
Washington Apple Health (Medicaid)
Respiratory Care
Billing Guide
January 1, 2019
Every effort has been made to ensure this guide’s accuracy. If an actual or apparent conflict between this
document and an agency rule arises, the agency rules apply.
About this guide
∗
This publication takes effect January 1, 2019, and supersedes earlier guides to this program.
The Health Care Authority (agency) is committed to providing equal access to our services. If
you need an accommodation or require documents in another format, please call 1-800-562-
3022. People who have hearing or speech disabilities, please call 711 for relay services.
Washington Apple Health means the public health insurance programs for eligible
Washington residents. Washington Apple Health is the name used in Washington
State for Medicaid, the children's health insurance program (CHIP), and state-
only funded health care programs. Washington Apple Health is administered by
the Washington State Health Care Authority.
Refer also to the agency’s ProviderOne billing and resource guide for valuable information to
help you conduct business with the agency.
∗
This publication is a billing instruction.
Respiratory Care
3
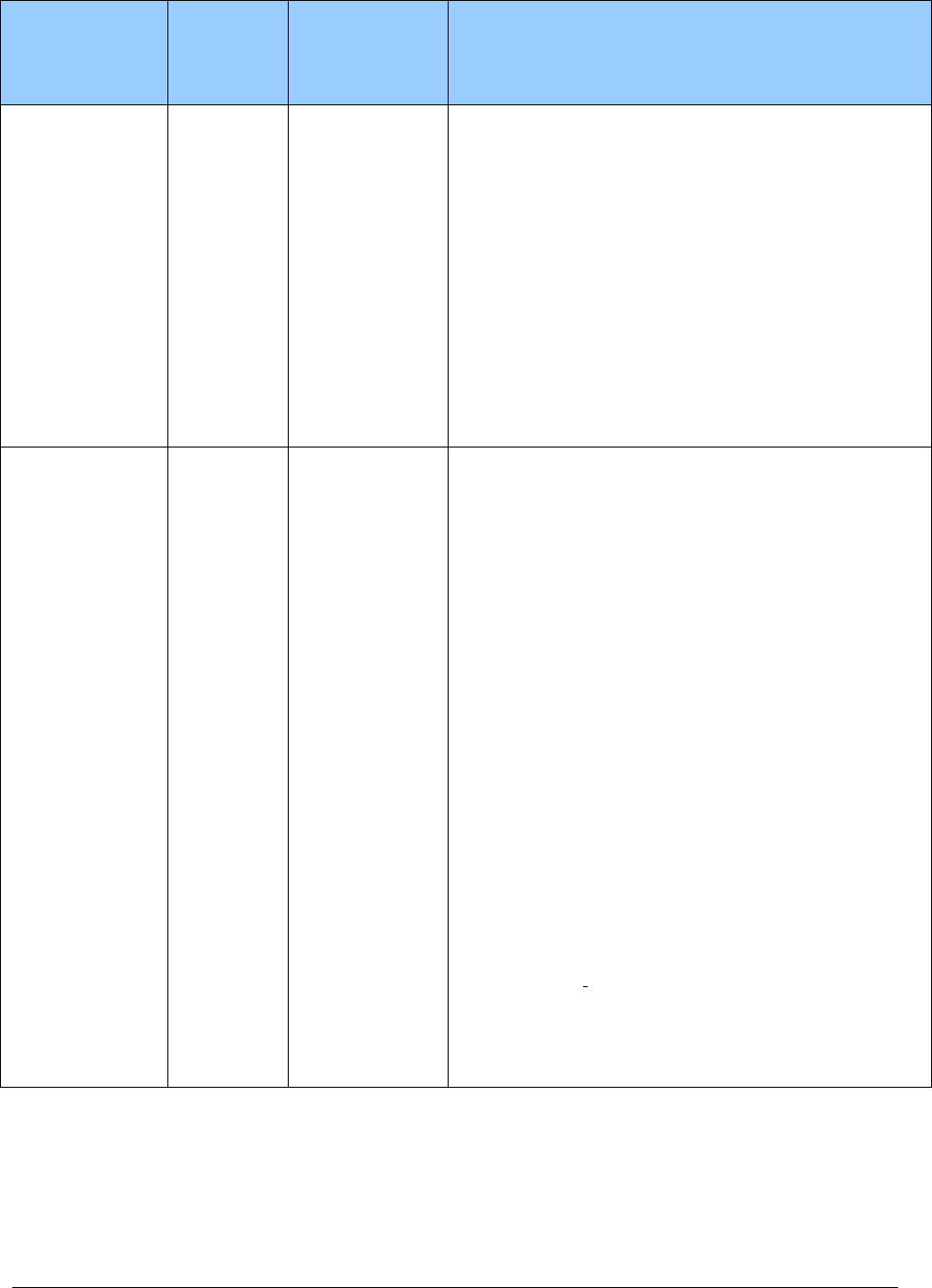
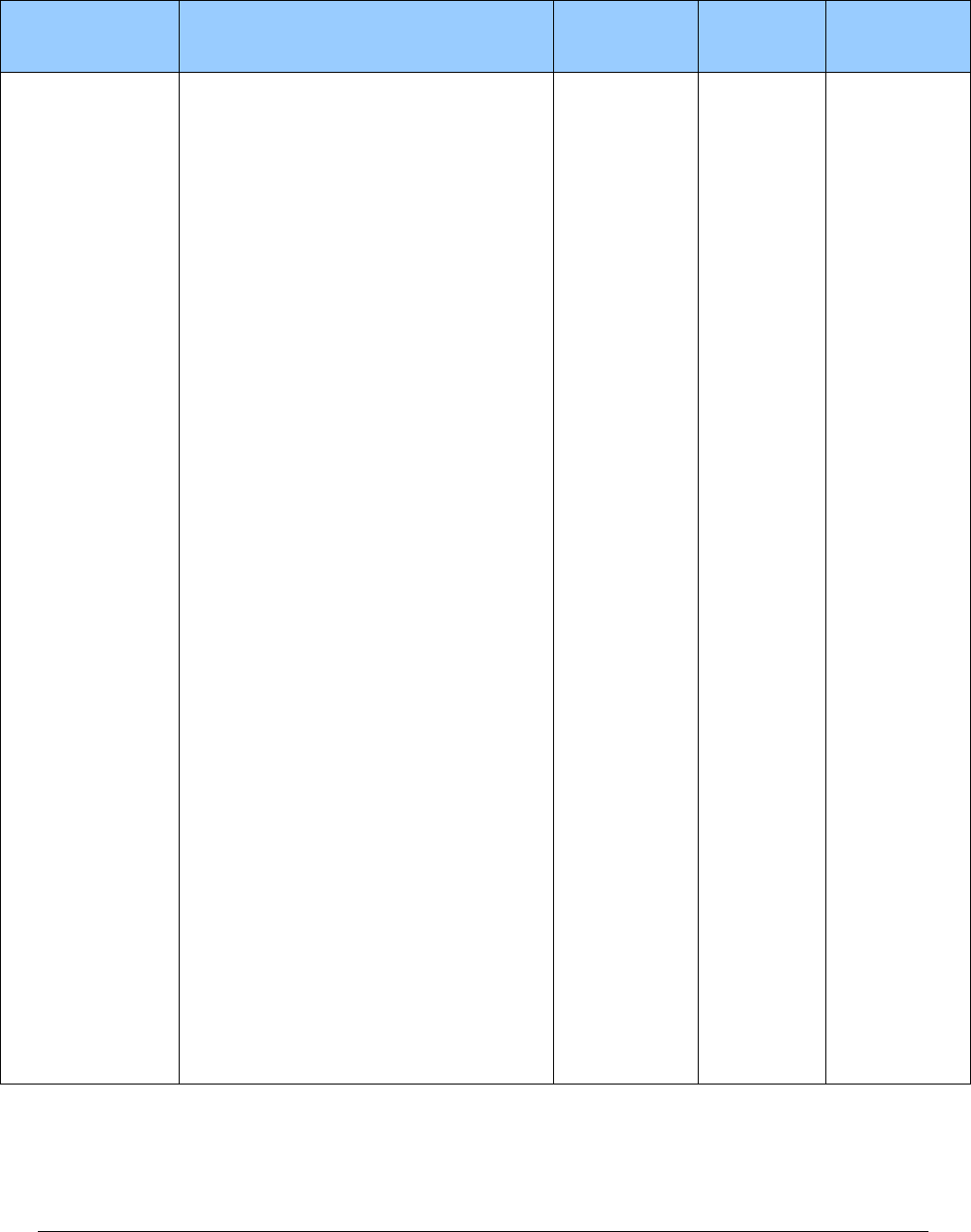
What has changed?
Subject
Change
Reason for Change
Entire document
General housekeeping
To improve clarity
Client Eligibility:
BHO, Changes for
January 1, 2019, IMC,
and Integrated Apple
Health Foster Care
Effective January 1, 2019, some existing
integrated managed care regions have new
counties
, and many new regions and
counties will be implemented.
Apple Health managed
care organizations
(MCOs) in certain RSAs
will expand their coverage
of behavioral health
services (mental health
and substance use disorder
treatment), along with
continuing to cover
physical health services.
Face-to-face encounter
examinations
Added a new section on face-to-face
encounter examinations
To comply with CMS
requirements
Oximeters
Reorganized section
To improve clarity
Modifier for
tracheostomy HCPCS
code
For HCPCS code A7520, removed
modifier AU and the sentence, “Invoice
required when billing with modifier AU.”
To list the correct modifier
Modifiers for
miscellaneous HCPCS
codes
Changed modifiers for HCPCS codes
A4450 and A4452 to AU
To list the correct modifier
How can I get agency provider documents?
To access provider alerts, go to the agency’s provider alerts web page.
To access provider documents, go to the agency’s provider billing guides and fee schedules web
page.
Respiratory Care
4
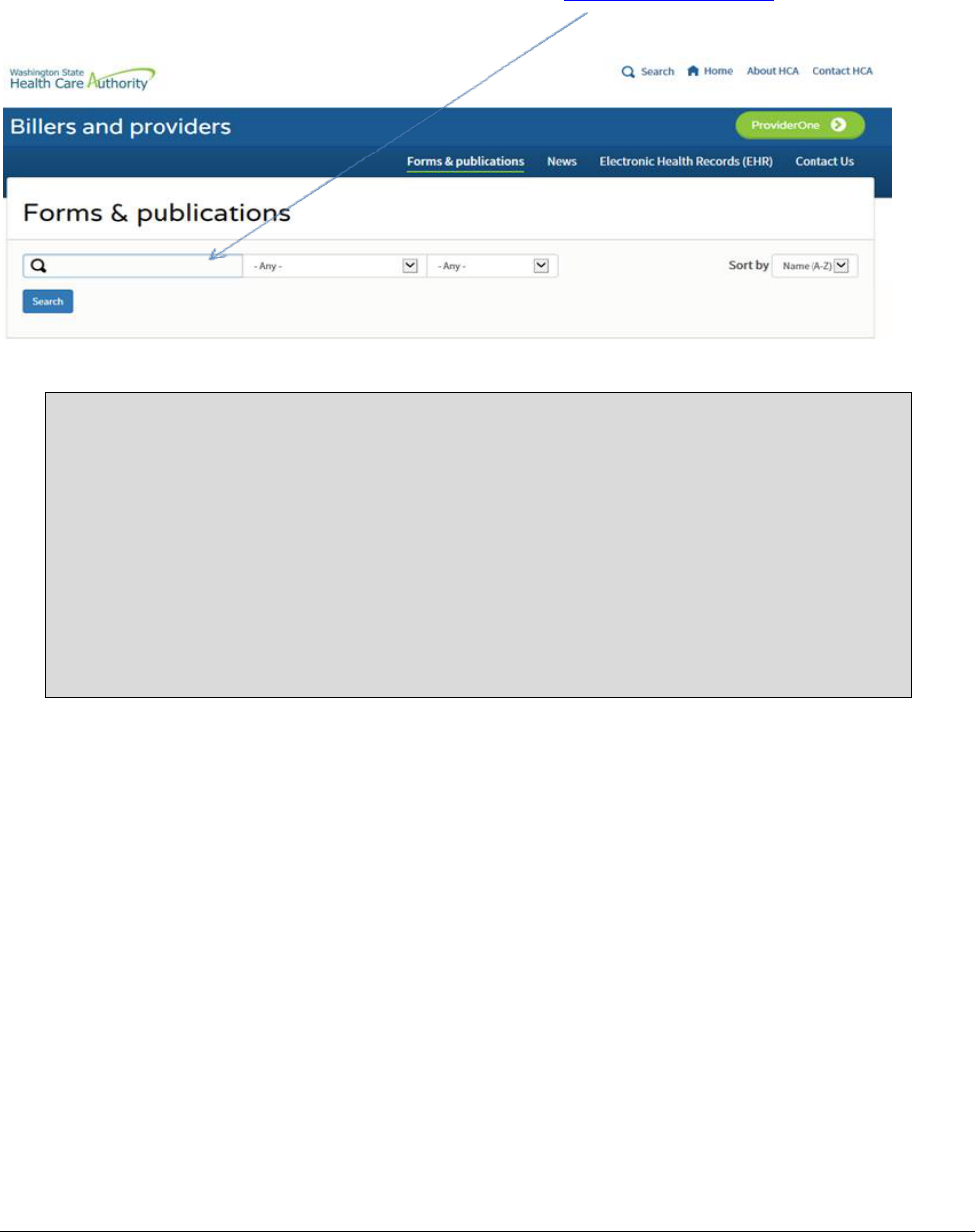
Where can I download agency forms?
To download an agency provider form, go to the agency’s Forms & publications webpage. Type
the agency form number into the Search box as shown below (Example: 13-835).
Copyright disclosure
Current Procedural Terminology (CPT) copyright 2018 American Medical Association
(AMA). All rights reserved. CPT is a registered trademark of the AMA.
Fee schedules, relative value units, conversion factors and/or related components are
not assigned by the AMA, are not part of CPT, and the AMA is not recommending
their use. The AMA does not directly or indirectly practice medicine or dispense
medical services. The AMA assumes no liability for data contained or not contained
herein.

Respiratory Care
Alert! This Table of Contents is automated. Click on a page number to go directly to the page.
5
Table of Contents
How can I get agency provider documents? ..............................................................................3
Where can I download agency forms? .......................................................................................4
Resources Available .......................................................................................................................8
Definitions .......................................................................................................................................9
About the Program ......................................................................................................................13
What is the purpose of the Respiratory Care program? ...........................................................13
When does the agency pay for respiratory care? .....................................................................13
Client Eligibility ...........................................................................................................................14
How do I verify a client’s eligibility? ......................................................................................14
Are clients enrolled in and agency-contracted managed care organization eligible? ..............15
Managed care enrollment ...................................................................................................16
Behavioral Health Organization (BHO) ............................................................................16
Apple Health – Changes for January 1, 2019 ....................................................................17
Integrated managed care ....................................................................................................17
Integrated managed care regions .......................................................................................18
Integrated Apple Health Foster Care (AHFC) ...................................................................19
Fee-for-service Apple Health Foster Care .........................................................................19
Provider Requirements ...............................................................................................................20
What are the general responsibilities of a respiratory care provider? ......................................20
Licensed health care professionals .....................................................................................20
Physician cosigning on face-to-face visits .........................................................................20
Are providers responsible to verify a client’s coverage? .........................................................21
Prescriptions .......................................................................................................................21
Respiratory care equipment and supplies ..........................................................................22
What are the client’s rights to health care decisions? ..............................................................23
Coverage .......................................................................................................................................24
What are the coverage criteria for respiratory care services? ..................................................24
What types of airway clearance devices does the agency cover? ............................................24
Does the agency cover the rental of apnea monitors? ..............................................................25
Does the agency cover bi-level respiratory assist devices (RADs)?........................................26
Clinical criteria...................................................................................................................26
Required clinical criteria for using RADs with specific types of respiratory
disorders .......................................................................................................................28
Replacement of bi-level RAD equipment and supplies .....................................................32
Does the agency cover continuous positive airway pressure (CPAP) and supplies? ..............33
Clinical criteria...................................................................................................................33
Use of RAD instead of CPAP ............................................................................................34
Prior authorization for a CPAP device...............................................................................34

Respiratory Care
Alert! This Table of Contents is automated. Click on a page number to go directly to the page.
6
Rental and purchase of a CPAP device..............................................................................35
Replacement of CPAP equipment and supplies.................................................................35
Does the agency cover nebulizers and related compressors? ..................................................36
Does the agency cover oximeters? ...........................................................................................37
For clients age 17 and younger ..........................................................................................37
For clients age 18 and older ...............................................................................................37
Does the agency cover oxygen? ...............................................................................................37
Requirements for valid oxygen prescriptions ....................................................................38
Coverage criteria for oxygen .............................................................................................39
Renting capped-rental oxygen systems and contents.........................................................40
Stationary and portable oxygen systems and contents .......................................................42
What types of services, equipment, and supplies does the agency not pay for? ......................44
Does the agency cover suction pumps and supplies? ..............................................................45
Does the agency cover ventilator equipment and supplies? ....................................................45
Primary ventilator ..............................................................................................................45
Secondary (back-up) ventilators ........................................................................................46
Expedited Prior Authorization ...........................................................................................46
Coverage Table.............................................................................................................................47
Apnea monitor and supplies...............................................................................................48
Continuous positive airway pressure system (CPAP) .......................................................49
IPPB machine and accessories ...........................................................................................54
Nebulizers and accessories ................................................................................................54
Oxygen and oxygen equipment .........................................................................................59
Suction pump/supplies .......................................................................................................72
Tracheostomy care supplies ...............................................................................................73
Ventilators and related respiratory equipment ...................................................................78
Miscellaneous ....................................................................................................................81
Miscellaneous equipment reimbursement..........................................................................87
Authorization................................................................................................................................89
What is prior authorization (PA)? ............................................................................................90
What are the criteria for PA? ...................................................................................................90
What is the PA process? ..........................................................................................................91
Online direct data entry into Provider One ........................................................................91
Written requests .................................................................................................................91
Additional information required for PA ............................................................................91
Is PA required for repairs to client-owned equipment? ...........................................................92
What is expedited prior authorization (EPA)? .........................................................................92
What are the EPA criteria? ......................................................................................................93
What is the EPA process? ........................................................................................................93
What is a limitation extension (LE)? .......................................................................................93
What are the LE criteria? .........................................................................................................94
What is the LE process? ...........................................................................................................94
Online direct data entry into Provider One ........................................................................94
Written requests .................................................................................................................94

Respiratory Care
Alert! This Table of Contents is automated. Click on a page number to go directly to the page.
7
Expedited prior authorization (EPA) criteria table ............................................................95
Noncovered Services ....................................................................................................................97
What types of services are not covered by the agency?...........................................................97
Reimbursement ............................................................................................................................98
What is the general payment for respiratory care? ..................................................................98
Maximum allowable fees ...................................................................................................98
Reimbursement rates ..........................................................................................................99
What does the agency not pay for? ..........................................................................................99
How does the agency decide to rent or purchase equipment? ...............................................100
What does the agency pay when replacement of rental equipment and supplies is
needed? ............................................................................................................................101
What rental equipment does the agency not pay for? ............................................................102
Does the agency pay for only new equipment? .....................................................................102
When does the agency pay for new equipment on capped-rental items? ..............................103
When does the agency pay for repairs on client-owned equipment? .....................................103
Does the agency require PA for repairs of client-owned equipment? ...................................104
What payment methodology does the agency use for the purchase of respiratory care
equipment? .......................................................................................................................105
How does the agency establish monthly rental reimbursement rates for respiratory
care equipment? ...............................................................................................................106
How does the agency establish daily rental payment rates for respiratory care
equipment? .......................................................................................................................106
Where is the program fee schedule? ......................................................................................106
Billing ..........................................................................................................................................107
What are the general billing requirements? ...........................................................................107
Billing with authorization numbers .................................................................................107
Is information available to bill for clients eligible for both Medicare and Medicaid? ..........107
How does the agency handle third-party liability coverage? .................................................108
How do I bill claims electronically? ......................................................................................108
How does a provider bill for supplies? ..................................................................................109
Respiratory Care
8
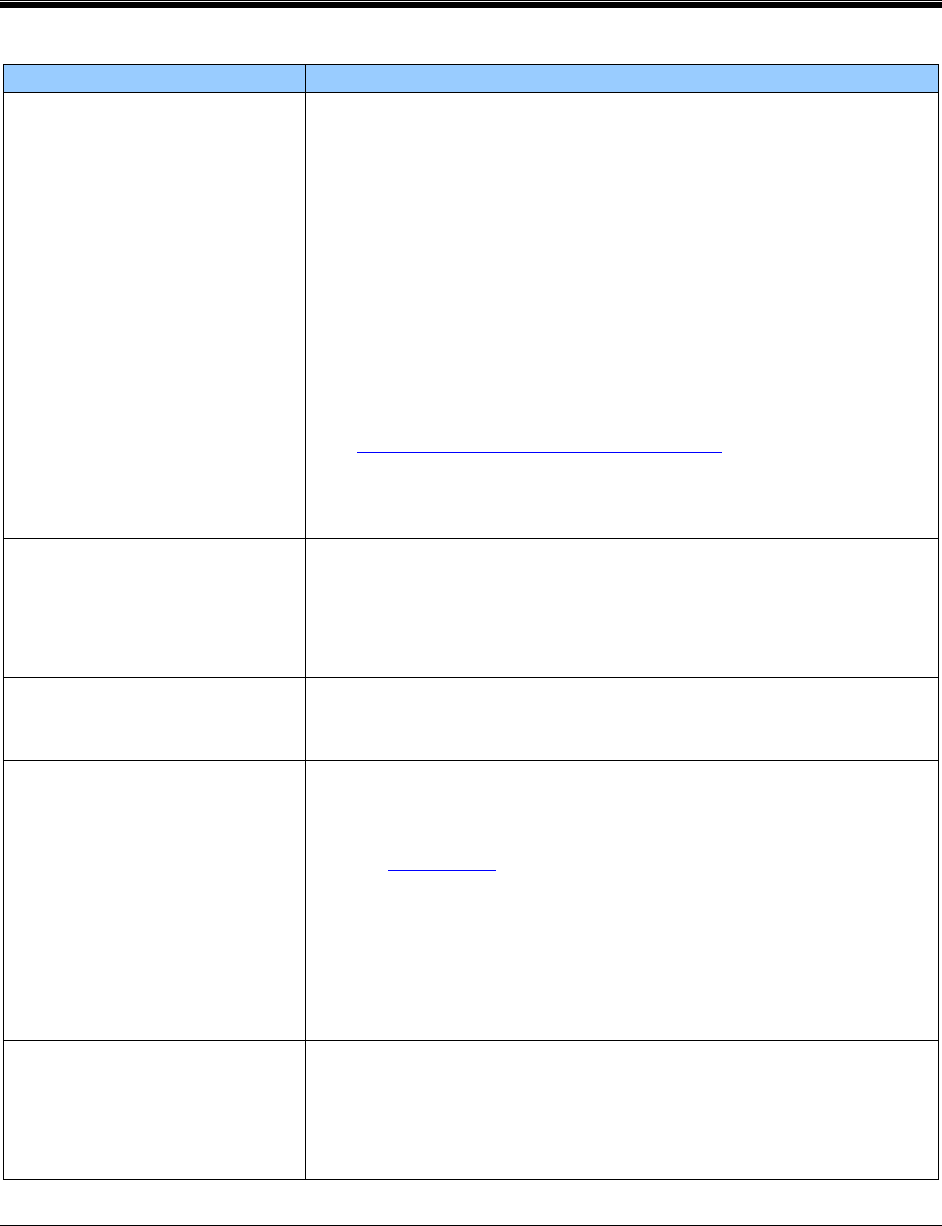
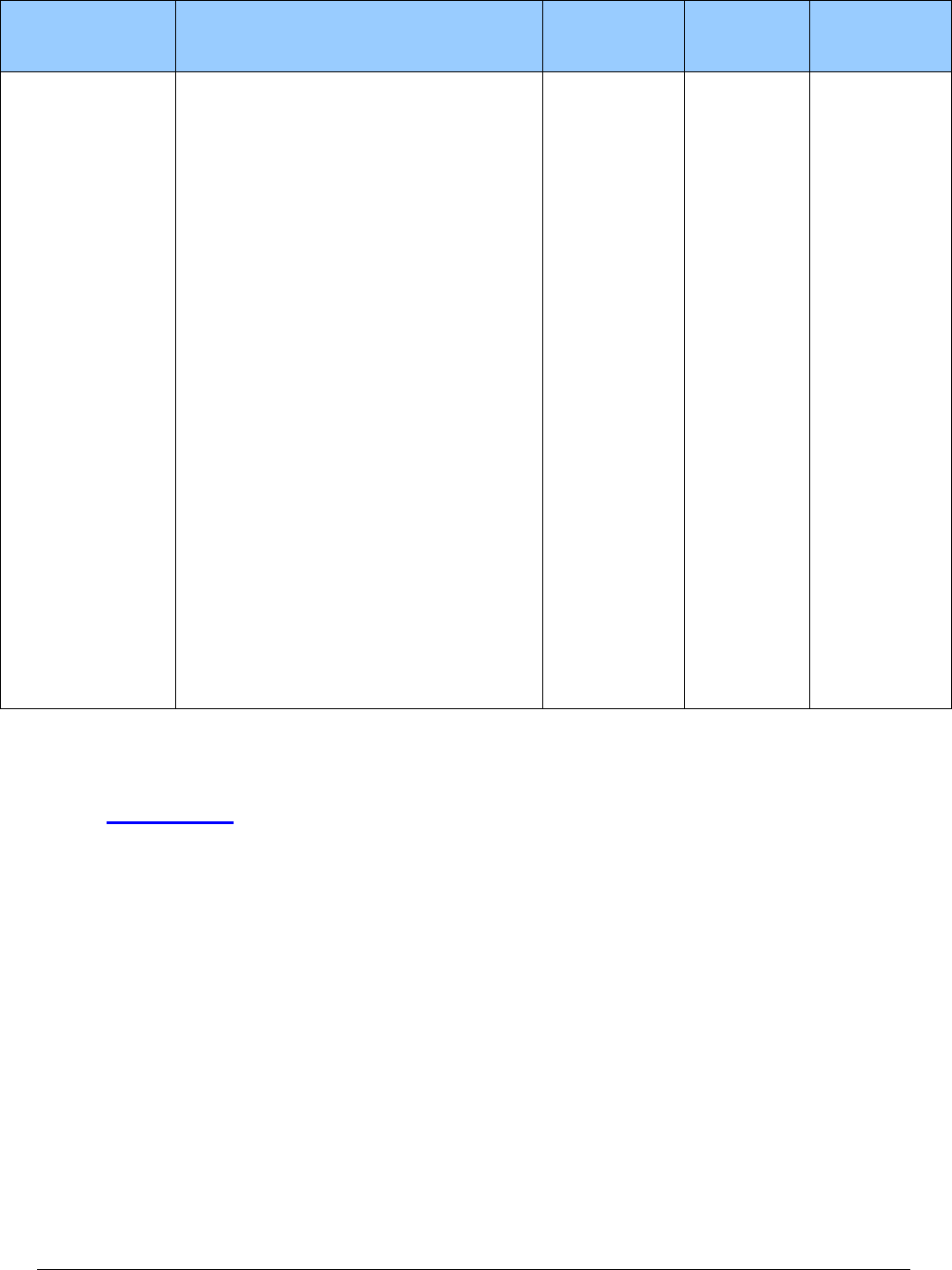
Resources Available
Topic
Contact Information
How do I obtain prior
authorization or a limitation
extension?
