Coverage Guidelines
DME Procedure Codes & Coverage Guidelines |
144
I69.352
I69.851
I69.852
I69.951
I69.952
I69.053
I69.054
I69.153
I69.154
I69.253
I69.254
I69.353
I69.354
I69.853
I69.854
I69.953
I69.954
G71.2
G71.0
G10
G24.1
G11.1
G11.4
G11.0
G11.2
G32.81
G11.3
G11.8
G11.9