For all requests for prior authorization or limitation extensions,
both these forms are required:
• A completed, TYPED General Information for
Authorization form, HCA 13-835. This request form
must be the initial page when you submit your request.
• A completed Oxygen and Respiratory Authorization
Request form, HCA 15-298, and all the documentation
listed on this form and any other medical justification.
See Where can I download agency forms?
Fax your request to: 866-668-1214.
How do I check on the status
of a request for prior
authorization or limitation
extension?
• Call 800-562-3022 and select the topic
• Call 800-562-3022, extension 15471
How do I get answers for
billing questions?
Call 800-562-3022 and ask for the billing extension.
How do I obtain information
regarding the Respiratory
Care Program?
Do one of the following:
• Refer to the agency’s Billers and Providers,
Contact Us web page
• Contact the Respiratory Care program manager at:
Division of Health Care Services
Health Care Authority
PO Box 45506
Olympia, WA 98504-5506
Who do I contact if I have a
reimbursement question?
Cost Reimbursement Analyst
Professional Reimbursement
PO Box 45510
Olympia, WA 98504-5510
Respiratory Care
9
Definitions
This section defines terms and abbreviations, including acronyms, used in this billing guide.
Refer to Chapter 182-500 WAC for a complete list of definitions for Washington Apple Health.
Adult Family Home – A residential home
licensed to care for up to six residents that
provides rooms, meals, laundry, supervision,
assistance with activities of daily living, and
personal care. In addition to these services,
some homes provide nursing or other special
care and services. (WAC 182-552-0005)
Apnea – The cessation of airflow for at least
10 seconds. (WAC 182-552-0005)
Apnea-hypopnea index (AHI) –
The average number of episodes of apnea
and hypopnea per hour of sleep without the
use of a positive airway pressure device. For
purposes of this chapter, respiratory effort
related arousals (RERAs) are not included in
the calculation.
Arterial PaO2 – Measurement of partial
pressure of arterial oxygen.
(WAC 182-552-0005)
Authorized prescriber – A health care
practitioner authorized by law or rule in the
state of Washington to prescribe oxygen and
respiratory care equipment, supplies, and
services. (WAC 182-552-0005)
Bi-level respiratory assist device (RAD)
with backup rate – A device that allows
independent setting of inspiratory and
expiratory pressures to deliver positive airway
pressure (within a single respiratory cycle) by
way of tubing and a noninvasive interface
(such as a nasal or oral facial mask) to assist
spontaneous respiratory efforts and
supplement the volume of inspired air into the
lungs. In addition, these devices have a timed
backup feature to deliver this air pressure
whenever sufficient spontaneous inspiratory
efforts fail to occur. (WAC 182-552-0005)
Bi-level respiratory assist device (RAD)
without backup rate– A device that allows
independent setting of inspiratory and
expiratory pressures to deliver positive airway
pressure (within a single respiratory cycle) by
way of tubing and a noninvasive interface
(such as a nasal, oral, or facial mask) to assist
spontaneous respiratory efforts and
supplement the volume of inspired air into the
lungs. (WAC 182-552-0005)
Blood gas study – For this guide, either an
oximetry test or an arterial blood gas test.
(WAC 182-552-0005)
Boarding Home – Adult residential care
(ARC) facility, enhanced adult residential
care (EARC) facility, or assisted living (AL)
facility. (WAC 182-552-0005)
Capped rental – Applies to certain oxygen
equipment for in-home medical assistance
clients. After 36 months of rental by the
provider, the equipment is considered
capped (not reimbursed) for the next 24
months. (See When does the agency pay for
new equipment on capped-rental items?
Respiratory Care
10
Central sleep apnea (CSA) – Is defined as
meeting all the following criteria:
• An apnea-hypopnea index (AHI) greater
than or equal to 5.
• Central apneas/hypopneas greater than
50% of the total apneas/hypopneas.
• Central apneas or hypopneas greater
than or equal to 5 times per hour.
• Symptoms of either excessive sleepiness
or disrupted sleep.
(WAC 182-552-0005)
Chronic Obstructive Pulmonary Disease
(COPD) – Any disorder that persistently
obstructs bronchial airflow. COPD mainly
involves two related diseases—chronic
bronchitis and emphysema. Both cause
chronic obstruction of air flowing through
the airways and in and out of the lungs. The
obstruction is generally permanent and
worsens over time. (WAC 182-552-0005)
Complex Sleep Apnea (CompSA) – A
form of central apnea specifically identified
by the persistence or emergence of central
apneas or hypopneas, upon exposure to
CPAP or a bi-level respiratory assist device
without a back-up rate feature, when
obstructive events have disappeared. These
clients have predominantly obstructive or
mixed apneas during the diagnostic sleep
study occurring at greater than or equal to
five times per hour. With use of a CPAP or
bi-level respiratory assist device without a
back-up rate feature, the client shows a
pattern of apneas and hypopneas that meets
the definition of central sleep apnea (CSA).
(WAC 182-552-0005)
Compressor – A pump driven appliance
that mechanically condenses atmospheric air
into a smaller volume under pressure. In
respiratory care therapy, it is used to
forcefully nebulize liquid solutions or
emulsions into a vapor state, or mist for
inhalation.
Concentrator – A device that increases the
concentration of oxygen from the air.
Continuous Positive Airway Pressure
(CPAP) – A single-level device that delivers
a constant level of positive air pressure
(within a single respiratory cycle) by way of
tubing and an interface to assist spontaneous
respiratory efforts and supplement the
volume of inspired air into the lungs.
(WAC 182-552-0005)
Dependent Edema – Fluid in the tissues,
usually ankles, wrists, and the arms.
(WAC 182-552-0005)
Emergency Oxygen – The immediate,
short-term administration of oxygen to a
client who normally does not receive
oxygen, but is experiencing an acute episode
that requires oxygen. (WAC 182-552-0005)
Erythrocythemia – More hematocrit (red
blood cells) than normal, making it very
difficult to oxygenate those cells.
(WAC 182-552-0005)
FIO2 – The fractional concentration of
oxygen delivered to the client for
inspiration. For the purpose of this policy,
the client’s prescribed FIO2 refers to the
oxygen concentration the client normally
breathes when not undergoing testing to
qualify for coverage of a Respiratory Assist
Device (RAD). That is, if the client does not
normally use supplemental oxygen, their
prescribed FIO2 is that found in room air.
(WAC 182-552-0005)
FEV1 – The forced expired volume in 1
second. (WAC 182-552-0005)
Respiratory Care
11
FVC – The forced vital capacity.
(WAC 182-552-0005)
Group I – Clinical criteria, set by Medicare,
to identify chronic oxygen clients with
obvious respiratory challenges as evidenced
by low oxygen saturation. (For specific
clinical criteria, see Coverage criteria for
oxygen.) (WAC 182-552-0005)
Group II – Clinical criteria, set by
Medicare, to identify borderline oxygen
clients. Their blood saturation levels seem to
be within the normal range, but additional
extenuating issues suggest a need for
oxygen. (For specific clinical criteria, see
Coverage criteria for oxygen.)
(WAC 182-552-0005)
Home and Community Residential
Settings – In-home, adult family home, or
boarding home. (WAC 182-552-0005)
Hypopnea – A temporary reduction of
airflow lasting at least ten seconds and
accompanied with a 30% reduction in
thoracoabdominal movement or airflow as
compared to baseline, and with at least a 4%
decrease in oxygen saturation. The AHI is
the average number of episodes of apnea
and hypopnea per hour of sleep without the
use of a positive airway pressure device.
(WAC 182-552-0005)
Hypoxemia – Less than normal level of
oxygen in the blood. (WAC 182-552-0005)
Month – For the purposes of this guide,
means 30 days, regardless of the number of
days in a specific calendar month.
(WAC 182-552-0005)
Nebulizer – A medical device that
administers drugs for inhalation therapy for
clients with respiratory conditions such as
asthma or emphysema.
(WAC 182-552-0005)
Obstructive sleep apnea (OSA) – This
syndrome refers to the interruption of
breathing during sleep, due to obstructive
tissue in the upper airway that collapses into
the air passage with respiration. This may
occur several hundred times a night and is
thought to cause many symptoms, such as
depression, irritability, sexual dysfunction,
learning and memory difficulties, and the
frequent complaint of excessive daytime
sleepiness. (WAC 182-552-0005)
Oxygen – Medical grade liquid oxygen or
compressed gas. (WAC 182-552-0005)
Oxygen Concentrator – A medical device
that removes nitrogen from room air and
retains almost pure oxygen (87–95%) for
delivery to a client. (WAC 182-552-0005)
Oxygen System – All equipment necessary
to provide oxygen to a client.
(WAC 182-552-0005)
Portable Oxygen System – A system that
allows the client to be independent of the
stationary system for several hours, thereby
providing mobility for the client.
(WAC 182-552-0005)
Pulmonary hypertension – High blood
pressure in the vessels that feed through the
lungs, causing the right side of the heart to
work harder to oxygenate blood.
(WAC 182-552-0005)
RAD – Respiratory assist device
Respiratory Care
12
Reasonable Useful Lifetime (RUL) –
Refers to the 36-month capped rental
oxygen equipment; the RUL is 5 years. The
RUL is not based on the chronological age
of the equipment. It starts on the initial date
of service and runs for 5 years from that
date. (WAC 182-552-0005)
Respiratory Care The care of a client with
respiratory needs and all related equipment,
oxygen, services and supplies.
(WAC 182-552-0005)
Respiratory Care Practitioner – A person
licensed by the Department of Health
according to chapter 18.89 RCW and
chapter 246-928 WAC as a respiratory
therapist (RT) or respiratory care
practitioner (RCP). (WAC 182-552-0005)
Respiratory Effort Related Arousals
(RERA) – These occur when there is a
sequence of breaths that lasts at least ten
seconds, characterized by increasing
respiratory effort or flattening of the nasal
pressure waveform, which lead to an arousal
from sleep. However, they do not meet the
criteria of an apnea or hypopnea. The degree
to which RERAs are associated with the
same sequelae as apneas and hypopneas is
unknown, although clients with only RERAs
can be symptomatic in terms of excessive
daytime sleepiness. (WAC 182-552-0005)
Restrictive Thoracic Disorders – This
refers to a variety of neuromuscular and
anatomical anomalies of the chest/rib cage
area that may result in hypoventilation,
particularly while the client sleeps at night.
Nocturnal hypoventilation is associated with
a host of health hazards and also can
significantly impact the quality of life for
these clients. The use of noninvasive
positive pressure respiratory assist devices
has been found helpful in reducing the
episodes of nocturnal hypoventilation and
the associated complications for a
significant number of those clients who are
able to use the device.
RUL – Also called Reasonable Useful
Lifetime.
Stationary Oxygen System – Equipment
designed to be used in one location,
generally for the purpose of continuous use
or frequent intermittent use.
(WAC 182-552-0005)
Ventilator – A device to provide breathing
assistance to clients with neuromuscular
diseases, thoracic restrictive diseases, or
chronic respiratory failure consequent to
chronic obstructive pulmonary disease. It
includes both positive and negative pressure
devices.
Respiratory Care
13
About the Program
(WAC 182-552-0001)
What is the purpose of the Respiratory Care
program?
The purpose of the Respiratory Care program is to provide medically necessary respiratory care
equipment, services, and supplies to eligible agency clients who are not enrolled in a managed
care plan and reside in:
• A home.
• A community residential setting.
• A skilled nursing facility.
When does the agency pay for respiratory care?
The agency pays for respiratory care when it is:
• Covered.
• Within the scope of the eligible client’s medical care program.
• Medically necessary, as defined under WAC 182-500-0070.
• Prescribed by a physician, advanced registered nurse practitioner (ARNP), or physician
assistant certified (PAC) within the scope of licensure.
• Authorized, as required within chapters 182-501, 182-502, and 182-552 WAC, and this
billing guide.
• Billed according to this billing guide.
• Provided and used within accepted medical or respiratory care community standards of
practice.
The respiratory care services, equipment, and supplies described in this guide are considered part
of the agency’s durable medical equipment (DME) benefit.
Respiratory Care
14
Client Eligibility
Most Apple Health clients are enrolled in an agency-contracted managed care organization
(MCO). This means that Apple Health pays a monthly premium to an MCO for providing
preventative, primary, specialty, and other health services to Apple Health clients. Clients in
managed care must see only providers who are in their MCO’s provider network, unless prior
authorized or to treat urgent or emergent care. See the agency’s Managed Care web page, under
Apple Health Managed Care for further details.
It is important to always check a client’s eligibility prior to
providing any services because it affects who will pay for the services.
How do I verify a client’s eligibility?
Check the client’s Services Card or follow the two-step process below to verify that a client has
Apple Health coverage for the date of service and that the client’s benefit package covers the
applicable service. This helps prevent delivering a service the agency will not pay for.
Is the client enrolled in an agency-contracted managed care organization (MCO), in a behavioral
health organization (BHO), or is the client receiving services through fee-for-service (FFS)
Apple Health?
Verifying eligibility is a two-step process:
Step 1. Verify the patient’s eligibility for Apple Health. For detailed instructions on
verifying a patient’s eligibility for Apple Health, see the Client Eligibility, Benefit
Packages, and Coverage Limits section in the agency’s ProviderOne billing and
resource guide.
If the patient is eligible for Apple Health, proceed to Step 2. If the patient is not
eligible, see the note box below.
Step 2. Verify service coverage under the Apple Health client’s benefit package. To
determine if the requested service is a covered benefit under the Apple Health client’s
benefit package, see the agency’s Program benefit packages and scope of services web
page.
Respiratory Care
15
Note: Patients who are not Apple Health clients may submit an application for
health care coverage in one of the following ways:
1. By visiting the Washington Healthplanfinder’s website at:
www.wahealthplanfinder.org
2. By calling the Customer Support Center toll-free at: 855-WAFINDER
(855-923-4633) or 855-627-9604 (TTY)
3. By mailing the application to:
Washington Healthplanfinder
PO Box 946
Olympia, WA 98507
In-person application assistance is also available. To get information about in-
person application assistance available in their area, people may visit
www.wahealthplanfinder.org or call the Customer Support Center.
Are clients enrolled in and agency-contracted
managed care organization eligible?
(WAC 182-552-0100 (2))
Yes. Respiratory care services, equipment and supplies are covered under the agency-contracted
managed care organization (MCO) when the services are medically necessary. All services must
be requested directly through the client’s MCO.
Providers can verify a client’s managed care enrollment through the ProviderOne client benefit
inquiry screen.
Clients may contact their MCO by calling the telephone number provided to them.
The MCO is responsible for:
• Payment of covered services.
• Payment of services referred by a provider participating with the plan to an outside
provider.
Respiratory Care
16
Managed care enrollment
Apple Health (Medicaid) places clients into an agency-contracted MCO the same month they are
determined eligible for managed care as a new or renewing client. This eliminates a person being
placed temporarily in FFS while they are waiting to be enrolled in an MCO or reconnected with
a prior MCO. This enrollment policy also applies to clients in FFS who have a change in the
program they are eligible for.
New clients are those initially applying for benefits or those with changes in their existing
eligibility program that consequently make them eligible for Apple Health managed care.
Renewing clients are those who have been enrolled with an MCO but have had a break in
enrollment and have subsequently renewed their eligibility.
Checking eligibility
• Providers must check eligibility and know when a client is enrolled and with which
MCO. For help with enrolling, clients can refer to the Washington Healthplanfinder’s Get
Help Enrolling page.
• MCOs have retroactive authorization and notification policies in place. The provider
must know the MCO’s requirements and be compliant with the MCO’s policies.
Behavioral Health Organization (BHO)
The Health Care Authority (agency) manages the contracts for behavioral health services (mental
health and substance use disorder) for the following four Regional Service Areas (RSAs):
• Great Rivers: Includes Cowlitz, Grays Harbor, Lewis, Pacific, and Wahkiakum counties
• North Sound: Includes Island, San Juan, Skagit, Snohomish, and Whatcom counties
• Salish: Includes Clallam, Jefferson, and Kitsap counties
• Thurston-Mason: Includes Thurston and Mason counties
To view a map and table of the integrated managed care plans available within each region,
please see Changes coming to Washington Apple Health. You may also refer to the agency’s
Apple Health managed care webpage.
See the agency’s Mental health services billing guide for details.
Respiratory Care
17
Apple Health – Changes for January 1, 2019
Effective January 1, 2019, agency-contracted managed care organizations (MCOs) in certain
Regional Services Areas (RSAs) will expand their coverage of behavioral health services (mental
health and substance use disorder treatment), along with continuing to cover physical health
services. The RSAs are outlined in the Integrated managed care regions section.
Apple Health clients who are not enrolled in an agency-contracted MCO for their physical health
services (e.g., dual-eligible Medicare-Medicaid clients) will still receive their behavioral health
services through one of the agency-contracted MCOs. The MCO will provide only behavioral
health services for the client.
Most clients will remain with the same health plan, except in regions where client’s plan will no
longer be available. The agency will auto-enroll these clients to one of the offered plans.
Clients can change their plan at any time by:
• Visiting the ProviderOne client portal.
• Calling Apple Health Customer Service toll-free at 1-800-562-3022. This automated
system is available 24 hours a day, 7 days a week.
• Requesting a change online through our secure Contact us – Apple Health (Medicaid)
client web form. Select the topic “Enroll/Change Health Plans.”
• Visiting the Washington Healthplanfinder (only for clients with a Washington
Healthplanfinder account).
Integrated managed care
For clients who live in an integrated managed care region, all physical health services, mental
health services, and drug and alcohol treatment are covered and coordinated by the client’s
agency-contracted MCO. The BHO will not provide behavioral health services in these regions.
Clients living in an integrated managed care region will enroll with an MCO of their choice that
is available in that region. If the client does not choose an MCO, the client will be automatically
enrolled into one of the available MCOs, unless the client is American Indian/Alaska Native
(AI/AN). Clients currently enrolled in one of the available MCOs in their region may keep their
enrollment when the behavioral health services are added.
Respiratory Care
18
American Indian/Alaska Native (AI/AN) clients living in an integrated
managed care region of Washington may choose to enroll in one of the agency-
contracted MCOs available in that region or they may choose to receive all these
services through Apple Health fee-for-service (FFS). If they do not choose an
MCO, they will be automatically enrolled into Apple Health FFS for all their
health care services, including comprehensive behavioral health services. See the
agency’s American Indian/Alaska Native webpage.
For more information about the services available under the FFS program, see the
agency’s Mental health services billing guide and the Substance use disorder
billing guide.
For full details on integrated managed care, see the agency’s Changes to Apple Health managed
care webpage.
Integrated managed care regions
Clients who reside in the following integrated managed care regions and who are eligible for
managed care enrollment must choose an available MCO in their region. Details, including
information about mental health crisis services, are located on the agency’s Apple Health
managed care webpage.
Existing integrated managed care regions – Expanding January 1, 2019
• North Central (Chelan, Douglas, Grant, and Okanogan counties)
The agency expanded this region to include Okanogan County
• Southwest Washington (Clark, Klickitat, and Skamania counties)
The agency expanded this region to include Klickitat County
New integrated managed care regions – Effective January 1, 2019
The following new regions are implemented for integrated managed care:
• Greater Columbia (Asotin, Benton, Columbia, Franklin, Garfield, Kittitas, Walla
Walla, Yakima, and Whitman counties)
• King (King County)
• Pierce (Pierce County)
• Spokane (Adams, Ferry, Lincoln, Pend Oreille, Spokane, and Stevens counties)
Respiratory Care
19
Integrated Apple Health Foster Care (AHFC)
Effective January 1, 2019, children and young adults in the Foster Care, Adoption Support and
Alumni programs who are enrolled in Coordinated Care of Washington’s (CCW) Apple Health
Foster Care program will receive both medical and behavioral health services from CCW.
Clients under this program are:
• Under the age of 21 who are in foster care (out of home placement).
• Under the age of 21 who are receiving adoption support.
• Age 18-21 years old in extended foster care.
• Age 18 to 26 years old who aged out of foster care on or after their 18
th
birthday (alumni).
These clients are identified in ProviderOne as
“Coordinated Care Healthy Options Foster Care.”
Fee-for-service Apple Health Foster Care
Children and young adults in the fee-for-service Apple Health Foster Care, Adoption Support and
Alumni programs receive behavioral health services through the regional Behavioral Health
Administrative Services Organization (BH-ASO). For details, see the agency’s Mental health
services billing guide, under How do providers identify the correct payer?
Respiratory Care
20
Provider Requirements
What are the general responsibilities of a
respiratory care provider?
(WAC 182-552-0200)
This section includes general responsibilities for respiratory care providers. More specific
requirements are described in different sections of this guide.
Providers must meet the general provider requirements in chapters 182-502 and 182-552 WAC
and this billing guide.
Licensed health care professionals
The agency requires that respiratory care providers employ a licensed health care professional
whose scope of practice allows providing respiratory care, including:
• Checking equipment to meet the client’s initial and ongoing needs.
• Communicating with the client’s authorized prescriber about any concerns or
recommendations.
(See WAC 182-552-0200(1) and the Department of Health’s licensing requirements)
Physician cosigning on face-to-face visits
(HCPCS code G0454)
To comply with federal regulations, medical supplies and equipment and home health services
must be cosigned by a physician, if ordered by a nonphysician provider.
• If the physician is cosigning the order (that was written by a nonphysician practitioner)
for medical equipment, the physician may bill using HCPCS code G0454. For all other
information regarding medical equipment, see the agency’s Nondurable medical supplies
and equipment billing guide.
• If the physician is cosigning the order (that was written by a nonphysician practitioner)
for home health services, the physician may bill the agency using CPT® code 99446. All
other information regarding home health services may be found in the agency’s Home
health services (acute care services) billing guide.
Respiratory Care
21
Are providers responsible to verify a client’s
coverage?
• Providers must verify the client’s eligibility in ProviderOne before providing services.
• If ProviderOne indicates the client is enrolled in a managed care plan, contact the client’s
MCO for all coverage conditions and limits on services. (See Client Eligibility).
• Bill the agency the usual and customary fee for clients not in managed care and residing
at home, in a skilled nursing facility or in a community residential setting.
Note: Also, see What are the client's rights for health care decisions?
Prescriptions
Respiratory care providers must:
• Keep initial and subsequent prescriptions in the client’s record.
• Verify that the client has a valid prescription. (See WACs 182-552-0200 and 182-552-
0800).
To be valid, a prescription must:
Be written, signed, and dated by a Medicaid-enrolled physician, advanced
registered nurse practitioner (ARNP), or physician’s assistant certified (PAC).
State the specific items or services requested, including the quantity, frequency,
and duration/length of need.
Note: Prescriptions that state only as needed or PRN are not sufficient.
For an initial prescription, not be older than 3 months from the date the prescriber
signed the prescription.
For subsequent prescriptions, not be older than 1 year from the date the prescriber
signs the prescription.
(For more details about oxygen prescriptions, see Requirements for valid oxygen
prescriptions.)
Respiratory Care
22
Respiratory care equipment and supplies
Respiratory care providers must:
• Obtain prior authorization (PA) from the agency, if required, before delivering
respiratory care equipment and supplies to the client and billing the agency.
• Make regular deliveries of medically necessary oxygen to the client’s home, skilled
nursing facility, community residential facility.
• Provide instructions to the client and the client’s caregiver on the safe and proper use of
the equipment provided.
• Maintain all rental equipment in good working condition on a continuous (24 hours a
day, seven days a week) basis.
• Furnish proof of direct delivery of equipment to a client or a client’s authorized
representative when requested by the agency. Proof of delivery must include:
The client’s name.
Detailed description of the item(s) delivered, including the quantity, brand name,
and serial number.
A signature and date by the client (or client’s authorized representative) when the
item was received.
(See WAC 182-552-0250).
• Provide a minimum warranty period of 1 year for all client-owned medical equipment
(excluding disposable/non-reusable supplies).
• Keep a copy of all warranties in the client’s file—including date of purchase, applicable
serial number, model number or other unique identifier of equipment, and warranty
period—and provide them to the agency upon request. If the warranty expires,
information must include the date of purchase and the warranty period. (See WAC 182-
552-1400).
Note: Under WAC 182-552-0200, the agency does not pay for respiratory care
equipment or supplies when the authorized prescriber providing a client’s
evaluation or an item’s medical justification also has a financial relationship with
the provider, including employment or a contract.

Respiratory Care
23
What are the client’s rights to health care
decisions?
(42 CFR §489.102)
All Medicare-Medicaid certified hospitals, nursing facilities, home health agencies, personal care
service agencies, hospices, and managed health care organizations are federally mandated to give
all adult clients written information about their rights, under state law, to make their own health
care decisions.
Clients have the right to:
• Accept or refuse medical treatment.
• Make decisions concerning their own medical care.
• Prepare an advance directive, such as a living will or durable power of attorney, for their
health care.
Respiratory Care
24
Coverage
What are the coverage criteria for respiratory
care services?
This section describes general clinical criteria and policies for respiratory care services,
equipment and supplies.
Inhalation drugs and solutions are included in the Medicaid prescription drug program (see
Chapter 182-530 WAC).
Note: Requests do not require prior authorization (PA) when meeting the clinical
criteria for covered respiratory care for Medicaid clients. When requests do not
meet the clinical criteria, as specified in this guide— including those associated
with expedited prior authorization (EPA)—PA is required. The agency evaluates
requests requiring PA on a case-by-case basis to determine whether they are
medically necessary. (See WAC 182-552-0001(4) and (5) and WAC 182-552-
1325). For more details about PA requests, including EPA and limitation
extension, see Authorization.
For details about specific items, see the Coverage Table. The coverage table lists equipment and
supplies with:
• Associated codes.
• Any authorization requirements (PA and EPA).
• Any limits and specific comments per code.
What types of airway clearance devices does the
agency cover?
(WAC 182-552-0600)
Clinical criteria
Chest physiotherapy (CPT), also known as percussion and postural drainage (P/PD), is
traditionally seen as the standard of care of secretion clearance methods. However, there are
client instances when conventional manual CPT is unavailable, ineffective, or not tolerated.
Respiratory Care
25
The agency covers the following types of airway clearance devices when medically necessary for
a person with a diagnosis characterized by excessive mucus production and difficulty clearing
secretions:
• Mechanical percussors
• Oscillatory positive expiratory pressure devices
• Positive expiratory pressure devices
• Cough stimulating devices, including replacement batteries,
alternating positive and negative airway pressure
• High frequency chest wall oscillation air-pulse generator system
For specific details about items covered, see Miscellaneous in the Coverage Table.
Does the agency cover the rental of apnea
monitors?
(WAC 182-552-0300)
Clinical criteria
The agency covers, without PA, the rental of an apnea monitor with recording feature for a
maximum of 6 months when:
• The vendor has a licensed clinician who:
Is competent in pediatric respiratory care.
Is responsible for managing the client’s apnea monitoring.
• The client is less than 1 year of age and meets at least one of the following clinical
criteria:
Born less than 37-weeks gestation, and the infant is not more than 43 weeks
corrected gestational age
Had an apparent life-threatening apneic event (defined as requiring mouth-to-
mouth resuscitation or vigorous stimulation)
Has been diagnosed with bradycardia and is being treated with caffeine,
theophylline, or other stimulating agents
Respiratory Care
26
Has documented gastro-esophageal reflux, which results in apnea, bradycardia, or
oxygen desaturation
Has documented apnea greater than 20 seconds in duration
Has apnea for periods less than 20 seconds in duration and accompanied by
bradycardia, cyanosis, or pallor
Has bradycardia (defined as heart rate less than 100 beats per minute)
Has oxygen desaturation below 90%
Has neurologic/anatomic/metabolic or respiratory diseases affecting respiratory
drive
Is a subsequent sibling of an infant who died of sudden infant death syndrome
(SIDS) until the client is 1 month older than the age at which the earlier sibling
died, and the client remains event-free
For each subsequent rental period:
• The client must continue to meet the clinical criteria for apnea monitors.
• The vendor must obtain PA from the agency.
The vendor must document the results of the use of the apnea monitor in the client’s records.
For specific details about items covered, see Apnea monitor and supplies in the Coverage Table.
Does the agency cover bi-level respiratory assist
devices (RADs)?
(WAC 182-552-0500)
Clinical criteria
The agency covers, without PA, one bi-level respiratory assist device (RAD), with or without a
back-up rate feature, per client every 5 years as long as the following criteria are met:
• The bi-level device has a data card.
• The client has one of the following conditions and meets the specific clinical criteria
specified in this section:
Restrictive thoracic disorders (such as neuromuscular diseases or severe thoracic
cage abnormalities)

Respiratory Care
27
Severe chronic obstructive pulmonary disease (COPD)
Central or complex sleep apnea
Hypoventilation syndrome
PA is required for Bi-Level RADs if one of the following applies:
• The client does not meet the required clinical criteria.
• The agency has purchased a CPAP device or other RAD for the client within the last 5
years.
Bi-level RAD without the back-up rate feature
For a bi-level RAD without the back-up rate feature, the agency:
• Pays for rental of the device during an initial 3-month period.
The treating authorized prescriber must:
Conduct a face-to-face clinical re-evaluation of the client between day 31 and day
91 of the rental period.
In order to continue rental of the device, document the following items in the
client’s file to show:
The progress of the client’s relevant symptoms.
The client’s compliance with using the device.
• Purchases the device after the requirements for the rental are met.
Bi-level RAD with the back-up rate feature
For a bi-level RAD with the back-up rate feature used with an invasive interface, the agency
pays for the rental only.
For a bi-level RAD with the back-up rate feature used with a noninvasive interface, the agency:
• Pays for rental of the device during an initial 3-month period. The treating authorized
prescriber must:
Conduct a face-to-face clinical re-evaluation of the client between 31 and 91 days
of the rental period.
Respiratory Care
28
In order to continue rental of the device, document the following items in the
client’s file to show:
The progress of the client’s relevant symptoms.
The client’s compliance with using the device.
• Purchases after a total of 13 months of rental.
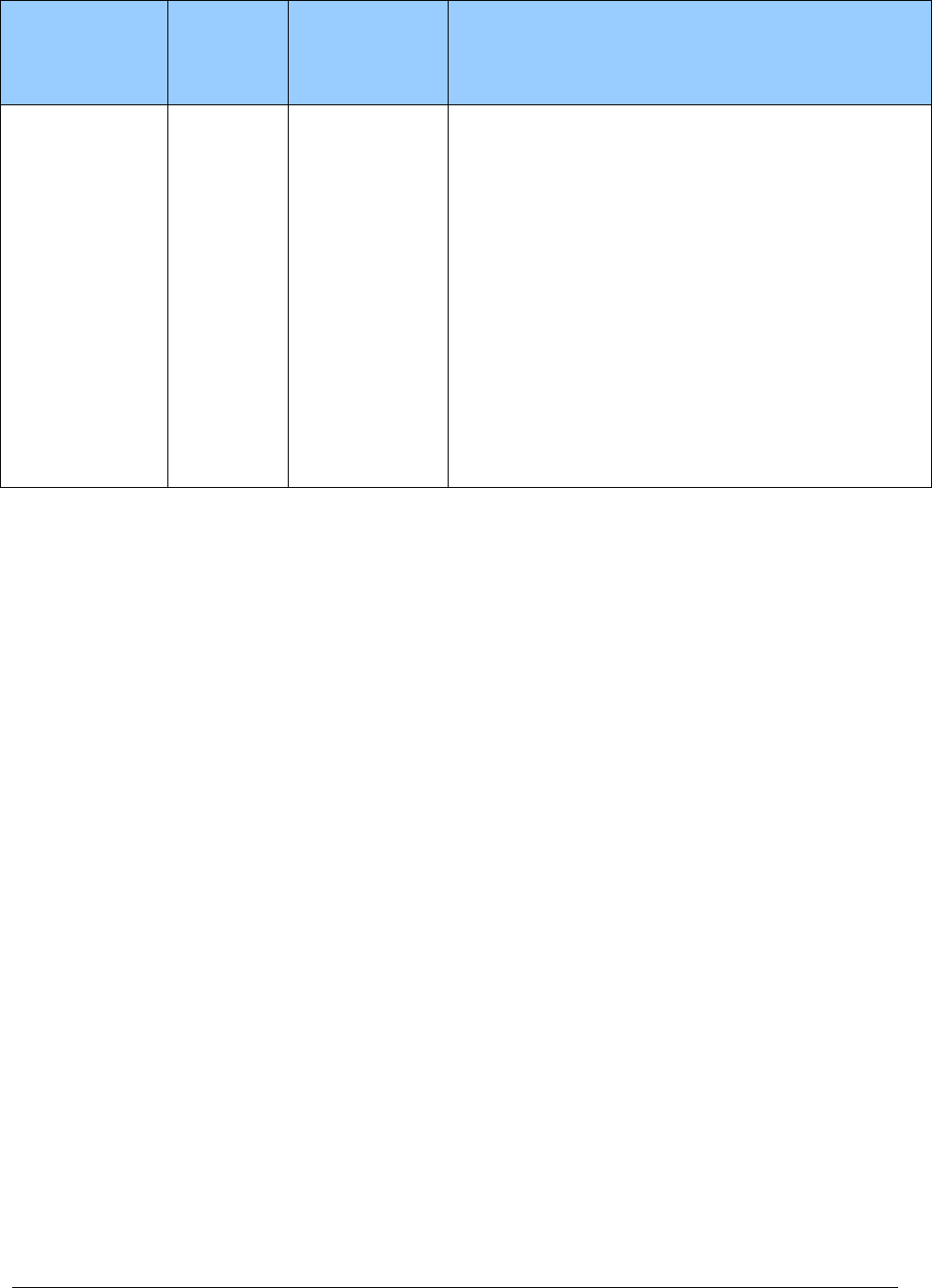
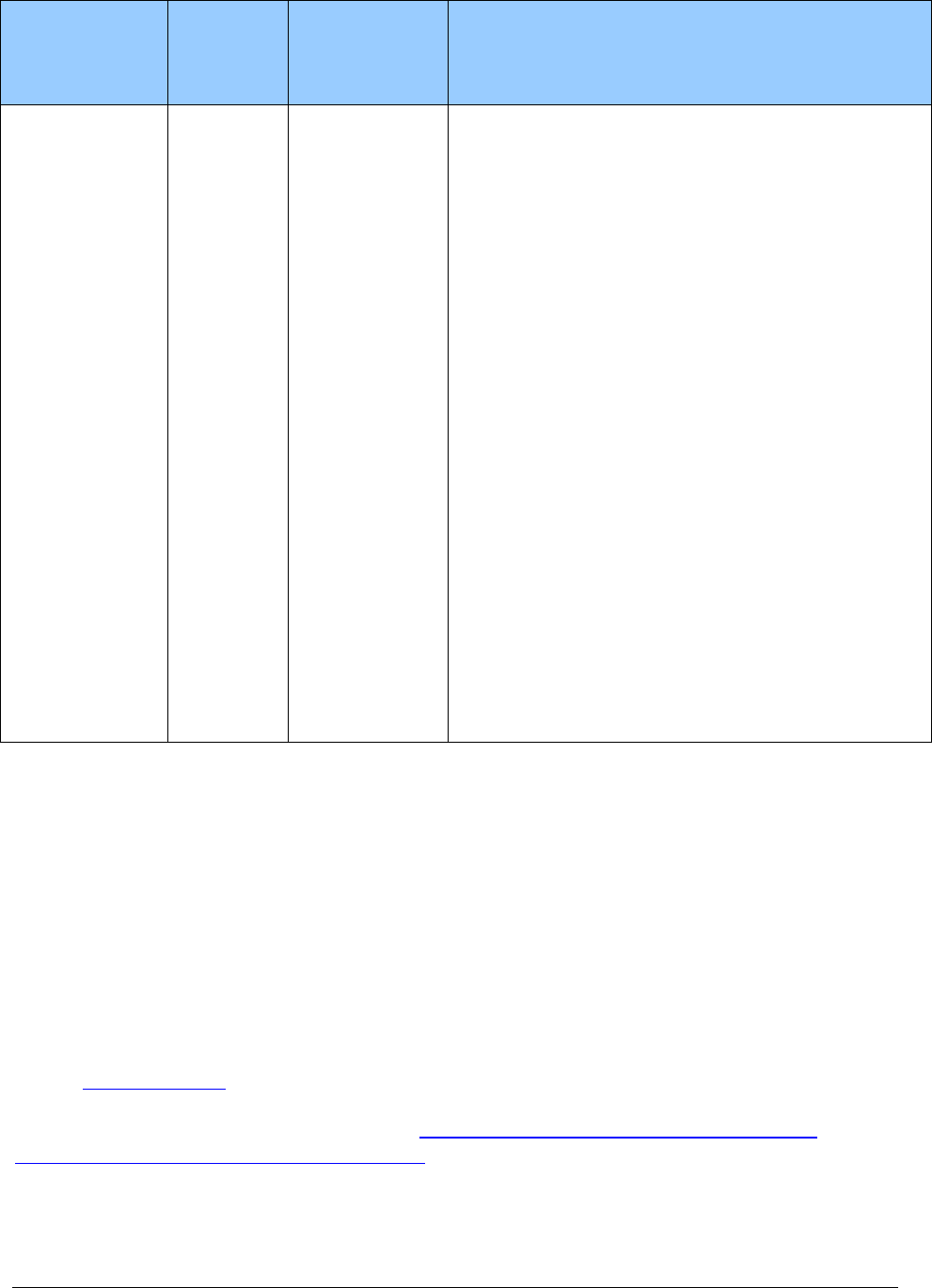
Required clinical criteria for using RADs with specific types
of respiratory disorders
Type of
Respiratory
Disorder
Type of
Device
Paid by
Agency
PA
Required Clinical Criteria
Restrictive
Thoracic
Disorders
Bi-level
RAD
device with
or without
back-up
rate feature
No—when all
clinical criteria
are met
• The client has been diagnosed with a neuromuscular
disease, such as amyotrophic lateral sclerosis (ALS)
or a severe thoracic cage abnormality (for example,
post-thoracoplasty for tuberculosis).
• Chronic obstructive pulmonary disease (COPD) does
not contribute significantly to the person’s
pulmonary limitation.
• The client also meets one or more of these clinical
criteria:
An arterial blood gas PaCO
2
, done while awake
and breathing the client’s prescribed FIO
2
(fractionated inspired oxygen concentration) is
≥ 45 mm Hg.
Sleep oximetry demonstrates an oxygen
saturation ≤ 88% for ≥ 5 minutes of nocturnal
recording time (minimum record time of 2
hours), done while breathing the client’s
prescribed recommended FIO
2
.
For a neuromuscular disease (only), either:
Maximal inspiratory pressure is < 60 cm
H2O.
Forced vital capacity is ≤ 50% predicted.
Respiratory Care
29
Type of
Respiratory
Disorder
Type of
Device
Paid by
Agency
PA
Required Clinical Criteria
Severe Chronic
Obstructive
Pulmonary
Disease (COPD)
Bi-level
RAD
device
without
back-up
rate feature
No—when all
clinical criteria
are met
The client meets all these clinical criteria:
• An arterial blood gas PaCO
2
, done while awake and
breathing the client’s prescribed FIO
2
, is ≥ 52 mm
Hg.
• Sleep oximetry demonstrates oxygen saturation ≤
88% for ≥ 5 minutes of nocturnal recording time
(minimum recording time of 2 hours), done while
breathing oxygen at 2 LPM or the client’s prescribed
FIO
2
(whichever is higher).
• Before initiating therapy, obstructive sleep apnea
and treatment with CPAP has been considered and
ruled out.
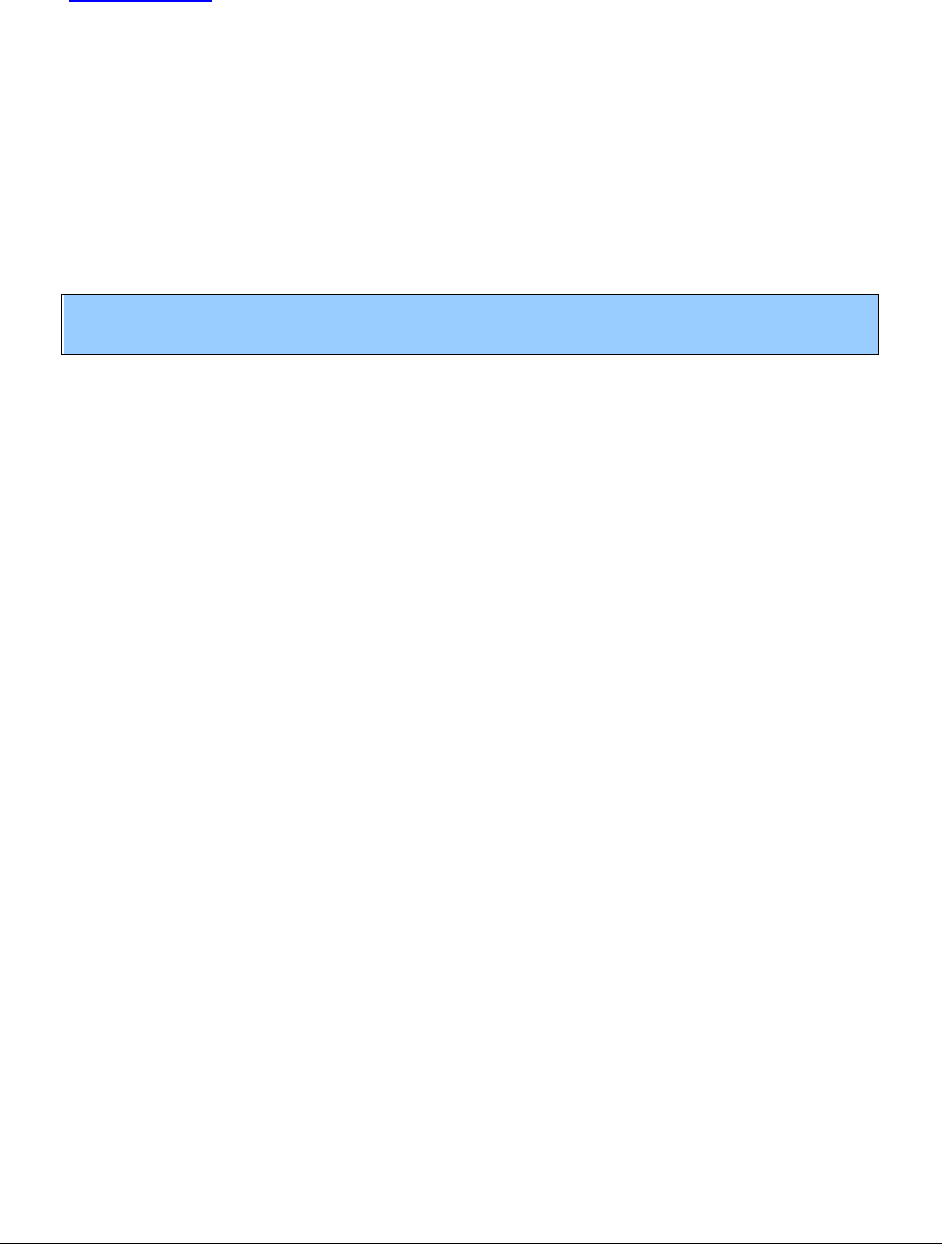
Respiratory Care
30
Type of
Respiratory
Disorder
Type of
Device
Paid by
Agency
PA
Required Clinical Criteria
COPD (cont.)
Bi-level
RAD
device with
the back-up
rate feature
No—when all
clinical criteria
are met
Started any time after the initial use of the bi-level
RAD without the backup rate feature when both
these clinical criteria are met:
• An arterial blood gas PaCO
2
, done while awake
and breathing, the client’s prescribed FIO
2
shows
that the client’s PaCO
2
, worsens ≥ 7 mm Hg
compared to the original result from using the bi-
level RAD without the back-up rate feature.
• A facility-based PSG demonstrates oxygen
saturation ≤ 88% for ≥ 5 minutes of nocturnal
recording time (minimum recording time of 2 hrs)
while using a bi-level RAD without the back-up
feature. (Not caused by obstructive upper airway
events—that is, AHI less than 5).
-OR-
Started at a time no sooner than 61 days after initial
use of the bi-level RAD without the back-up rate
feature when both these clinical criteria are met:
• An arterial blood gas PaCO
2
, done while awake
and breathing, the client’s prescribed FIO
2
still
remains ≥ 52 mm Hg.
• Sleep oximetry while breathing with the bi-level
RAD without the back-up rate demonstrates
oxygen saturation ≤ 88% for ≥ 5 minutes of
nocturnal recording time (minimum recording time
of 2 hrs), done while breathing oxygen at 2 LPM or
the client’s prescribed FIO
2,
whichever is higher.
Central or
Complex Sleep
Apnea
(not due to
airway
obstruction)
Bi-level
RAD
device with
or without
the back-up
rate feature
No—when the
client’s
polysomnogram
test meets
clinical criteria
The client’s polysomnogram test reveals both:
• The diagnosis of central sleep apnea (CSA) or
complex sleep apnea (CompSA).
• Significant improvement of the sleep-associated
hypoventilation with the use of a bi-level RAD
device with or without the back-up rate feature on
the settings that will be prescribed for initial use at
home, while breathing the client’s usual FIO
2.
Respiratory Care
31
Type of
Respiratory
Disorder
Type of
Device
Paid by
Agency
PA
Required Clinical Criteria
Obstructive
Sleep Apnea
(OSA)
Bi-level
RAD
device
without the
back-up
rate feature
No—when all
clinical criteria
are met
The client meets the clinical criteria for a CPAP.
However, the CPAP has been tried and proven
ineffective.
Ineffective in this case, is defined as documented
failure to meet therapeutic goals using a CPAP during
either:
• The titration portion of a facility-based study.
• Home use despite optimal therapy (that is, proper
mask selection and fitting and appropriate pressure
setting).
Hypoventilation
Syndrome
Bi-level
RAD
device
without the
back-up
rate feature
No—when all
the clinical
criteria are met.
The client meets one of these three sets of clinical
criteria:
• An initial arterial blood gas PaCO2, done while
awake and breathing the client’s prescribed FIO
2
, ≥
to 45 mm Hg.
• Spirometry shows an FEV1/FVC ≥ to 70% and an
FEV1 ≥ 50% of predicted.
-OR-
• An arterial blood gas PaCO2, done during sleep or
immediately upon awakening, and breathing the
client’s prescribed FIO
2
, shows the client’s PaCO2
worsened ≥ to 7 mm Hg compared to the original
result.
-OR-
• A facility-based PSG demonstrates oxygen
saturation ≤ 88% for ≥ to 5 continuous minutes of
nocturnal recording time (minimum recording time
of 2 hours) that is not caused by obstructive upper
airway events—that is, AHI less than 5.
Respiratory Care
32
Type of
Respiratory
Disorder
Type of
Device
Paid by
Agency
PA
Required Clinical Criteria
Hypoventilation
Syndrome
(cont.)
Bi-level
RAD
device with
the back-up
rate feature
No- when all the
clinical criteria
are met.
The client meets both of these clinical criteria:
• A covered bi-level RAD without the back-up rate
feature is being used.
• Spirometry shows an FEV1/FVC ≥ 70% and an
FEV1 ≥ 50% of predicted.
The client also meets one of these clinical criteria:
• An arterial blood gas PaCO2, done while awake and
breathing the client’s prescribed FIO2, shows that
the client’s PaCO2 worsens ≥ 7 mm Hg compared
to the ABG result performed to qualify the client for
the bi-level RAD without the back-up rate feature.
-OR-
• A facility-based PSG demonstrates oxygen
saturation ≤ to 88% percent for ≥ 5 continuous
minutes of nocturnal recording time (minimum
recording time of 2 hours) that is not caused by
obstructive upper airway events—that is, AHI less
than 5 while using a bi-level RAD without the back-
up rate feature.
Replacement of bi-level RAD equipment and supplies
• PA is required for the replacement of a bi-level RAD device if the client has had the
device for less than 5 years.
• After 5 years, the client’s authorized prescriber must conduct a face-to-face evaluation
documenting that the client continues to use and benefit from the bi-level RAD device. A
new polysmnogram (PSG) (sleep test), trial period, or PA is not required.
• The agency pays for replacement supplies for a bi-level RAD device, as identified in the
Coverage Table.
For specific details about items covered, see Continuous positive airway pressure system and
Ventilators and related respiratory equipment in the Coverage Table.
The agency does not cover accessories or services not specifically identified in this guide.
Respiratory Care
33
Does the agency cover continuous positive airway
pressure (CPAP) and supplies?
(WAC 182-552-0400)
Clinical criteria
The agency covers, without PA, one continuous positive airway pressure (CPAP) device
including related supplies, per client, every 5 years when all the following criteria are met:
• The client is diagnosed with obstructive sleep apnea using a clinical evaluation and a
positive attended polysomnogram (PSG) performed in a sleep laboratory or performed
during an unattended home sleep study.
Notes: The agency does not pay for a CPAP device when the client is diagnosed
with upper airway resistance syndrome (UARS).
• CPAP is the least costly, most effective treatment modality.
• The CPAP device has a data card and is FDA approved.
• The item requested is not included in any other reimbursement methodology such as the
diagnosis-related group (DRG).
Additional criteria for clients age 13 and older
• The client’s polysomnogram demonstrates an apnea-hypopnea index (AHI) ≥ 15 events
per hour with a minimum of 30 events.
-OR-
• The client’s PSG demonstrates the AHI is ≥ 5 and ≤ 14 events per hour with a minimum
of 10 events and clinical documentation of one of the following:
Excessive daytime sleepiness, impaired cognition, mood disorders, or insomnia.
Hypertension, ischemic heart disease, or history of stroke.
Additional criteria for clients age 12 and younger
Clinical criteria must include:
• A documented diagnosis of obstructive sleep apnea (OSA).
Respiratory Care
34
• A PSG that demonstrates an apnea index (AI) or apnea-hypopnea index (AHI) ≥ 1 and
one of the following:
Adenotonsillectomy has been unsuccessful in relieving OSA.
Adenotonsillar tissue is minimal.
Adenotonsillectomy is inappropriate based on OSA being attributable to another
underlying cause (such as craniofacial anomaly or obesity) or adenotonsillectomy
is contraindicated.
The client’s family does not wish to pursue surgical intervention.
Note: The AHI is calculated on the average number of events per hour. If the AHI
is calculated based on less than two hours of sleep or recording time, the total
number of recorded events used to calculate the AHI must be at least the number
of events that would have been required in a two-hour period (that is, must reach
at least 30 events without symptoms or at least 10 events with symptoms).
Use of RAD instead of CPAP
If a client meets the criteria for CPAP, but a CPAP device has been tried and proven ineffective,
the agency will cover a bi-level RAD without the back-up. Ineffective, in this case, means
documented failure to meet therapeutic goals using a CPAP during either:
• The titration portion of a facility-based study.
• Home use despite optimal therapy (that is, proper mask selection and fitting and
appropriate pressure setting).
Prior authorization for a CPAP device
PA is required for a CPAP device if either:
• The client does not meet the required clinical criteria.
• The agency has purchased either a CPAP or a bi-level RAD device for the client within
the last 5 years.
Respiratory Care
35
Rental and purchase of a CPAP device
After the initial 3-month rental period for a CPAP device, the agency will consider purchasing
this device for the client.
Note: The provider must submit a purchase request to the agency. The following
documentation of clinical benefit must be recorded in the client’s file:
• A face-to-face clinical re-evaluation of the client by the authorized
prescriber, which documents that symptoms of obstructive sleep apnea are
improved.
• A review of objective evidence by the authorized prescriber of the client’s
adherence* to use of the CPAP device.
*Adherance is defined as use of the CPAP device ≥ 4 hours per night on 70% of
nights during a consecutive 30-day period anytime during the first 3 months of
initial usage.
For specific details about CPAP-related covered items, see Continuous positive airway pressure
system in the Coverage Table.
Replacement of CPAP equipment and supplies
• PA is required for the replacement of a CPAP device if the client has had the device for
less than 5 years.
• After 5 years, the client’s treating authorized prescriber must conduct a face-to-face
evaluation documenting that the client continues to use and benefit from the CPAP
device. A new PSG (sleep test), trial period, or PA is not required.
• The agency pays for replacement supplies for a CPAP device, as identified in Continuous
positive airway pressure system in the Coverage Table.
Respiratory Care
36
Does the agency cover nebulizers and related
compressors?
(WAC 182-552-0650)
Clinical criteria
The agency covers, without PA, the purchase of a nebulizer and related compressor, with limits,
when the following clinical criteria are met:
• The small volume nebulizer and related compressor are covered for administering
inhalation drugs for:
The management of obstructive pulmonary disease.
A client with cystic fibrosis or bronchiectiasis.
A client with HIV, pneumocystosis, or complications of organ transplants.
Persistent, thick, or tenacious pulmonary secretions.
• The large volume nebulizer and related compressor are covered to deliver humidity to a
client who has thick, tenacious secretions and has:
Cystic fibrosis.
Bronchiestasis.
A tracheostomy.
A tracheobronchial stent.
• The filtered nebulizer is covered when necessary to administer pentamidine to clients
with HIV, pneumocystosis, or complications of organ transplants.
The agency does not pay for a large volume nebulizer, related compressor/generator, and water
or saline when used predominantly to provide room humidification.
For specific details about items covered, see Nebulizer and Accessories in the Coverage Table.
Respiratory Care
37
Does the agency cover oximeters?
(WAC 182-552-0900)
For clients age 17 and younger
Clinical criteria for standard oximeters
The agency covers the purchase of a standard oximeter, without PA, for clients age 17 and
younger in the home when the client meets one of the following criteria:
• Has chronic lung disease and is on supplemental oxygen
• Has a compromised or artificial airway
• Has chronic lung disease requiring a ventilator or a bi-level RAD
Clinical criteria for enhanced oximeters
The agency covers the purchase of enhanced oximeters with expedited prior authorization (EPA)
for clients age 17 and younger in the home when the clinical criteria for the standard oximeter
and EPA criteria are met. See EPA #870000006. If the client does not meet the EPA criteria, PA
is required. See What is prior authorization (PA)?
For clients age 18 and older
Clinical criteria for standard and enhanced oximeters
The agency covers the purchase of standard and enhanced oximeters, with PA, for clients age 18
and older in the home when the client meets one of the following criteria:
• Has chronic lung disease and is on supplemental oxygen
• Has a compromised or artificial airway
• Has chronic lung disease requiring a ventilator or a bi-level RAD
For specific details about items covered, see Miscellaneous in the Coverage Table.
Does the agency cover oxygen?
(WACs 182-552-0200 and 182-552-0800)
The agency covers oxygen, without PA, when the clinical criteria are met.
Respiratory Care
38
Requirements for valid oxygen prescriptions
(WAC 182-552-0200)
• The agency requires a valid prescription for oxygen under WAC 182-552-0200.
• When prescribing oxygen, follow these requirements:
Include the flow rate of oxygen, estimated length of need, frequency and duration
of oxygen use, and the client’s oxygen saturation level on the prescription.
Prescriptions that state only as needed or PRN are not sufficient.
Recertify clients who meet Group I clinical criteria 1 year after initial
certification.
Recertify clients who meet Group II clinical criteria 3-months after initial
certification.
Use the client’s oxygen saturation or laboratory values to meet recertification
requirements.
• The agency requires that documentation be kept in the client’s record for oxygen
saturation and lab values to verify the medical necessity of continued oxygen.
The provider may perform the oxygen saturation measurements.
The agency does not accept lifetime certificates of medical need (CMNs). (See
WAC 182-552-0800.)
Respiratory Care
39
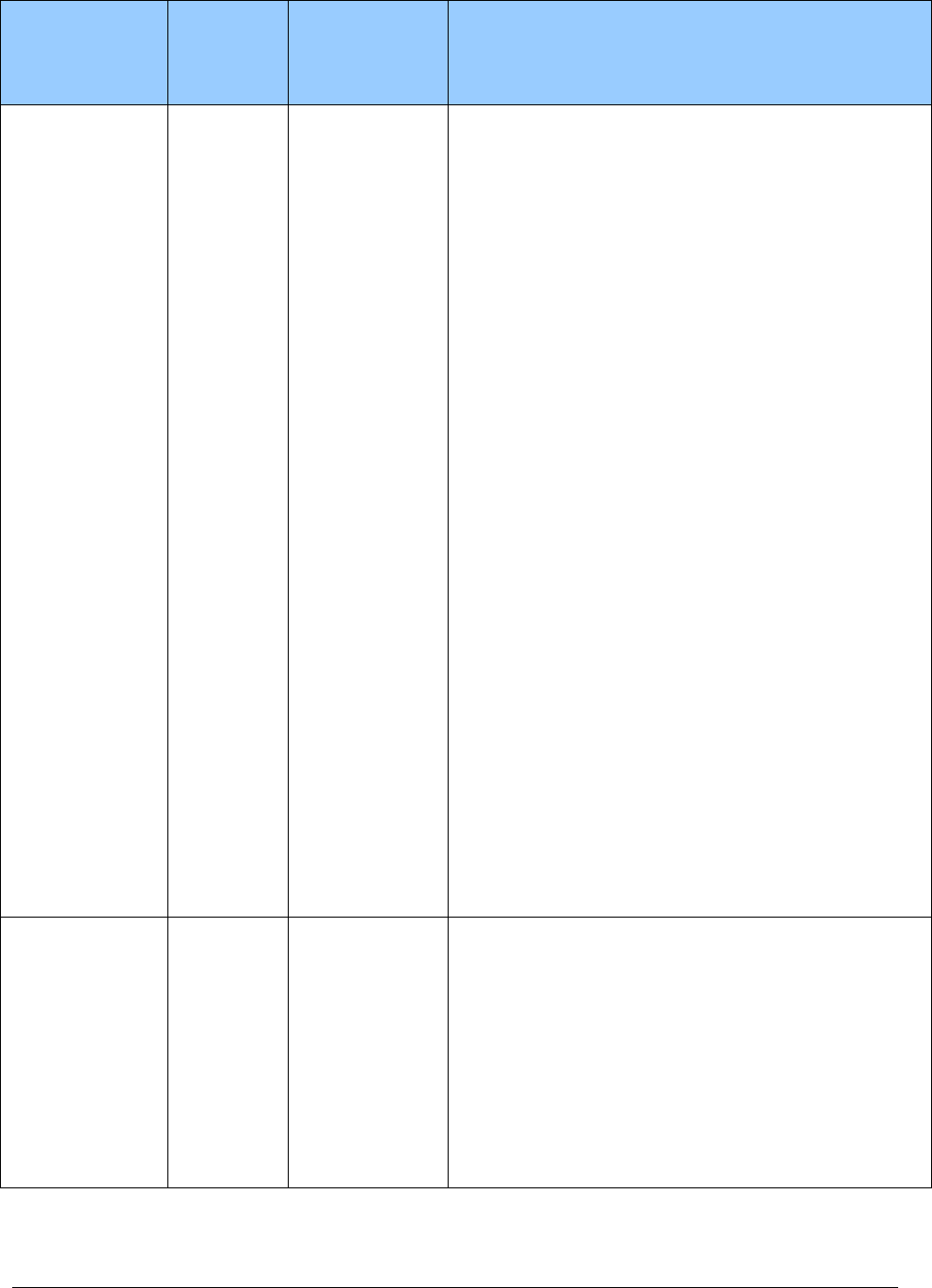
Coverage criteria for oxygen
Criteria
Initial
Prescription
Renew
Prescription
Documented
Verification
by Provider
For Group I
clients
(
chronic oxygen
clients with
obvious
respiratory
challenges as
evidenced by
low oxygen
saturation)
Any of the following:
• An arterial PaO2 at or below 55mm
Hg or an arterial oxygen saturation
(SaO2) at or below 88% taken at rest
(awake).
• An arterial PaO2 at or below 55 mm
Hg, or an arterial oxygen saturation at
or below 88% for at least 5 minutes,
taken during sleep for a client who
demonstrates an arterial PaO2 at or
above 56 mm Hg or an arterial
oxygen saturation at or above 89%
while awake.
• A decrease in arterial PaO2 more than
ten mm Hg, or a decrease in arterial
oxygen saturation more than 5% from
baseline saturation for at least five
minutes taken during sleep associated
with symptoms (for example,
impairment of cognitive processes
and nocturnal restlessness or
insomnia) or signs (for example, cor
pulmonale, P pulmonale on EKG,
documented pulmonary hypertension
and erythrocytosis) reasonably
attributable to hypoxemia.
• An arterial PaO2 at or below 55 mm
Hg or an arterial oxygen saturation at
or below 88%, taken during exercise
for a client who demonstrates an
arterial PaO2 at or above 56 mm Hg
or an arterial oxygen saturation at or
above 89% during the day while at
rest. In this case, oxygen is provided
during exercise if it is documented
that the use of oxygen improves the
hypoxemia that was demonstrated
during exercise when the client was
breathing room air.
12 months or
length of need
specified by
authorized
prescriber,
whichever is
shorter
A least
every 12
months
thereafter,
provided
that clinical
criteria
continue to
be met
For both the
initial and
renewal
prescriptions,
document how
the client
specifically
meets the
criteria.
For ongoing
coverage, the
provider
may perform
the oxygen
saturation
measurements.
Respiratory Care
40
Criteria
Initial
Prescription
Renew
Prescription
Documented
Verification
by Provider
For Group II
clients
(
borderline
oxygen clients—
their blood
saturation levels
seem to be
within the
normal range,
but additional
extenuating
issues suggest a
need for oxygen)
• The presence of an arterial PaO2 of
56-59 mm Hg or an arterial blood
oxygen saturation of 89% at rest
(awake), during sleep for at least five
minutes, or during exercise (as
described under Group I criteria).
AND
• Any of the following:
Dependent edema suggesting
congestive heart failure.
Pulmonary hypertension or cor
pulmonale, determined by
measurement of pulmonary artery
pressure, gated blood pool scan,
echocardiogram, or P pulmonale
on EKG (P wave greater than 3
mm in standard leads II, III, or
AVF).
Erythrocythemia with a
hematocrit greater than 56%.
3 months or
length of need
specified by
authorized
prescriber,
whichever is
shorter
3 months
after initial
prescription
and annually
thereafter,
provided
that clinical
criteria
continue to
be met
For both the
initial and
renewal
prescriptions,
document how
the client
specifically
meets the
criteria.
For ongoing
coverage, the
provider
may perform
the oxygen
saturation
measurements.
Renting capped-rental oxygen systems and contents
(WAC 182-552-0800)
• Capped rental applies only to in-home oxygen use by medical assistance clients. Oxygen
systems are considered capped rental (provider continues to own the equipment) after 36
months.
• The agency makes only 36 rental payments for stationary oxygen system and portable
oxygen system equipment.
• During the rental period, the agency’s payment includes any supplies, accessories,
oxygen contents, delivery and associated costs, instructions, maintenance, servicing, and
repairs.
• Throughout the 36-month capped rental period, the supplier who provides the oxygen
equipment for the first month must continue to provide any necessary oxygen equipment
and related items and services.
Respiratory Care
41
• The supplier (provider) must continue to provide the client with properly functioning
oxygen equipment (including maintenance and repair), and associated supplies for the
remaining 24 months of the equipment’s reasonable useful lifetime (RUL).
During the remaining 24 months, the supplier may bill the agency only for:
Oxygen contents.
Disposable supplies.
Maintenance fees, which are limited to one every 6 months.
• The provider may replace the equipment any time after the end of the 5-year RUL, which
begins a new 36-month rental period.
• Using the EPA process, providers may restart a 36-month rental period in any of the
following situations:
The initial provider is no longer providing oxygen equipment or services.
The initial provider’s core provider agreement with the agency is terminated or
expires.
The client moves to an area that is not part of the provider’s service area. (This
applies to Medicaid-only clients.)
The client moves into a permanent residential setting.
A pediatric client is transferred to an adult provider.
• Once a provider requests and receives PA, the agency may authorize a restart of the 36-
month rental period when:
Extenuating circumstances occur, resulting in a loss or destruction of oxygen
equipment (for example, fire, or flood). (See WAC 182-501-0050(7)).
The client was exercising reasonable care.
Note: For further details, see the EPA criteria table and the EPA process in
Authorization.
Respiratory Care
42
Stationary and portable oxygen systems and contents
(WAC 182-552-0800)
The agency covers, without PA, the rental of a stationary oxygen system and a portable oxygen
system, as follows:
• For clients age 20 and younger, when prescribed by the client's treating practitioner.
• For clients age 21 and older, when prescribed by a practitioner and the client meets
Medicare group I or group II clinical criteria as defined in WAC 182-552-0005. PA is
required for clients age 21 and older, who do not meet Medicare clinical criteria.
• Stationary oxygen systems are one of the following:
Compressed gaseous oxygen
Stationary liquid oxygen
A concentrator
• A portable oxygen system can be either gas or liquid.
For specific details about items covered, see Oxygen and oxygen equipment.
Rental
• The agency pays a maximum of one rental payment every 30 days (1 unit=30 days) per
client for stationary or portable oxygen systems, including oxygen contents.
• Billing and payment is based on a 30-day period, not a monthly calendar period. The
period starts on the day of delivery, and is a rolling 30-day period.
• The rental of a stationary oxygen system and a portable oxygen system is covered
without prior authorization for clients who are:
Age 20 and younger, when prescribed by the client’s treating practitioner.
Age 21 and older, when prescribed by a practitioner and the client meets Group I
or Group II clinical criteria.
• PA is required for clients age 21 and older who do not meet clinical criteria for rental of a
stationary oxygen system or a portable oxygen system.
Additional Rental Information
The agency pays a monthly amount per client for oxygen and oxygen equipment. For stationary
oxygen equipment, this monthly amount covers the oxygen equipment, contents, and supplies
and is subject to adjustment depending on the amount of oxygen prescribed (liters per minute –
LPM) and whether or not portable oxygen is also prescribed.

Respiratory Care
43
Prescribed flow rate (liters per minute – LPM)
of oxygen when client is at rest
Modifier
Description
QE
Prescribed amount of stationary oxygen while at rest is less than 1 LPM
QF
Prescribed amount of stationary oxygen while at rest exceeds 4 LPM and
portable oxygen is prescribed
QG
Prescribed amount of stationary oxygen while at rest is greater than 4 LPM
If the prescribed amount of oxygen is less than 1 LPM, the agency reduces the maximum
allowable amount for stationary oxygen rental by 50%.
The agency increases the maximum allowable amount for stationary oxygen equipment rental
under the following conditions. If both conditions apply, vendors use the higher of either of the
following add-ons. Vendors are not paid for both add-ons.
• Volume adjustment – Add On
If the prescribed amount of oxygen for stationary equipment exceeds 4 liters per
minute, the fee schedule amount for stationary oxygen rental is increased by 50%.
If the prescribed liter flow for stationary oxygen equipment is different than the
flow for portable oxygen equipment, or the flow is different for when the client is
at rest or is exercising, vendors must use the prescribed amount for stationary
sytems and for clients at rest.
If the prescribed liter flow is different for day and night use, venders use the
average of the two rates.
• Portable Oxygen - Add-On – If portable oxygen is prescribed, the fee schedule amount
for portable equipment is added to the fee schedule amount for stationary oxygen
equipment rental.
Varying prescribed flow rate
(liters per minute – LPM) of oxygen
To provide greater specificity in the modifiers used for oxygen volume adjustment in instances
where there are varying prescribed flow rates, use one of the following modifiers on the claim
to identify the prescribed flow rate and to ensure appropriate use of modifiers in all cases
based on the prescribed flow rate at rest (or at night or based on the average of the rate at rest
and at night, if applicable).
Modifier
Description
QA
Prescribed amounts of stationary oxygen for daytime use while at rest and
nighttime use differ and the average of the two amounts is less than 1 LPM
QB
Prescribed amount of stationary oxygen for daytime use while at rest and
nighttime use differ and the average of the two amounts exceeds 4 LPM and
portable oxygen is prescribed
QR
Prescribed amount of stationary oxygen for daytime use while at rest and
nighttime use differ and the average of the two amounts is greater than 4 LPM

Respiratory Care
44
Contents
The agency pays a maximum of one payment for oxygen contents, per client, every 30 days
when the client owns the oxygen system or when the capped rental period is met.
Maintenance
The agency pays one maintenance fee every 6 months for an oxygen concentrator and oxygen
transfilling equipment only when the capped rental period is met or the client owns the oxygen
concentrator. The maintenance fee is 50% of the monthly rental rate.
What types of services, equipment, and supplies
does the agency not pay for?
• The agency does not pay for oxygen therapy and related services, equipment or supplies
for clients age 21 and older with, but not limited to, any one of the following conditions:
Angina pectoris in the absence of hypoxemia.
Dyspnea without cor pulmonale or evidence of hypoxemia.
Severe peripheral vascular disease resulting in clinically evident desaturation in
one or more extremities but in the absence of systemic hypoxemia.
• The agency does not pay separately for:
Accessories, such as humidifiers, necessary for the effective use of oxygen
equipment. These are included in the monthly rental payment.
Spare tanks of oxygen and related supplies as back-up or for travel.
Respiratory Care
45
Does the agency cover suction pumps and
supplies?
(WAC 182-552-1100)
The agency:
• Covers suction pumps and supplies when medically necessary for airway clearance or
tracheostomy suctioning.
• Pays for a maximum of two suction devices per client in a 5-year period as follows:
The agency rents one primary suction device (stationary or portable) per client for
use in the home and one secondary suction device per client for back-up or
portability.
The agency considers the suction devices purchased after 12 months’ rental.
For specific details about items covered, see Suction pumps/supplies.
Does the agency cover ventilator equipment and
supplies?
(WAC 182-552-1000)
Primary ventilator
• The agency covers the rental of a ventilator, equipment, and disposable ventilator
supplies when the client requires periodic or mechanical ventilation for the treatment of
chronic respiratory failure resulting from hypoxemia or hypercapnia.
• The agency covers medically necessary ventilator equipment rental and related
disposable supplies when all of the following apply:
There is a prescription for the ventilator.
The ventilator is to be used exclusively by the client for whom it is requested.
The ventilator is FDA-approved.
The item requested is not included in any other reimbursement methodology such
as, but not limited to, diagnosis-related group (DRG).
Respiratory Care
46
• The agency’s monthly rental rate includes ventilator maintenance and accessories,
including but not limited to:
Alarms
Adapters
Batteries
Cables
Chargers
Circuits, and filters
Connectors
Fittings
Humidifiers
Nebulizers
Temperature probes
Tubing
Note: The agency does not pay separately for ventilator accessories unless the client
owns the ventilator system.
Secondary (back-up) ventilators
The agency covers a secondary (back-up) ventilator at 50% of the monthly rental rate when one
or more of the following clinical criteria are met:
• The client cannot maintain spontaneous or adequate ventilation for four or more
consecutive hours.
• The client lives in an area where a replacement ventilator cannot be provided within two
hours.
• The client requires mechanical ventilation during mobility as prescribed in their plan of
care.
Expedited Prior Authorization
The agency requires an EPA for all ventilators. What is expedited prior authorization (EPA)?
All ventilators are subject to authorization. At the time of authorization, the following criteria
must be documented in the patient record, and available to the agency upon request:
• Medical history (not required if request is for continuation of services)
• Diagnosis and degree of impairment
• Degree of ventilatory support required (e.g., continuous, nocturnal only)
• Ventilator settings/parameters including mode and type of ventilator ordered at time of
authorization request
The EPA is valid for either 6 or 12 months. If the client has no clinical potential for weaning, the
agency’s EPA is valid for 12 months. If the client has the potential to be weaned, the agency’s
EPA is valid for 6 months.
For specific details about items covered, see Ventilators and related respiratory equipment.
Respiratory Care
47
Coverage Table
Bill With:
Taxonomy 332BX2000X.
Do Not Bill With:
Any procedure code listed in the Do Not Bill With column of the
fee schedule is AT NO TIME allowed in combination with the
primary code located in the Hospital Common Coding System
(HCPCS) Code column.
Maximum
Allowance:
Rentals are calculated on a 30-day basis unless otherwise indicated. In
those instances where rental is required before purchase, the rental
price is applied towards the purchase price.
Rentals:
From and to dates are required on all rental billings.
(1 month equals 30 days.)
REMINDER: See the Respiratory care fee schedule for payment requirements.
Notes: Providers must monitor the amount of supplies and accessories a client is
actually using and assure the client has nearly exhausted the supply on hand
before dispensing any additional items.
For policy requirements, including clinical criteria, for different types of
equipment and supplies, see Coverage Criteria. For an explanation of PA,
including EPA and limitation extension, see Authorization.
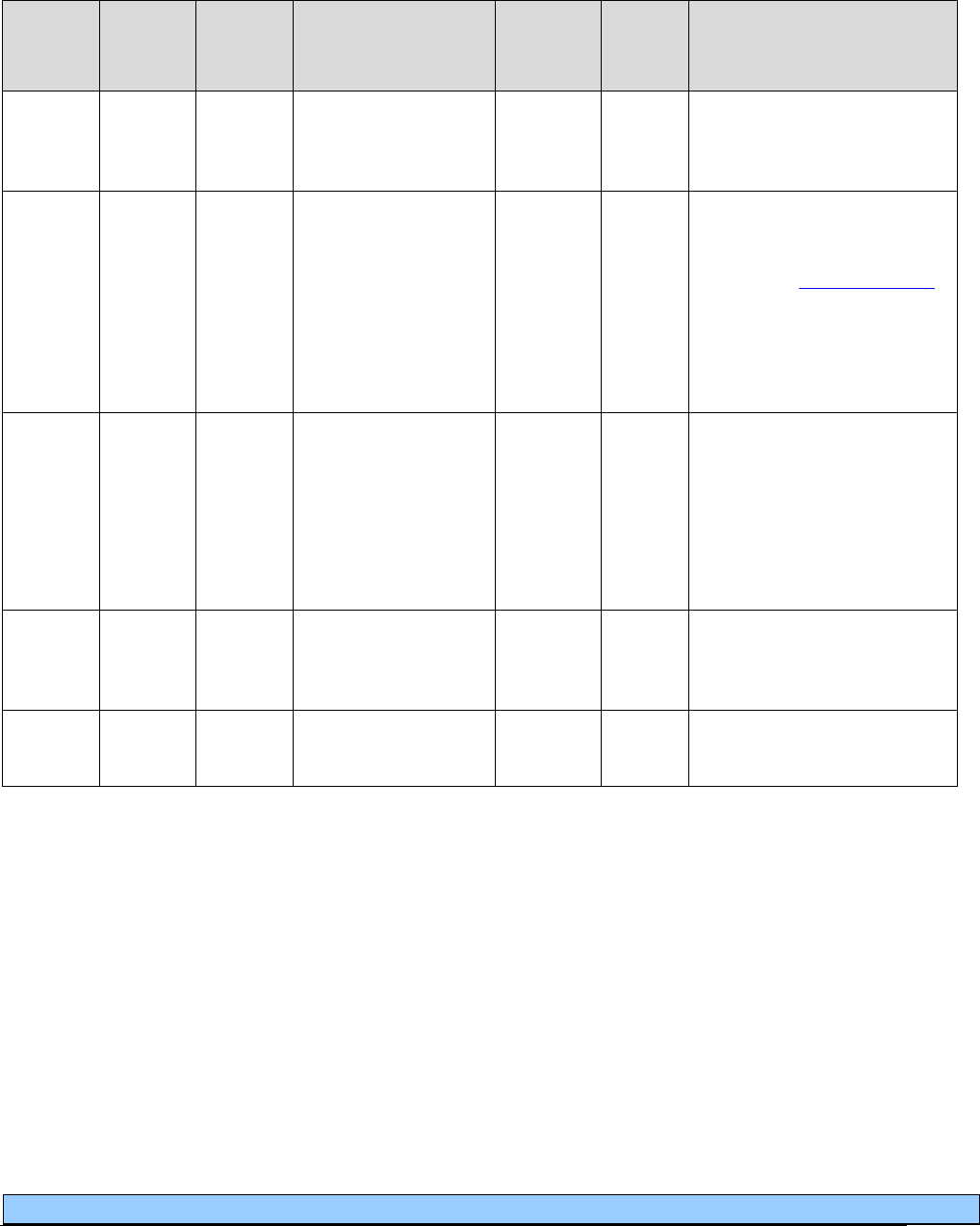
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
48
Apnea monitor and supplies
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
NC
E0618
Apnea monitor,
without recording
feature
E0619
RR
Apnea monitor, with
recording feature
PA
Maximum of 6 months
rental without PA if criteria
are met. (For more about
criteria, see Apnea monitors
in Coverage Criteria.)
PA required after the initial
6 months.
A4556
NU
Electrodes (e.g.,
Apnea monitor), per
pair
A4558
Purchase only. For use only
when client is unable to
tolerate carbon patch
electrodes.
Limit: 15 pairs every 30
days.
NC
A4557
Lead Wires,
e.g. apnea monitor
per pair
NC
A4558
NU
Conductive paste or
gel
A4556
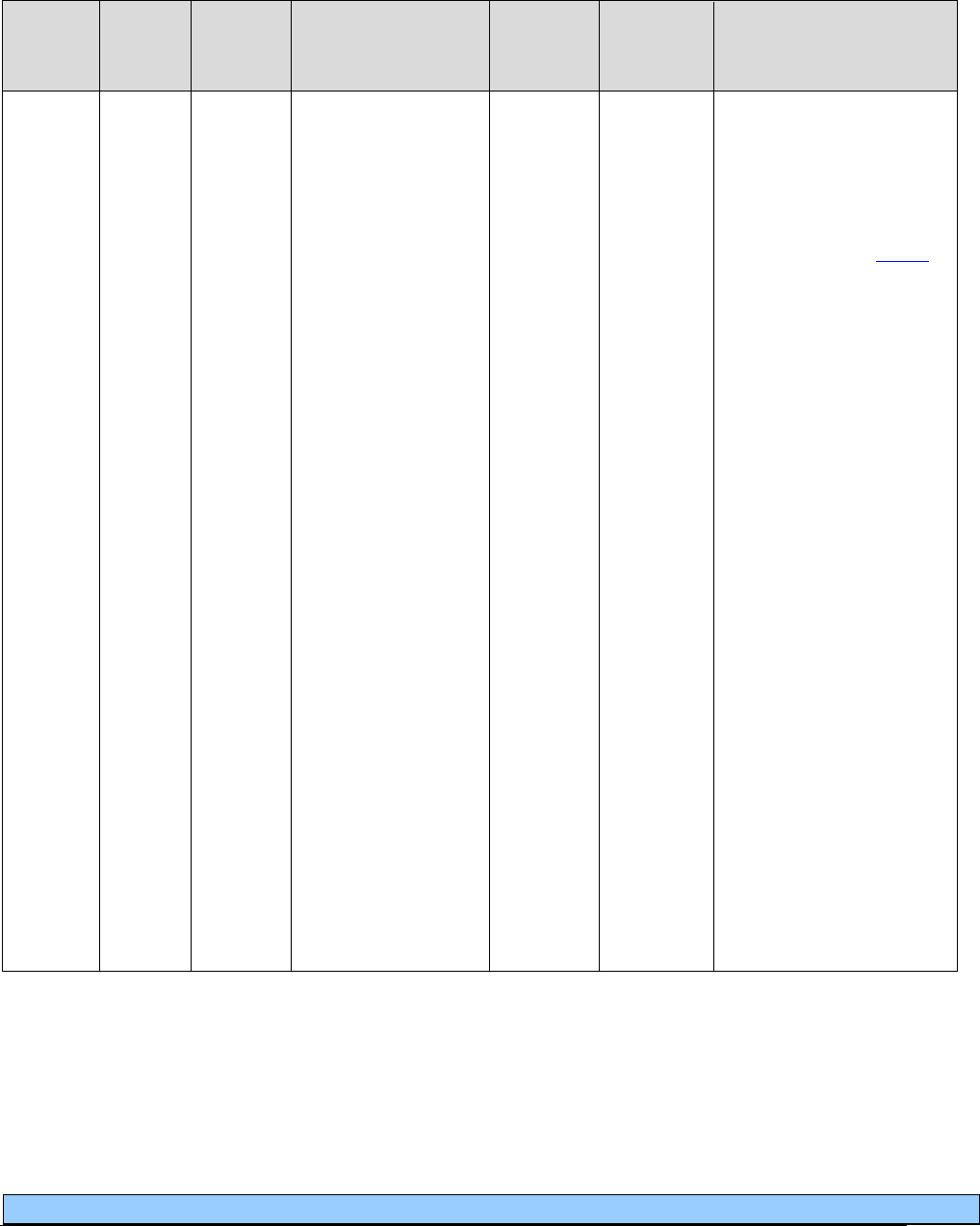
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
49
Continuous positive airway pressure system (CPAP)
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E0601
RR
NU
RA
Continuous airway
pressure (CPAP)
device
E0470
E0471
E0472
Requires results of sleep
study performed in an
agency-approved sleep
center. No PA is required
for rental or purchase if
criteria are met. (For more
about criteria, see
CPAP
in Coverage Criteria.)
Rental limit: 1 unit per
month, maximum of 3-
months mandatory rental.
Limit includes 3-month
rental. If criteria met,
submit for purchase.
Purchase limit: 1 unit per
client, every 5 years.
Purchase price is amount
allowed after 3 months
mandatory rental.
Use of RA modifier – the
RA modifier allows for
the replacement of a
CPAP at the end of the 5-
year limit when the
machine is no longer
functional or cost effective
to repair. This eliminates
the 3-month rental
requirement for this
situation.
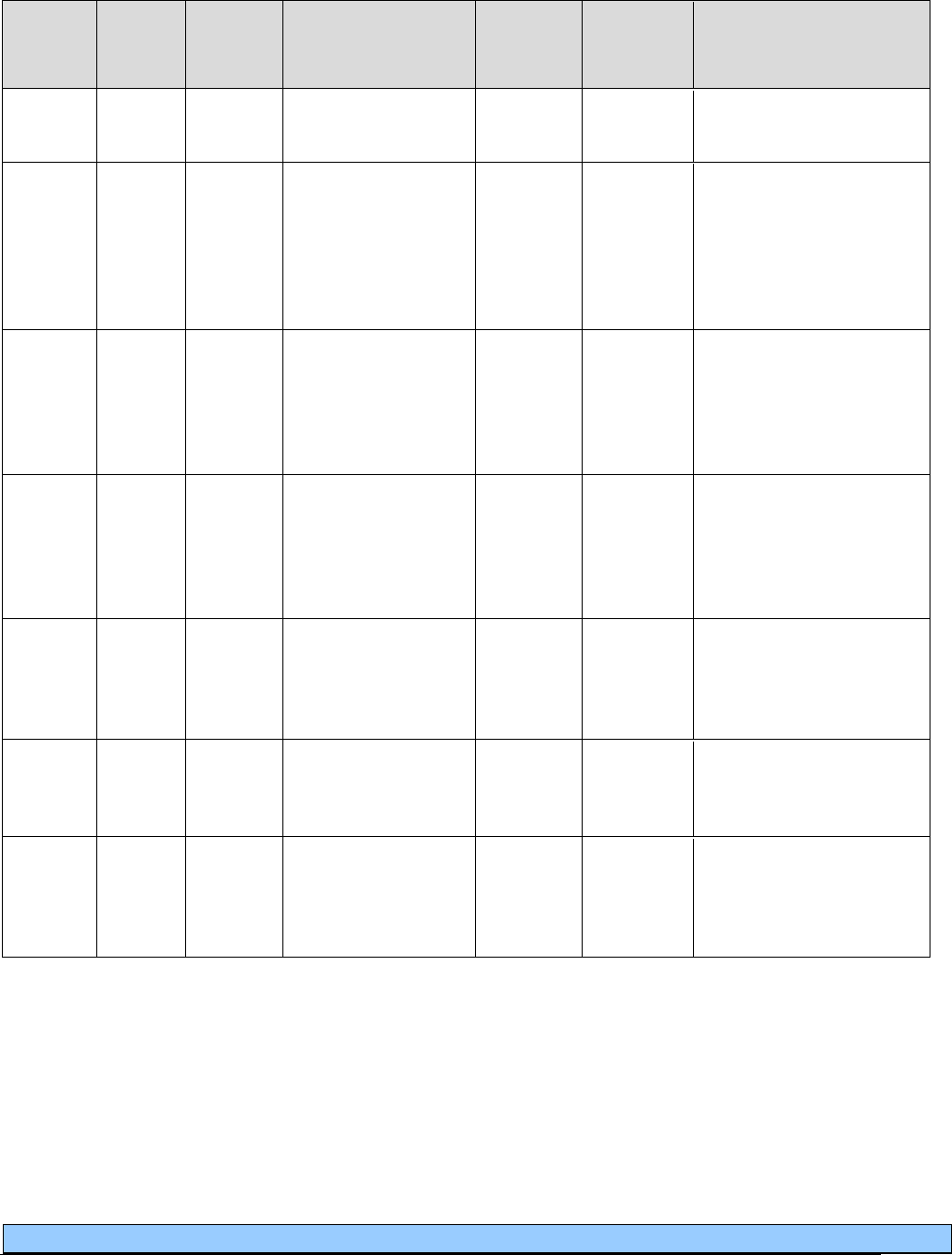
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
50
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
NC
E0605
Vaporizer, Room
Type
A7027
Combination
oral/nasal mask,
used with continuous
positive airway
pressure device,
each
PA
A7028
Oral cushion for
combination
oral/nasal mask,
replacement only,
each
PA
A7029
Nasal pillows for
combination
oral/nasal mask,
replacement only,
pair
PA
A7030
NU
Full face mask, used
with positive airway
pressure device,
each
A7031
Limit: 1 every 6 months.
(Cushion, pillows, and
interface can be replaced
every 3 months.)
A7031
NU
Face mask interface,
replacement for full
face mask, each
A7030
Limit: 1 every 3 months,
not ordered within 3
months of A7030.
A7032
NU
Cushion for use on
nasal mask interface,
replacement only,
each
A7033
A7034
Limit: 1 every 3 months,
not ordered within 3
months of A7034.

Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
51
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
A7033
NU
Pillow for use on
nasal cannula type
interface,
replacement only,
pair
A7032
A7034
Limit: 1 pair every 3
months, not ordered
within 3 months of
A7034.
A7034
NU
Nasal interface
(mask or cannula
type) used with
positive airway
pressure device,
with or without
head strap
A7032
A7033
Limit: 1 every 6 months.
(Cushion and pillows can
be replaced every 3
months.)
A7035
NU
Headgear used with
positive airway
pressure device
Limit: 1 every 6 months.
A7036
NU
Chinstrap used with
positive airway
pressure device
Limit: 1 every 6 months.
A4604
NU
Tubing with
integrated heating
element for use with
positive airway
pressure device
A7010
A7037
Limit: 1 every 6 months.
A7037
NU
Tubing used with
positive airway
pressure device
A7010
A4604
Limit: 1 every 6 months.
A7038
NU
Filter, disposable,
used with positive
airway pressure
device
Limit: 2 every 30 days.
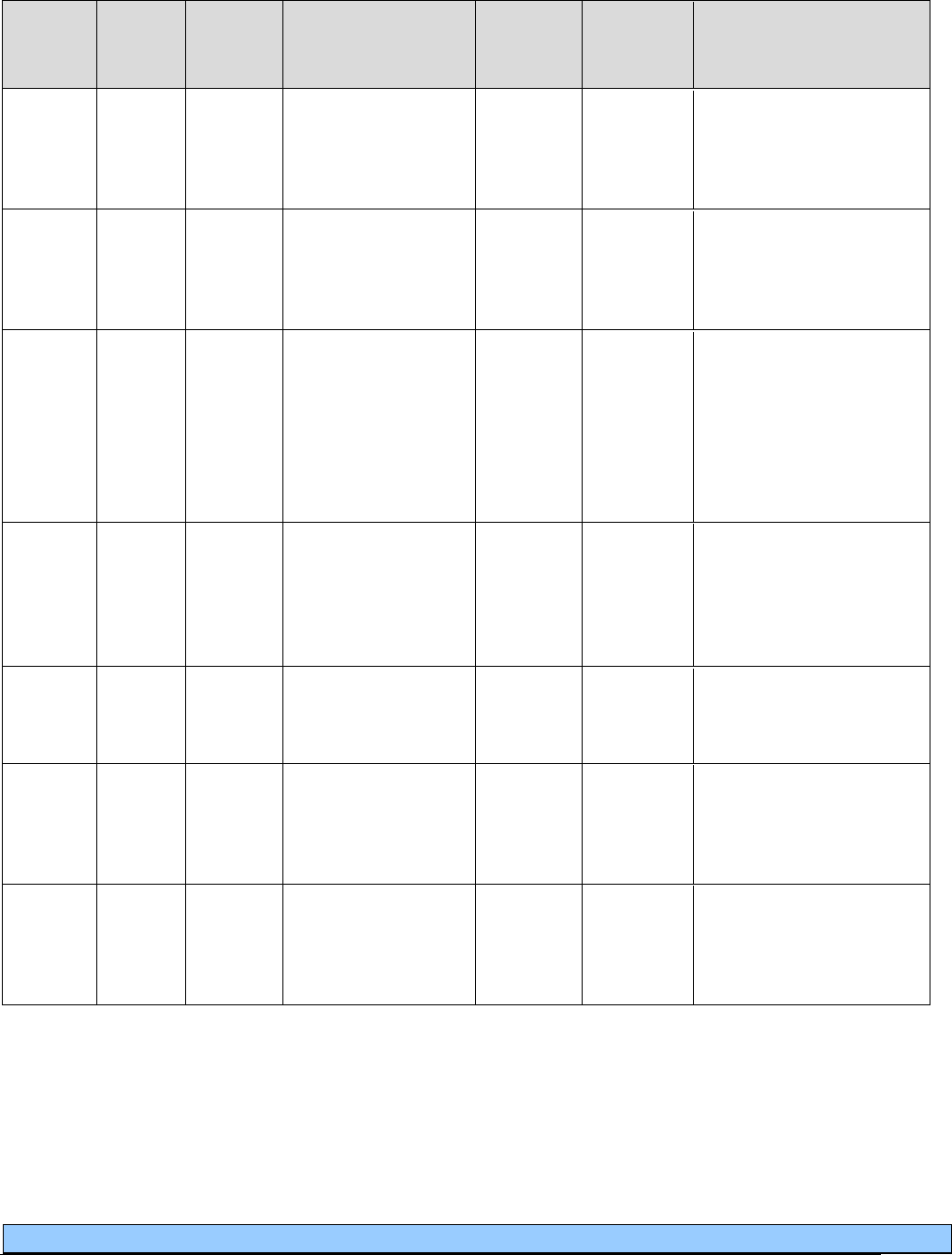
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
52
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
A7039
NU
Filter, non-
disposable, used
with positive airway
pressure device
Limit: 1 every 6 months.
NC
A7044
Oral interface, used
with positive airway
pressure device,
each
NC
A7045
Exhalation port
(with or without
swivel) used with
accessories for
positive airway
devices, replacement
only
A7046
NU
Water chamber for
humidifier, used
with positive airway
pressure device,
replacement, each
Limit: 1 every 6 months.
NC
A7047
Oral interface used
with respiratory
suction pump, each
E0561
NU
Humidifier,
nonheated, used with
positive airway
pressure device
E0562
NU
Humidifier, heated,
used with positive
airway pressure
device
Purchase only.
Limit: 1 per 5 years.
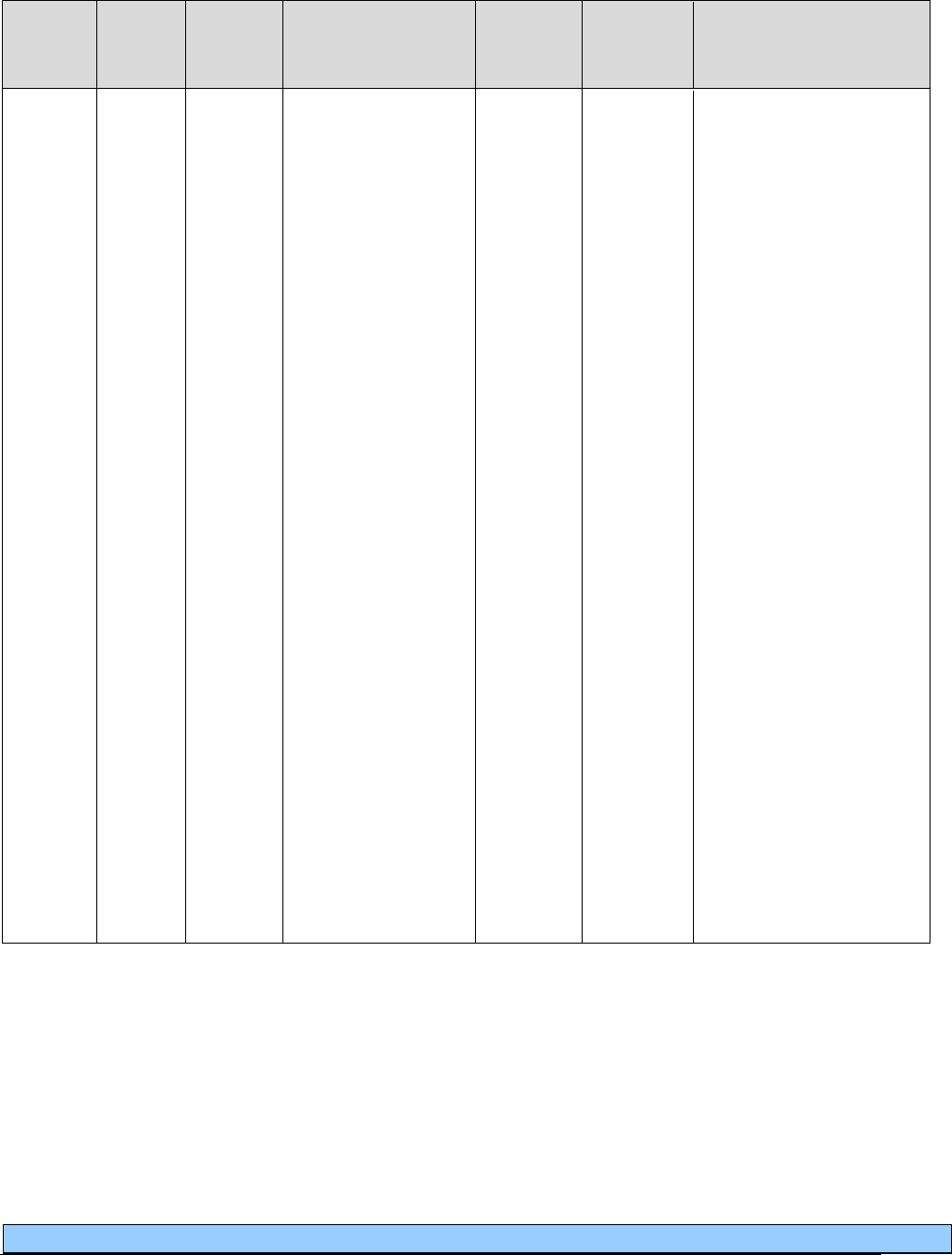
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
53
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E0470
RR
NU
RA
Respiratory assist
device, bi-level
pressure capability,
without backup rate
feature, used with
noninvasive
interface, e.g., nasal
or facial mask
(intermittent assist
device with
continuous positive
airway pressure
device)
E0601
E0471
E0472
PA
PA is
necessary
only if the
client does
not meet
the
Medicare
clinical
criteria; or
if a CPAP
machine
(E0601), or
a BiPAP
machine
(E0470)
has been
purchased
within the
last 5
years.
(Example: BiPAP S)
Requires results of sleep
study performed in an
agency-approved sleep
center when prescribed for
sleep apnea.
Purchase required after
maximum of 3 months
mandatory rental. Client
compliance and
effectiveness must be
documented prior to
purchase. Purchase price is
amount allowed after 3
months mandatory rental.
Limit includes 3-month
rental. If criteria are met,
submit for a purchase.
Purchase limit: 1 unit per
client, every 5 years.
RA modifier allows for
the replacement of a
BiPAP at the end of the 5-
year limit when the
machine is no longer
functional or cost effective
to repair. This eliminates
the 3-month rental
requirement for this
situation.
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
54
IPPB machine and accessories
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
NC
E0500
RR
IPPB machine, all
types, with built-in
nebulization; manual
or automatic valves;
internal or external
power source (includes
mouthpiece and
tubing)
E0570
Nebulizers and accessories
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E0565
RR
Compressor, air
power source for
equipment which is
not self-contained or
cylinder driven
Rental for 13 months,
then considered
purchased.
Limit: 1 per client
every 5 years.
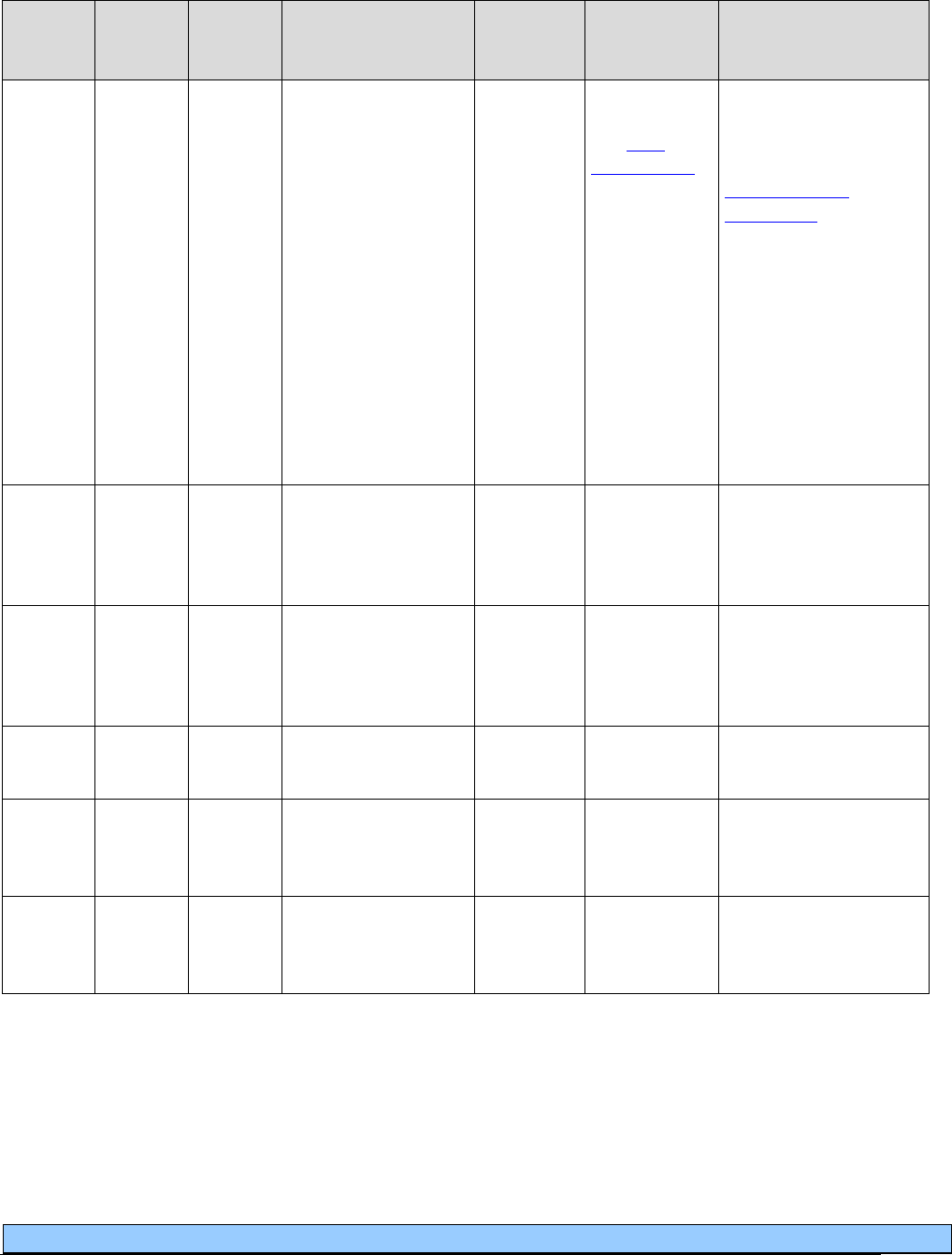
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
55
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E0570
NU
Nebulizer with
compressor
A4619
A4217
A7007
A7010
A7012
A7014
A7018
E0500
EPA
See EPA
criteria table
for clients not
meeting
clinical
criteria.
PA not required if
client meets clinical
criteria. (For more
about criteria, see
Nebulizers and
accessories in Coverage
Criteria.)
Limit: 1 per client,
every 5 years.
AC/DC adapters used
with this equipment are
considered included in
nebulizer
reimbursement.
NC
E0572
Aerosol compressor,
adjustable pressure,
light duty for
intermittent use
NC
E0574
Ultrasonic/electronic
aerosol generator
with small volume
nebulizer
NC
E0575
Nebulizer ultrasonic,
large volume
NC
E0580
Nebulizer, with
compressor and
heater
NC
E0585
Nebulizer, with
compressor and
heater
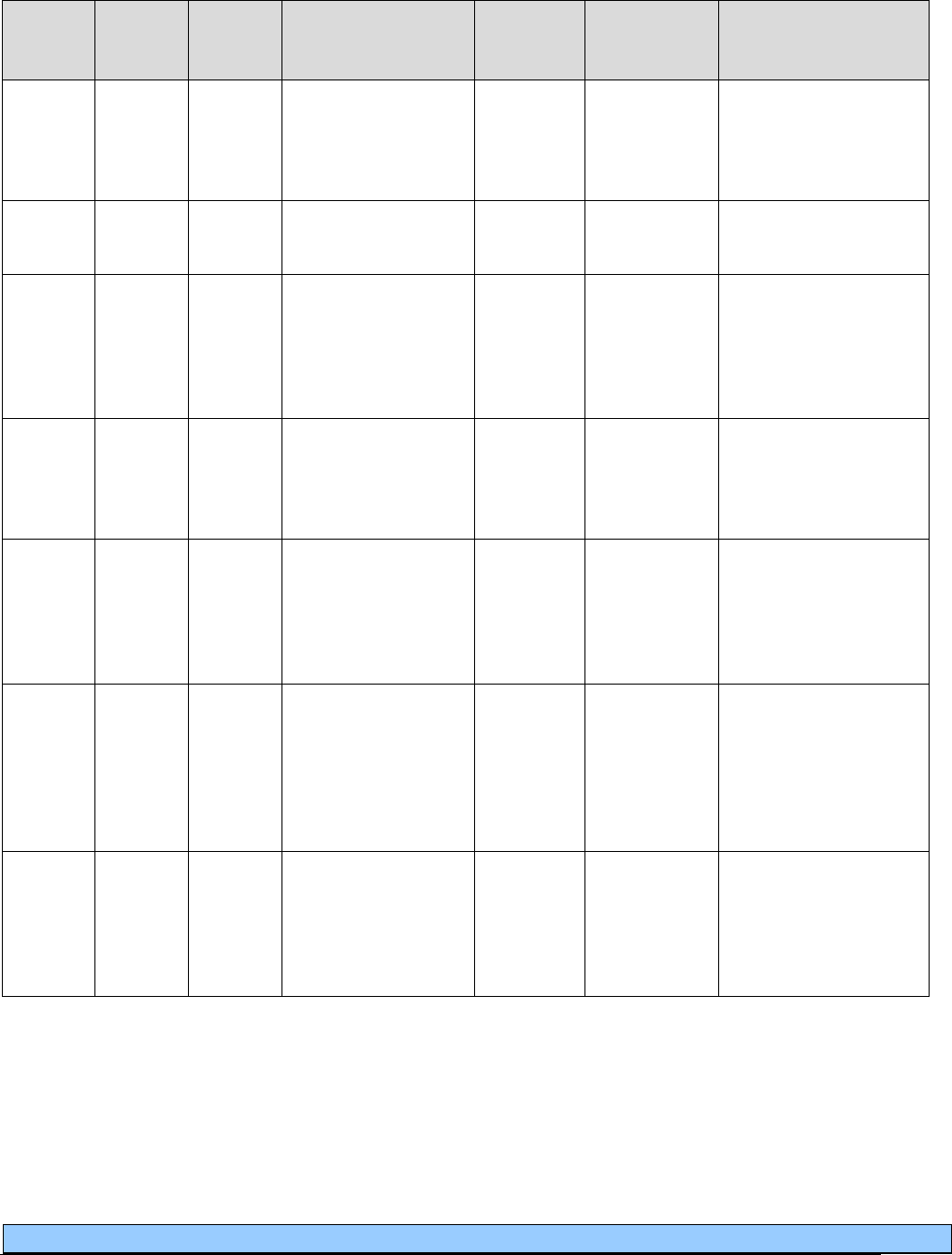
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
56
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E1352
Oxygen accessory,
flow regulator
capable of positive
inspiratory pressure
E1372
Immersion external
heater for nebulizer
PA
A7003
NU
Administration set,
with small volume
non-filtered
pneumatic nebulizer,
disposable
Purchase only.
Limit: 1 per client,
every 30 days.
A7004
NU
Small volume
nonfiltered
pneumatic nebulizer,
disposable
A7005
Purchase only.
Limit: 2 per client,
every 30 days.
A7005
NU
Administration set,
with small volume
non-filtered
pneumatic nebulizer,
non-disposable
A7004
Purchase only.
Limit: 1 per client,
every 6 months.
A7006
NU
Administration set,
with small volume
filtered pneumatic
nebulizer.
Purchase only.
Limit: 1 per client,
every 30 days.
For Pentamidine
administration only.
A7007
NU
Large volume
nebulizer,
disposable, unfilled,
used with aerosol
compressor
E0570
Limit: 10 per client,
every 30 days.
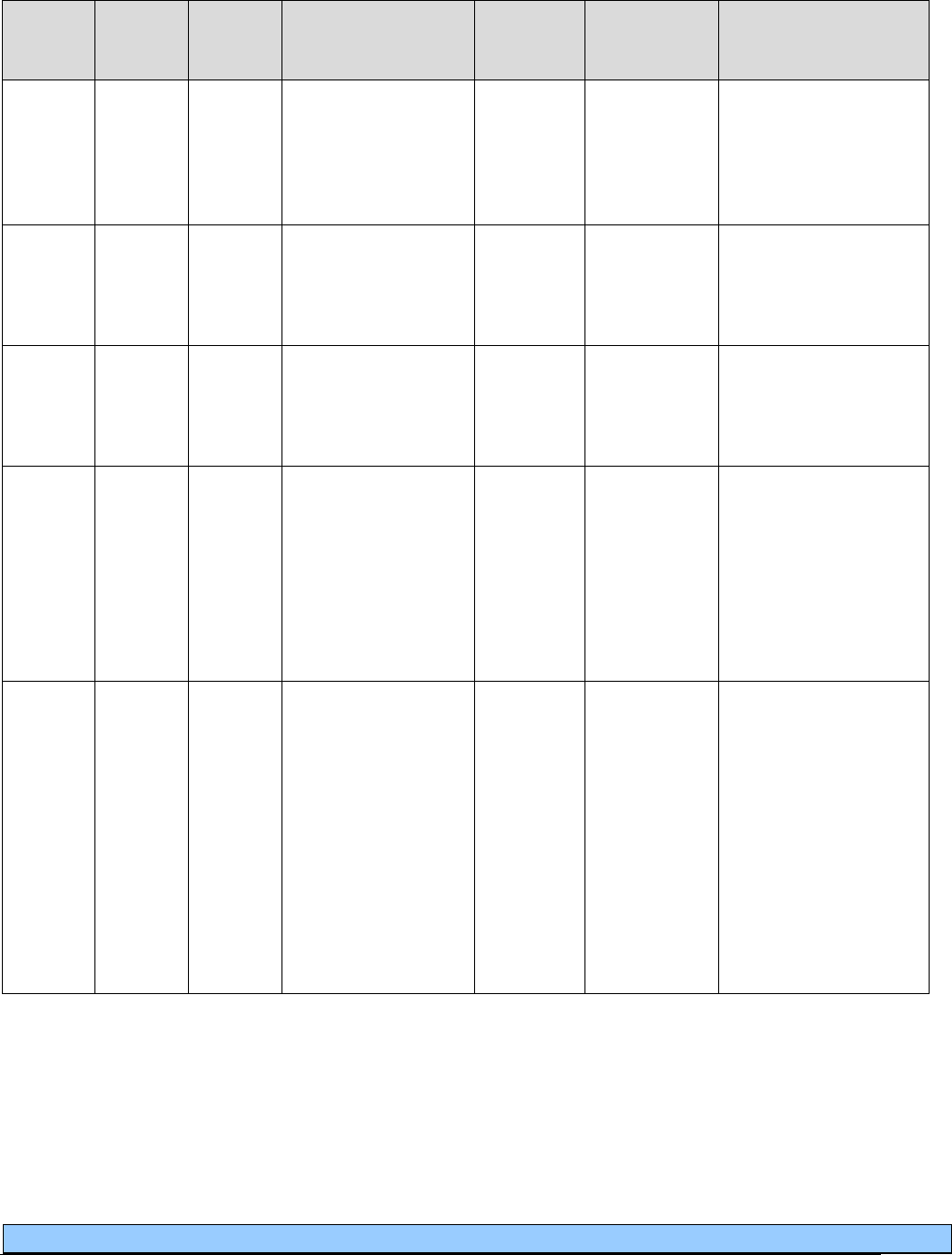
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
57
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
NC
A7008
Large volume
nebulizer,
disposable, prefilled,
used with aerosol
compressor
NC
A7009
Reservoir bottle,
non-disposable, used
with large volume
ultrasonic nebulizer
A7010
NU
Corrugated tubing,
disposable, used
with large volume
nebulizer, 100 feet
A7037
A4604
E0570
Purchase only.
Limit: 1 unit per client,
every 60 days.
A7012
NU
Water collection
device, used with
large volume
nebulizer (e.g.,
aerosol drainage
bag)
E0570
Only paid in
conjunction with
E0565. Must bill on
same claim with
E0565.
Purchase only.
Limit: 8 per client,
every 30 days.
A7013
NU
Filter, disposable,
used with aerosol
compressor
A7014
For use with E0570 or
E0565.
Purchase only.
Limit: 2 per client,
every 30 days.
A7014
NU
Filter, non-
disposable, used
with aerosol
compressor or
ultrasonic generator
A7013
E0570
Only when using
E0565. Must bill on
same claim with
E0565. Purchase only.
Limit: 1 per client,
every 90 days.
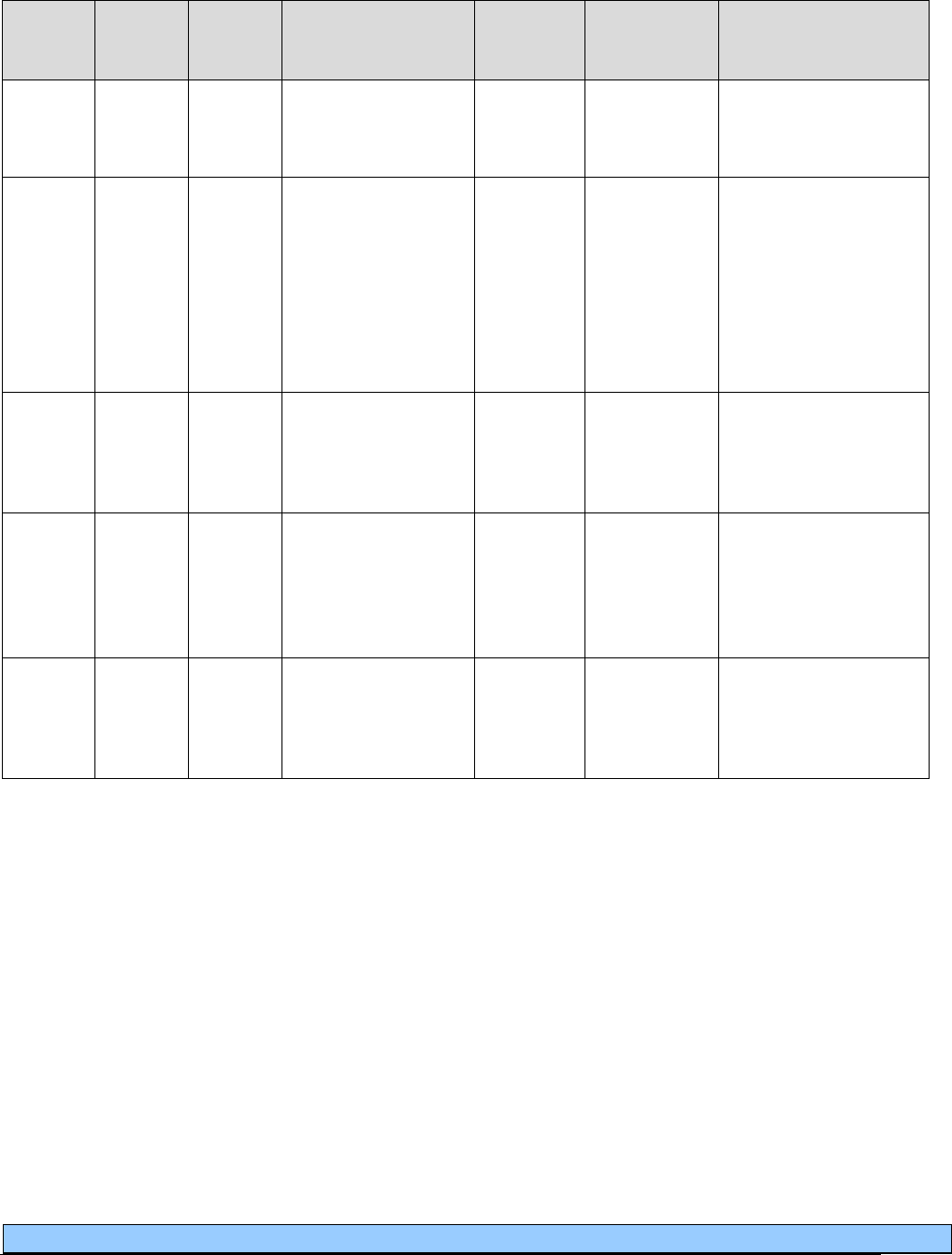
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
58
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
A7015
NU
Aerosol mask, used
with DME nebulizer
Purchase only.
Limit: 1 per client,
every 30 days.
A4619
NU
Face tent
E0424
E0431
E0434
E0439
E0570
E1390
E1392
K0738
Purchase only.
Limit: 1 per client,
every 30 days.
NC
A7016
Dome and mouth
piece, used with
small volume
ultrasonic nebulizer
NC
A7017
Nebulizer, durable,
glass or autoclavable
plastic, bottle type,
not used with
oxygen
A7018
NU
Water, distilled,
used with large
volume nebulizer,
1000 ml
E0570
A4217
Limit is 50 units, per
client, every 30 days.
1 unit = 1000ml.
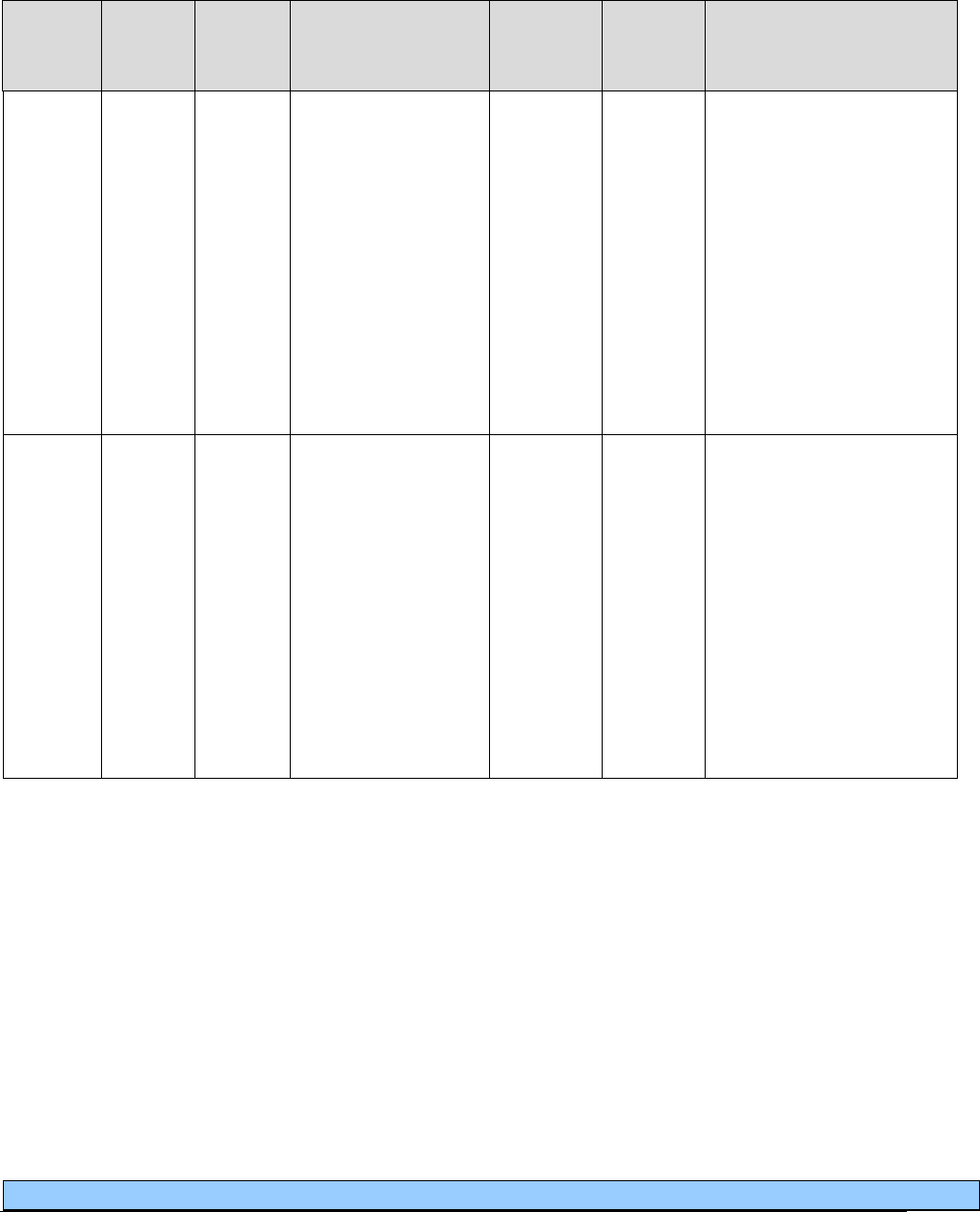
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
59
Oxygen and oxygen equipment
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
A4615
NU
Cannula, nasal
E0424
E0431
E0434
E0439
E1390
E1392
K0738
May only be billed for
client-owned equipment or
following the 36-month
capped rental period until
the end of the 5-year
lifetime for the following
equipment : E0424,
E0431, E0434, E0439,
E1390, E1392, and
K0738.
Limit: 2 per client, every
30 days.
A4616
NU
Tubing (oxygen), per
foot
E0424
E0431
E0434
E0439
E0471
E0472
E1390
E1392
K0738
May only be billed for
client-owned equipment or
following the 36-month
capped rental period until
the end of the 5-year
lifetime for the following
equipment : E0424,
E0431, E0434, E0439,
E1390, E1392, and
K0738.
Limit: 1 tube per client,
every 30 days.
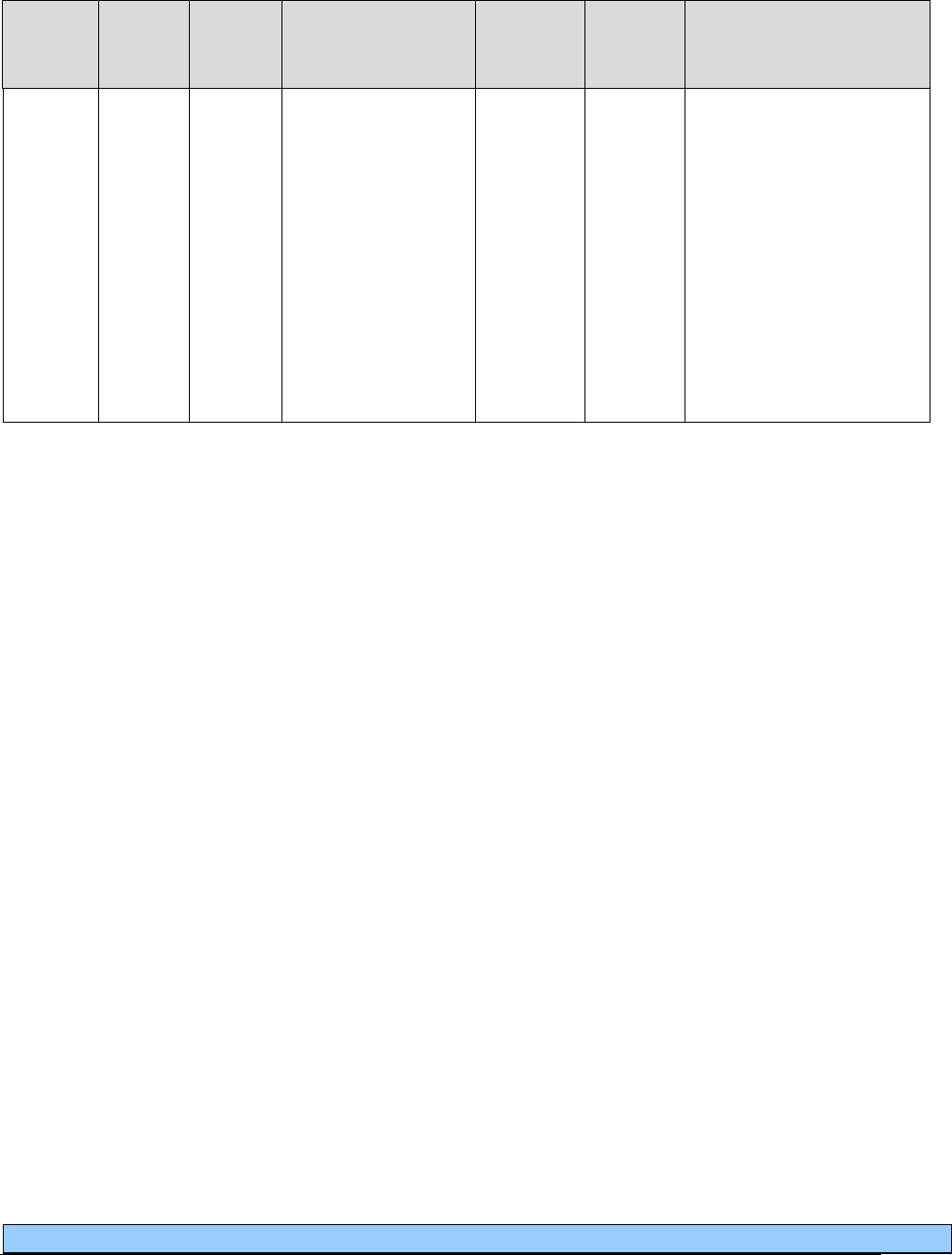
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
60
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
A4620
NU
Variable
concentration mask
E0424
E0431
E0434
E0439
E1390
E1392
K0738
May only be billed for
client-owned equipment or
following the 36-month
capped rental period until
the end of the 5-year
lifetime for the following
equipment : E0424,
E0431, E0434, E0439,
E1390, E1392, and
K0738.
Limit: 2 per client, every
30 days.
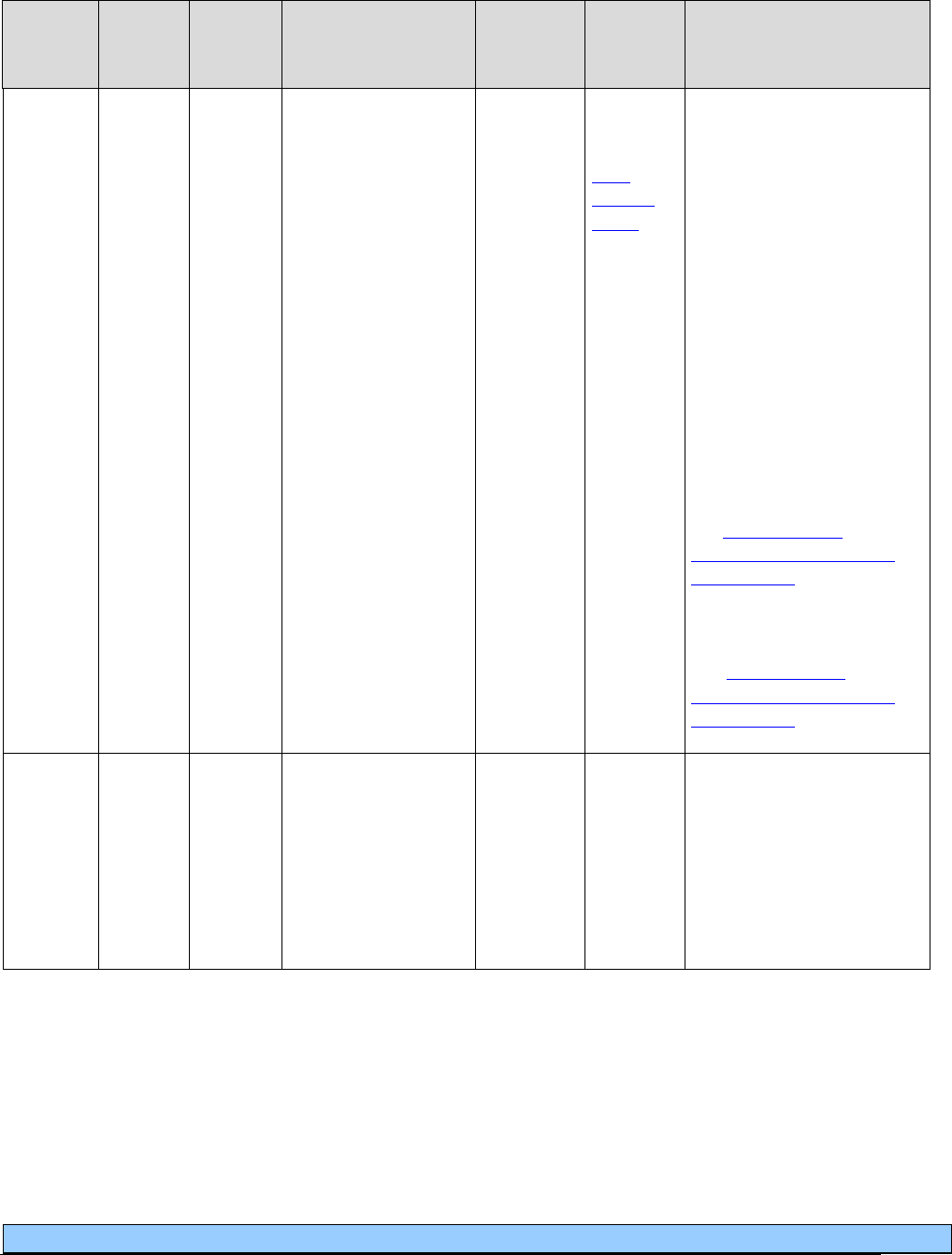
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
61
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E0424
RR
MS
QA**
QB**
QR**
QE**
QF**
QG**
Stationary
compressed gaseous
oxygen system,
rental; includes
container, contents,
regulator, flowmeter,
humidifier, nebulizer,
cannula or mask, and
tubing
A4615-
A4620
E0439
E0441-
E0444
E1390
E1392
EPA
See the
EPA
Criteria
Table for
criteria
to restart
the 36-
month
capped
rental
period.
Limit: 1 per client, every
30 days, for a maximum
reimbursed period of 36
months.
Following the capped
rental period, the same
vendor continues to be
responsible for the
equipment and provision
of oxygen services to the
client until the 5-year
reasonable, useful lifetime
of the equipment has been
met.
For maintenance and
capped rental information,
see Stationary and
portable oxygen systems
and contents.
**Modifiers are based on
liters per minute (LPM).
See Stationary and
portable oxygen systems
and contents.
NC
E0425
Stationary
compressed gas
system, purchase:
includes regulator,
flowmeter,
humidifier, nebuliz
er,
cannula or mask, and
tubing
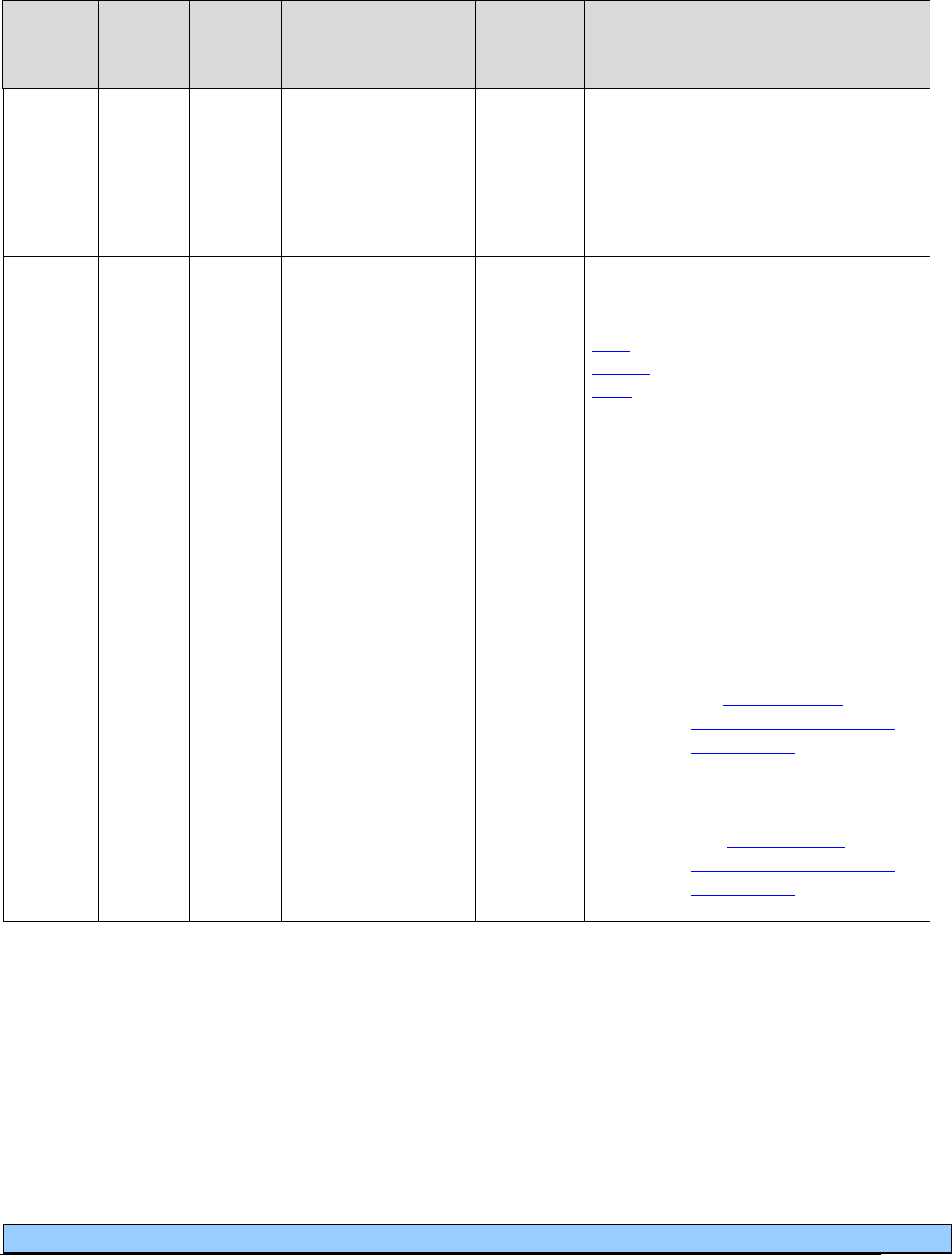
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
62
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
NC
E0430
Portable gaseous
oxygen system,
purchase; includes
regulator, flowmeter,
humidifier, cannula
or mask, and tubing
E0431
RR
MS
QA**
QB**
QR**
QE**
QF**
QG**
Portable gaseous
oxygen system,
rental; includes
portable container,
regulator, flowmeter,
humidifier, cannula
or mask, and tubing
A4615-
A4620
E0434
E0441-
E0444
K0738
EPA
See the
EPA
criteria
table for
criteria
to restart
the 36-
month
capped
rental
period.
Limit: 1 per client, every
30 days, for a maximum
reimbursed period of 36
months.
Following the capped
rental period, the same
vendor continues to be
responsible for the
equipment and provision
of oxygen services to the
client until the 5-year
reasonable, useful lifetime
of the equipment has been
met.
For maintenance and
capped rental information,
see
Stationary and
portable oxygen systems
and contents.
**Modifiers are based on
liters per minute (LPM).
See
Stationary and
portable oxygen systems
and contents.
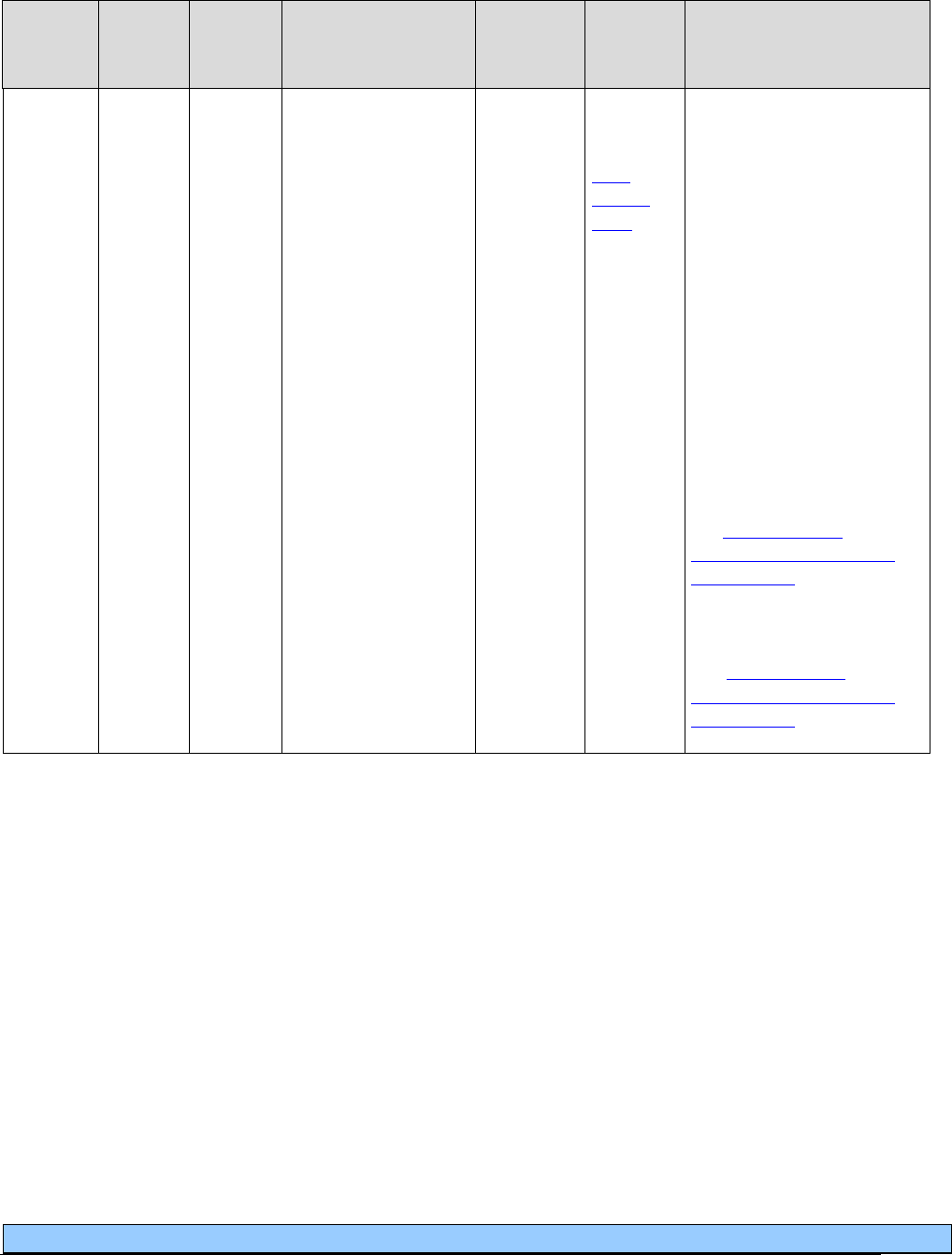
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
63
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
K0738
RR
MS
QA**
QB**
QR**
QE**
QF**
QG**
Portable gaseous
oxygen system,
rental; home
compressor used to
fill portable oxygen
cylinders; includes
portable containers,
regulator, flowmeter,
humidifier, cannula
or mask and tubing
A4615-
A4620
E0431
E0434
E0441-
E0444
EPA
See the
EPA
criteria
table for
criteria
to restart
the 36-
month
capped
rental
period.
Limit: 1 per client, every
30 days, for a maximum
reimbursed period of 36
months.
Following the capped
rental period, the same
vendor continues to be
responsible for the
equipment and provision
of oxygen services to the
client until the 5-year
reasonable, useful lifetime
of the equipment has been
met.
For maintenance and
capped rental information,
see
Stationary and
portable oxygen systems
and contents.
**Modifiers are based on
liters per minute (LPM).
See
Stationary and
portable oxygen systems
and contents.
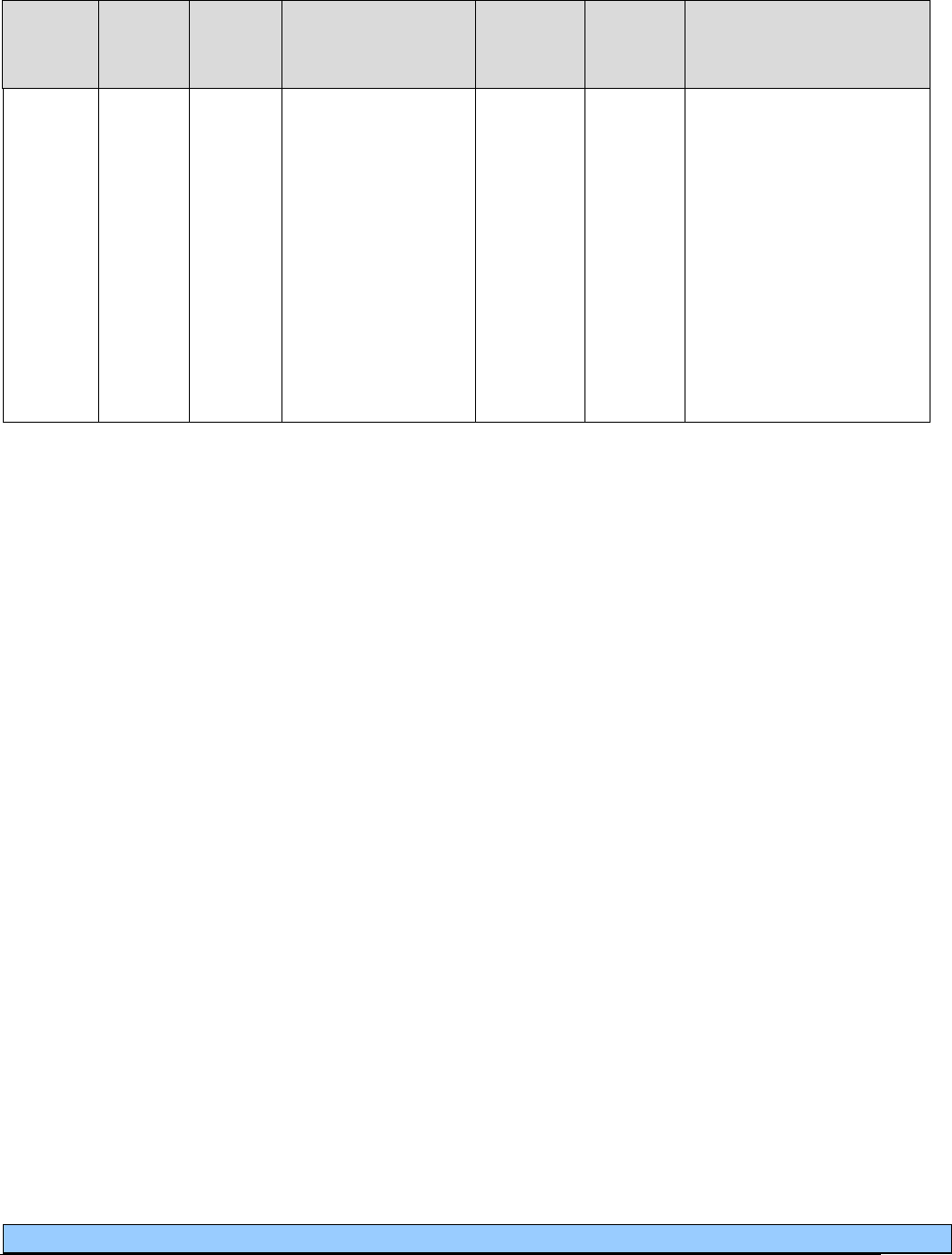
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
64
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
NC
E0433
Portable liquid
oxygen system,
rental; home liquefier
used to fill portable
liquid oxygen
containers, includes
portable containers,
regulator, flowmeter,
humidifier, cannula or
mask and tubing, with
or without supply
reservoir and
contents
gauge
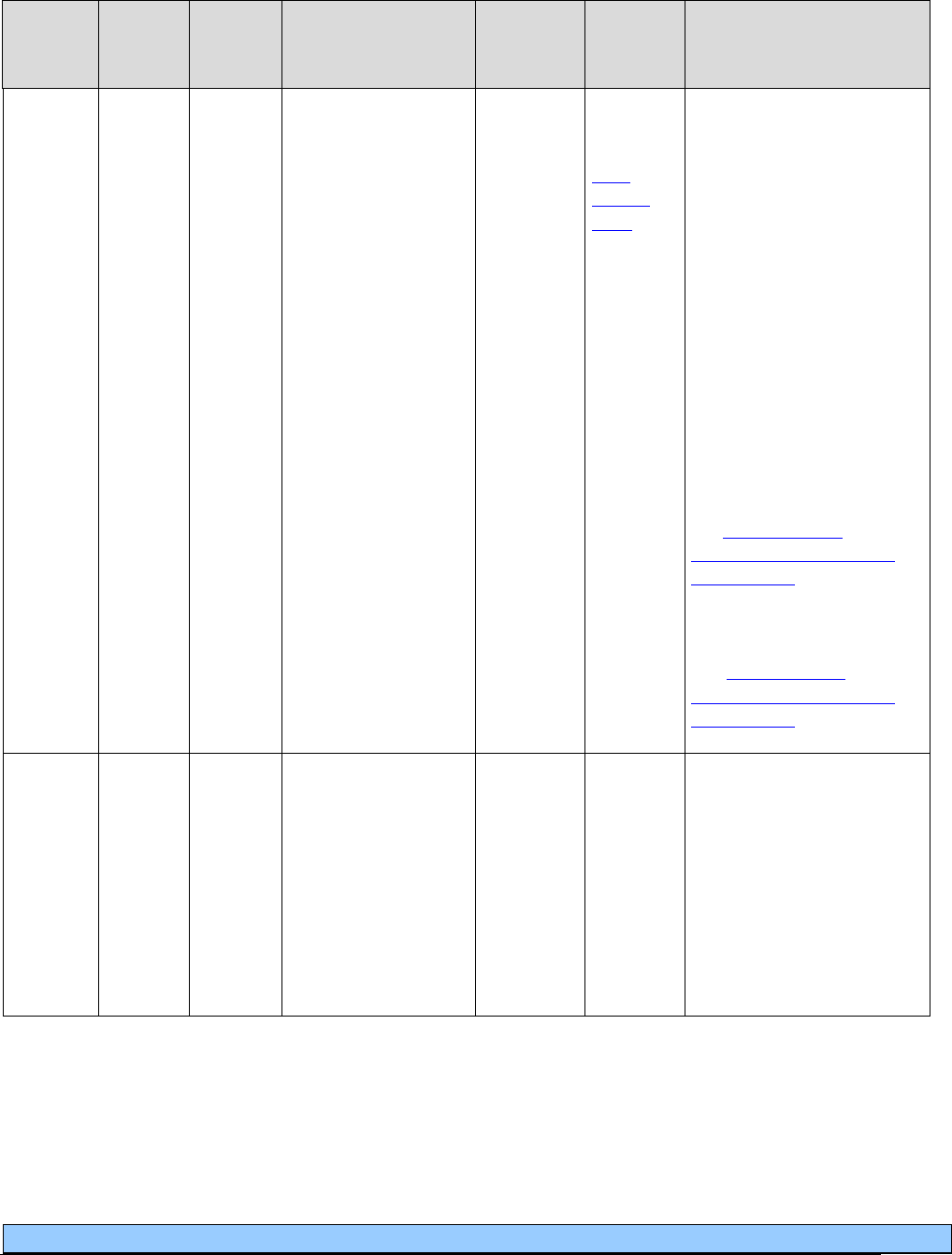
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
65
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E0434
RR
MS
QA**
QB**
QR**
QE**
QF**
QG**
Portable liquid
oxygen system,
rental; includes
portable container,
supply reservoir,
humidifier,
flowmeter, refill
adapter, contents,
gauge, cannula or
mask and tubing
A4615-
A4620
E0431
E0441-
E0444
E1392
K0738
EPA
See the
EPA
criteria
table for
criteria
to restart
the 36-
month
capped
rental
period.
Limit: 1 per client, every
30 days, for a maximum
reimbursed period of 36
months.
Following the capped
rental period, the same
vendor continues to be
responsible for the
equipment and provision
of oxygen services to the
client until the 5-year
reasonable, useful lifetime
of the equipment has been
met.
For maintenance and
capped rental information,
see Stationary and
portable oxygen systems
and contents.
**Modifiers are based on
liters per minute (LPM).
See Stationary and
portable oxygen systems
and contents.
NC
E0435
Portable liquid
oxygen system,
purchase: includes
portable container,
supply reservoir,
humidifier,
flowmeter, contents
gauge, cannula or
mask, tubing, and
refill adapter
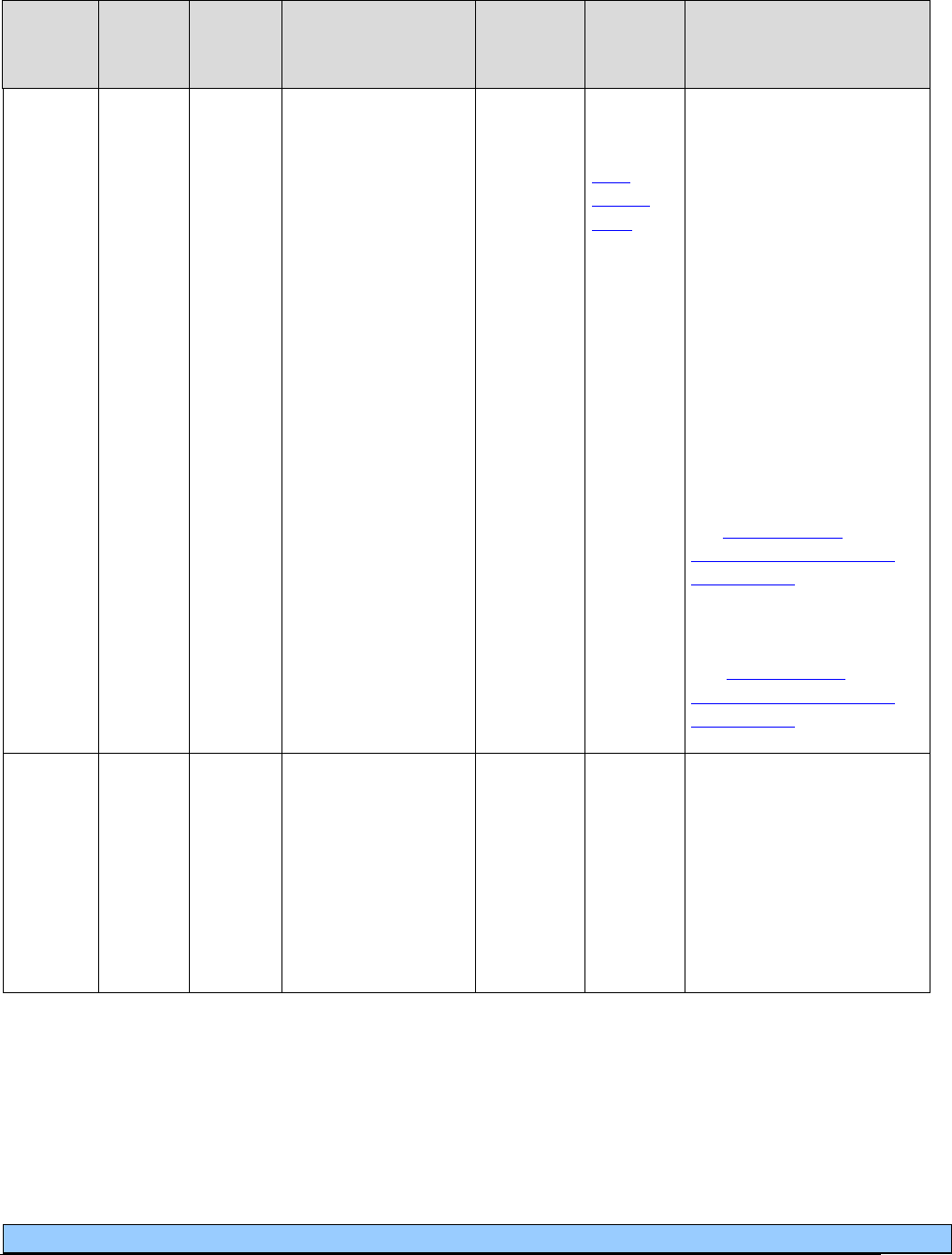
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
66
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E0439
RR
MS
QA**
QB**
QR**
QE**
QF**
QG**
Stationary liquid
oxygen system,
rental; includes
container, contents,
regulator, flowmeter,
humidifier, nebuliz
er,
cannula or mask, and
tubing
A4615-
A4620
E0424
E0441-
E0444
E1390
E1392
EPA
See the
EPA
criteria
table for
criteria
to restart
the 36-
month
capped
rental
period.
Limit: 1 per client, every
30 days, for a maximum
reimbursed period of 36
months.
Following the capped
rental period, the same
vendor continues to be
responsible for the
equipment and provision
of oxygen services to the
client until the 5-year
reasonable, useful lifetime
of the equipment has been
met.
For maintenance and
capped rental information,
see
Stationary and
portable oxygen systems
and contents.
**Modifiers are based on
liters per minute (LPM).
See
Stationary and
portable oxygen systems
and contents.
NC
E0440
Stationary liquid
oxygen system,
purchase; includes
use of reservoir,
contains indicator,
regulator, flowmeter,
humidifier, nebuliz
er,
cannula or mask, and
tubing

Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
67
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E0441
NU
Stationary oxygen
contents, gaseous.
One month’s supply
equals one unit.
E0424
E0431
E0434
E0439
E0442
E0443
E0444
E1390
E1392
K0738
Limit: 1 per client, every
30 days.
30-day supply equals one
unit.
Providers may bill this
code for the 24 months
following a 36 month
capped rental period, or if
the client owns the oxygen
equipment. Provider needs
to add comment on the
claim as to which criteria
have been met.
E0442
NU
Stationary oxygen
contents, liquid). One
month’s supply
equals one unit
E0424
E0431
E0434
E0439
E0441
E0443
E0444
E1390
E1392
K0738
Limit: 1 per client, every
30 days.
30-day supply equals one
unit.
Providers may bill this
code for the 24 months
following a 36 month
capped rental period, or if
the client owns the oxygen
equipment. Provider needs
to add comment on the
claim as to which criteria
have been met.
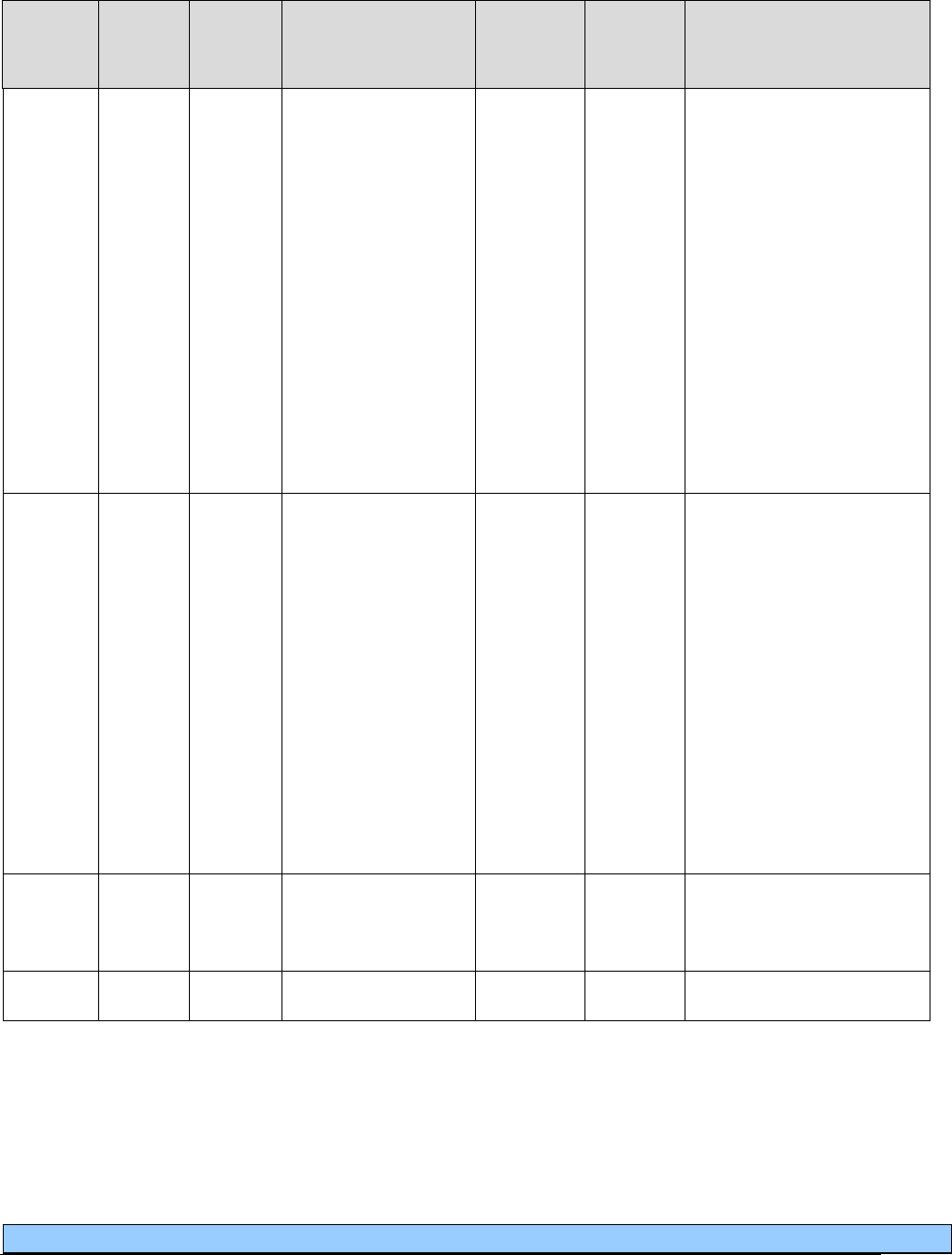
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
68
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E0443
NU
Portable oxygen
contents, gaseous.
One month’s supply
equals one unit
E0424
E0431
E0434
E0439
E0441
E0442
E0444
E1390
E1392
K0738
Limit: 1 per client, every
30 days for client-owned
equipment.
30-day supply equals one
unit.
Providers may bill this
code for the 24 months
following a 36 month
capped rental period, or if
the client owns the oxygen
equipment Provider needs
to add comment on the
claim as to which criteria
have been met.
E0444
NU
Portable oxygen
contents, liquid. One
month’s supply
equals one unit
E0424
E0431
E0434
E0439
E0441
E0443
E1390
E1392
K0738
Limit: 1 per client, every
30 days.
30-day supply equals one
unit.
Providers may bill this
code for the 24 months
following a 36 month
capped rental period, or if
the client owns the oxygen
equipment. Provider needs
to add comment on the
claim as to which criteria
have been met.
NC
E0455
Oxygen tent,
excluding croup or
pediatric tents
NC
E0457
Chest Sll (Cuirass)
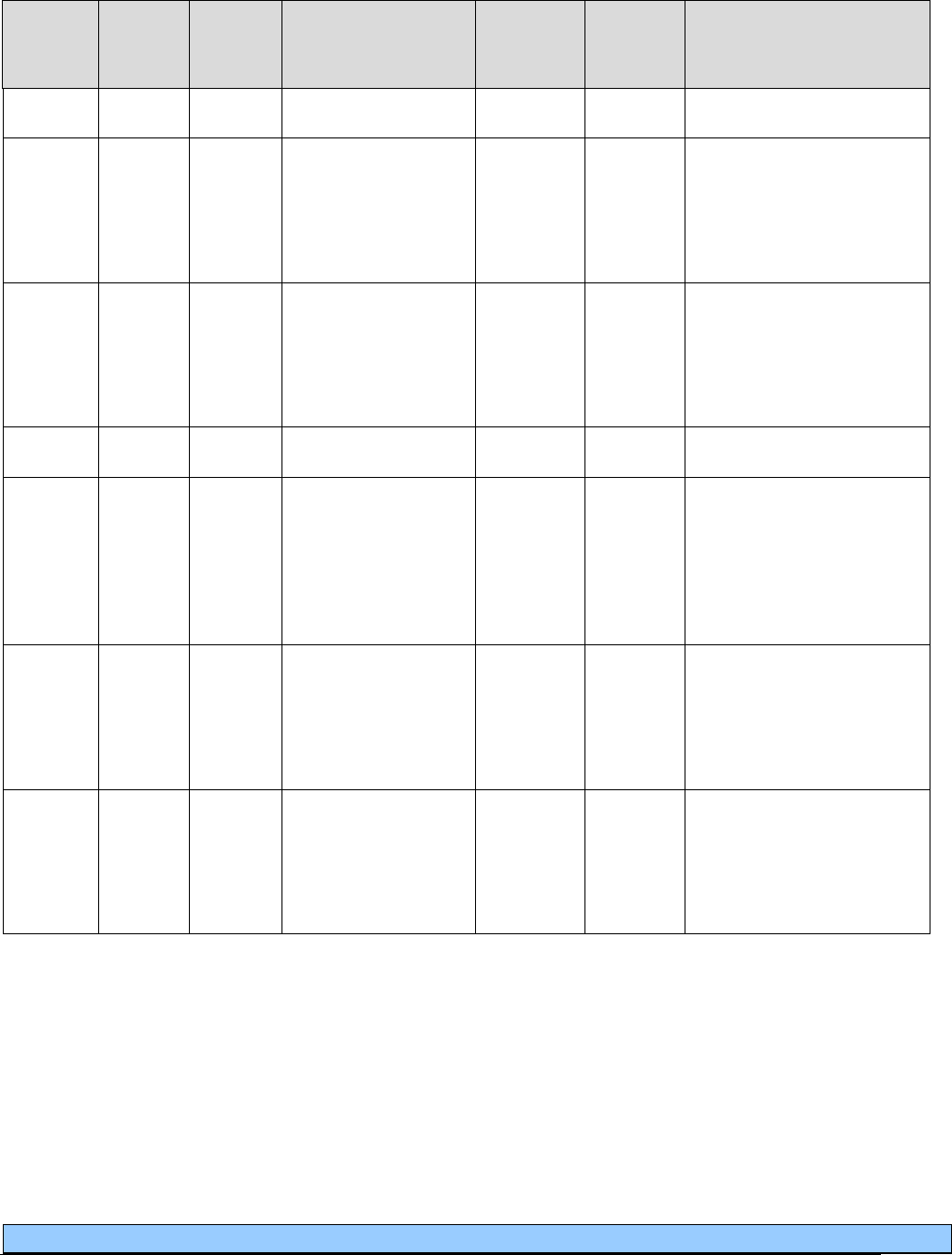
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
69
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
NC
E0459
Chest wrap
NC
E0446
Topical oxygen
delivery system, not
otherwise specified,
includes all supplies
and accessories
NC
E1354
Oxygen accessory,
wheeled cart for
portable cylinder
or portable
concentrator
NC
E1355
Stand/rack
NC
E1356
Oxygen accessory,
battery
pack/cartridge for
portable
concentrator, any
type
NC
E1357
Oxygen accessory,
battery charger for
portable
concentrator, any
type
NC
E1358
Oxygen accessory,
DC power adapter
for portable
concentrator, any
type
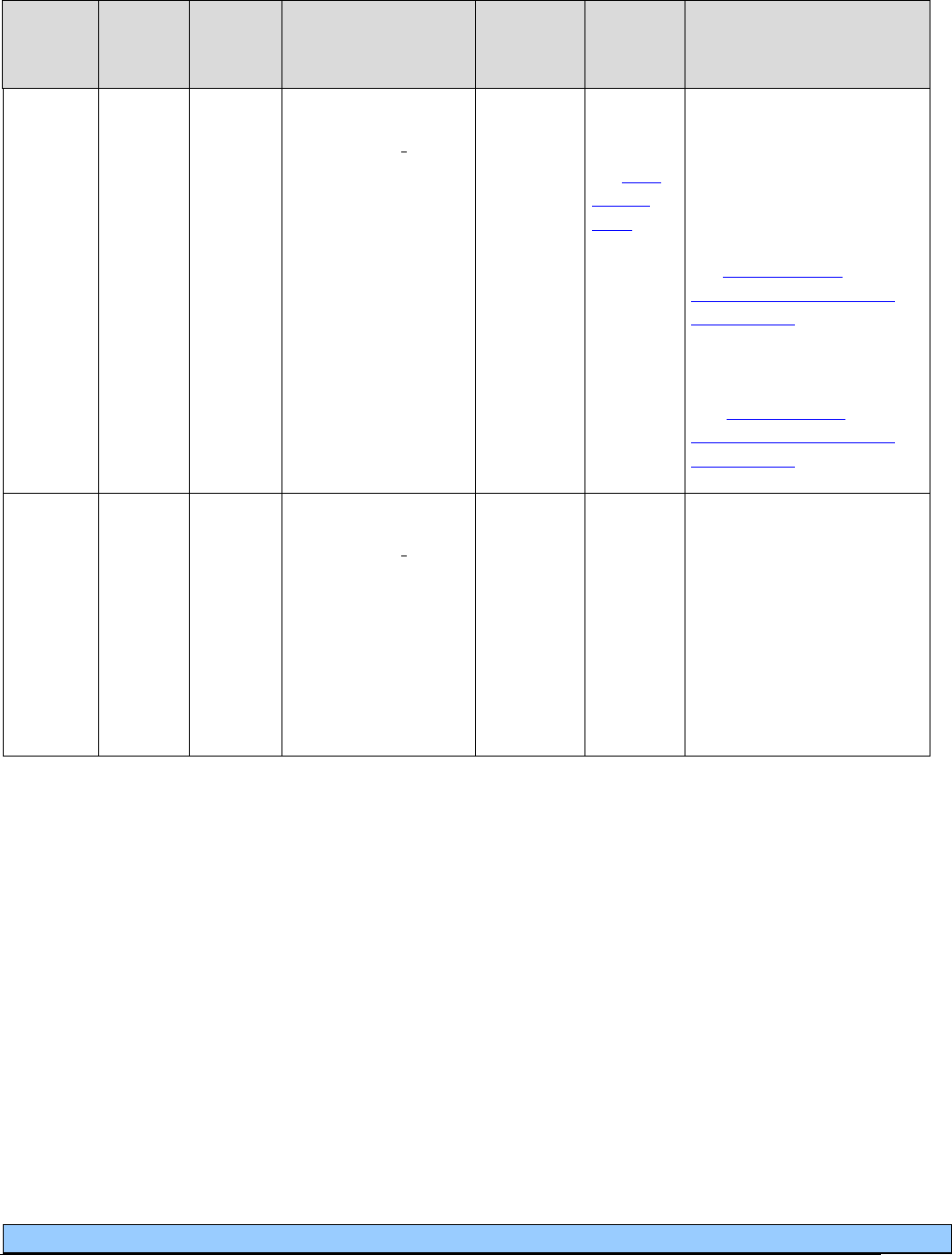
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
70
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E1390
RR
MS
QA**
QB**
QR**
QE**
QF**
QG**
Oxygen
concentrator, single
delivery port,
capable of
delivering 85
percent or greater
oxygen
concentration at the
prescribed flow
A4615-
A4620
E0424
E0439
E0441
E0442
E0443
E0444
EPA
Refer to
the
EPA
criteria
table for
criteria to
restart the
36-month
capped
rental
period.
Limit: 1 per client, every
30 days, for a maximum
reimbursed period of 36
months.
For maintenance and
capped rental information,
see
Stationary and
portable oxygen systems
and contents.
**Modifiers are based on
liters per minute (LPM).
See
Stationary and
portable oxygen systems
and contents.
NC
E1391
Oxygen
concentrator, dual
delivery port,
capable of
delivering 85
percent or greater
oxygen
concentration at the
prescribed flow rate,
each
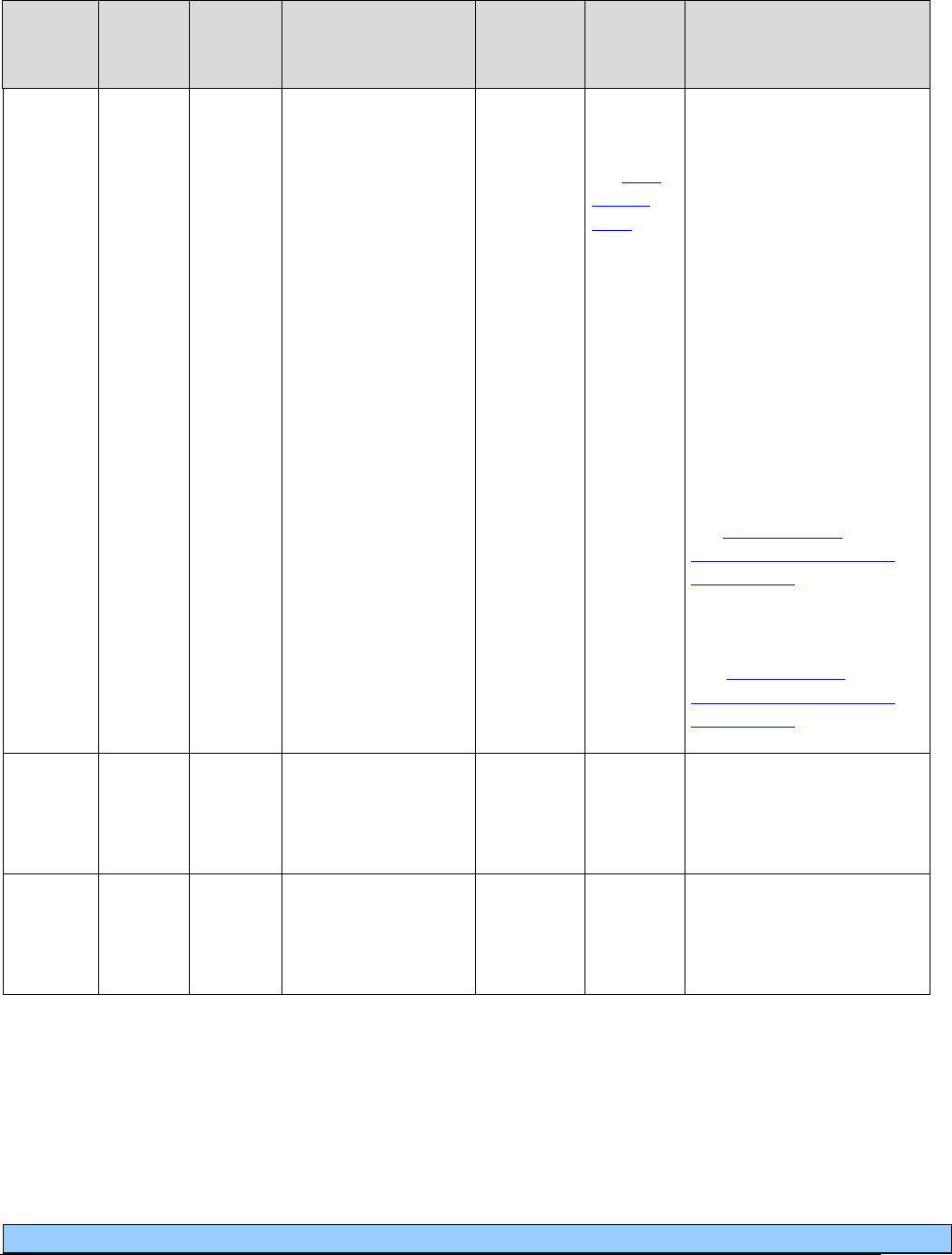
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
71
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
E1392
RR
MS
QA**
QB**
QR**
QE**
QF**
QG**
Portable oxygen
concentrator, rental.
A4615-
A4620
E0424
E0431
E0434
E0439
E0441
E0442
E0443
E0444
EPA
Refer to
the
EPA
criteria
table for
criteria to
restart the
36-month
capped
rental
period.
Limit: 1 per client, every
30 days, for a maximum
reimbursed period of 36
months.
Following the capped
rental period, the same
vendor continues to be
responsible for the
equipment and provision
of oxygen services to the
client until the 5-year
reasonable, useful lifetime
of the equipment has been
met.
For maintenance and
capped rental information,
see
Stationary and
portable oxygen systems
and contents.
**Modifiers are based on
liters per minute (LPM).
See
Stationary and
portable oxygen systems
and contents.
NC
E1405
Oxygen and water
vapor enriching
system with heated
delivery
NC
E1406
Oxygen and water
vapor enriching
system without
heated delivery
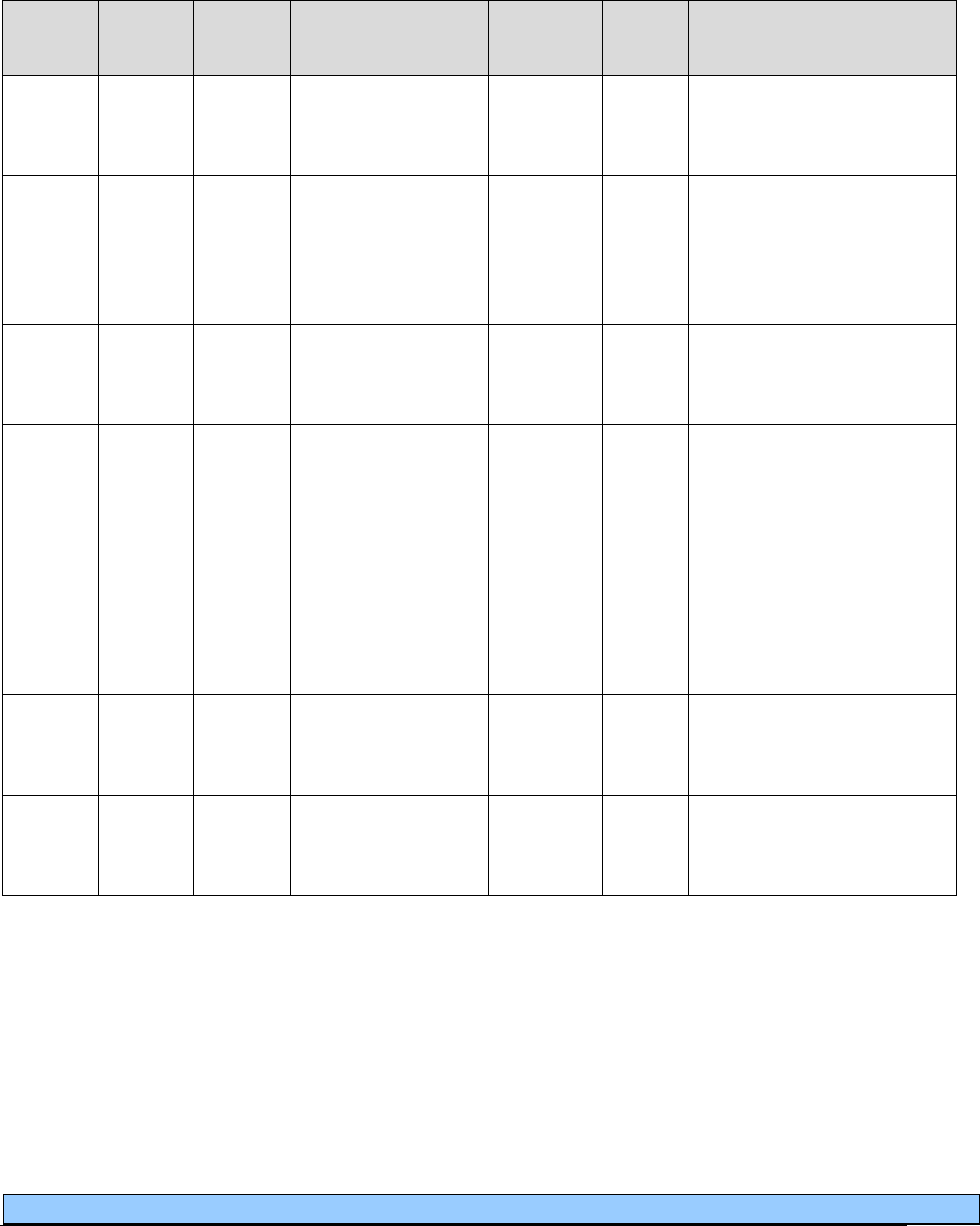
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
72
Suction pump/supplies
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not Bill
With
EPA/
PA?
Policy/
Comments
A4605
NU
Tracheal suction
catheter, closed
system, each
A4624
Limit 1 per day per
client.
A4624
NU
Tracheal suction
catheter, any type,
other than closed
system, each
A4605
Purchase only.
Limit: 150 per client age 8
years and older, every 30
days. 300 per client under age
8, every 30 days.
A4628
NU
Oropharyngeal
suction catheter
(Yankauer), each
Purchase only.
Limit: 4 per client, every 30
days.
A7000
NU
Canister, disposable,
used with suction
pump, each
A7001
Purchase only.
Limit: 5 per client every 30
days for primary suction
pump; 5 per client every 30
days for secondary suction
pump.
Use modifiers NU and TW
together for the secondary
pump.
A7001
NU
Canister, non-
disposable, used with
suction pump, each
A7000
Purchase only.
Limit: 1 every 12 months.
A7002
NU
Tubing, used with
suction pump, each
Purchase only.
Limit: 15 per client, every 30
days.
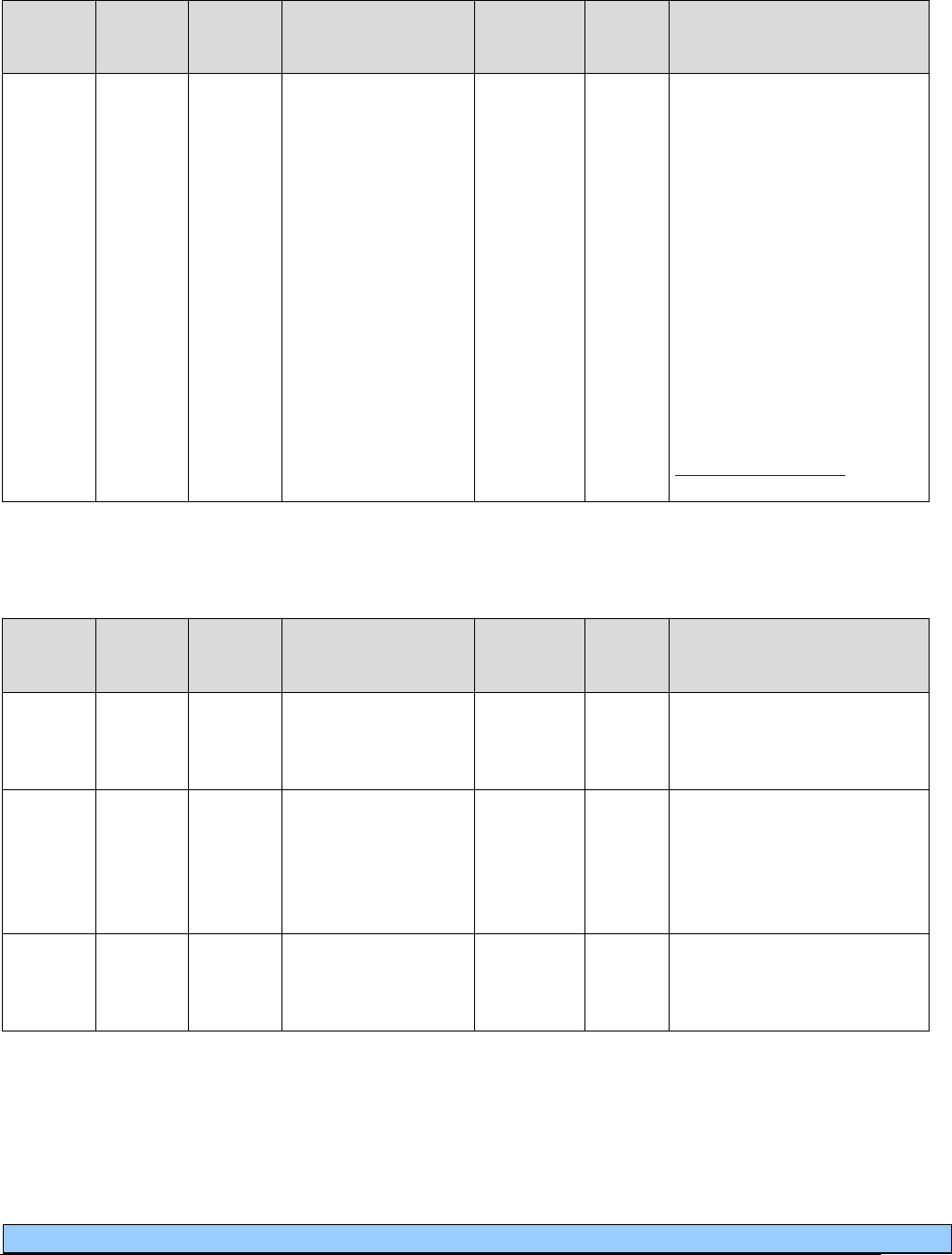
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
73
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not Bill
With
EPA/
PA?
Policy/
Comments
E0600
RR
TW
Respiratory suction
pump, home model,
p
ortable or stationary,
electric
Limit: 2 in 5 years per client,
one for use in the home and
one for back-
up or portability.
Bill RRTW when billing for
the backup unit.
Deemed purchased after 12
months rental.
The agency allows payment
for suction supplies, (e.g.,
gloves and sterile water) when
billed by Durable Medical
Equipment (DME) providers
and pharmacists. (See
Resources Available.)
Tracheostomy care supplies
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not Bill
With
EPA/
PA?
Policy/
Comments
NC
A4481
Tracheostoma filter,
any type, any size,
each
NC
A4483
Moisture exchanger,
disposable, for use
with invasive
mechanical
ventilation
NC
A4608
Transtracheal
oxygen catheter,
each

Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
74
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not Bill
With
EPA/
PA?
Policy/
Comments
A4623
NU
Tracheostomy, inner
cannula (disposable
replacement only)
Purchase only.
Limit: 1 per client, each day.
A4625
NU
Tracheostomy care
kit for new
tracheostomy
A4626
A4629
Includes: basin or tray, trach
dressing, gauze sponges,
pipe cleaners, cleaning
brush, cotton tipped
applicators, twill tape, drape,
and sterile gloves.
Limit: 1 per client, each day.
Use this code for first 14
days only, then use A4629.
A4625 should not be billed
again after the first 14 days.
Purchase only.
NC
A4626
Tracheostomy
cleaning brush, each
A4629
NU
Tracheostomy care
kit for established
tracheostomy
A4625
A4626
Includes: basin or tray, trach
dressing, gauze sponges,
pipe cleaners, cleaning
brush, cotton tipped
applicators, twill tape, drape,
and sterile gloves.
Limit: 1 per client, each day.
Use after the first 14 days.
Do not bill A4625 after the
first 14 days.
Purchase only.
NC
A7501
Tracheostoma valve,
including
diaphragm, each
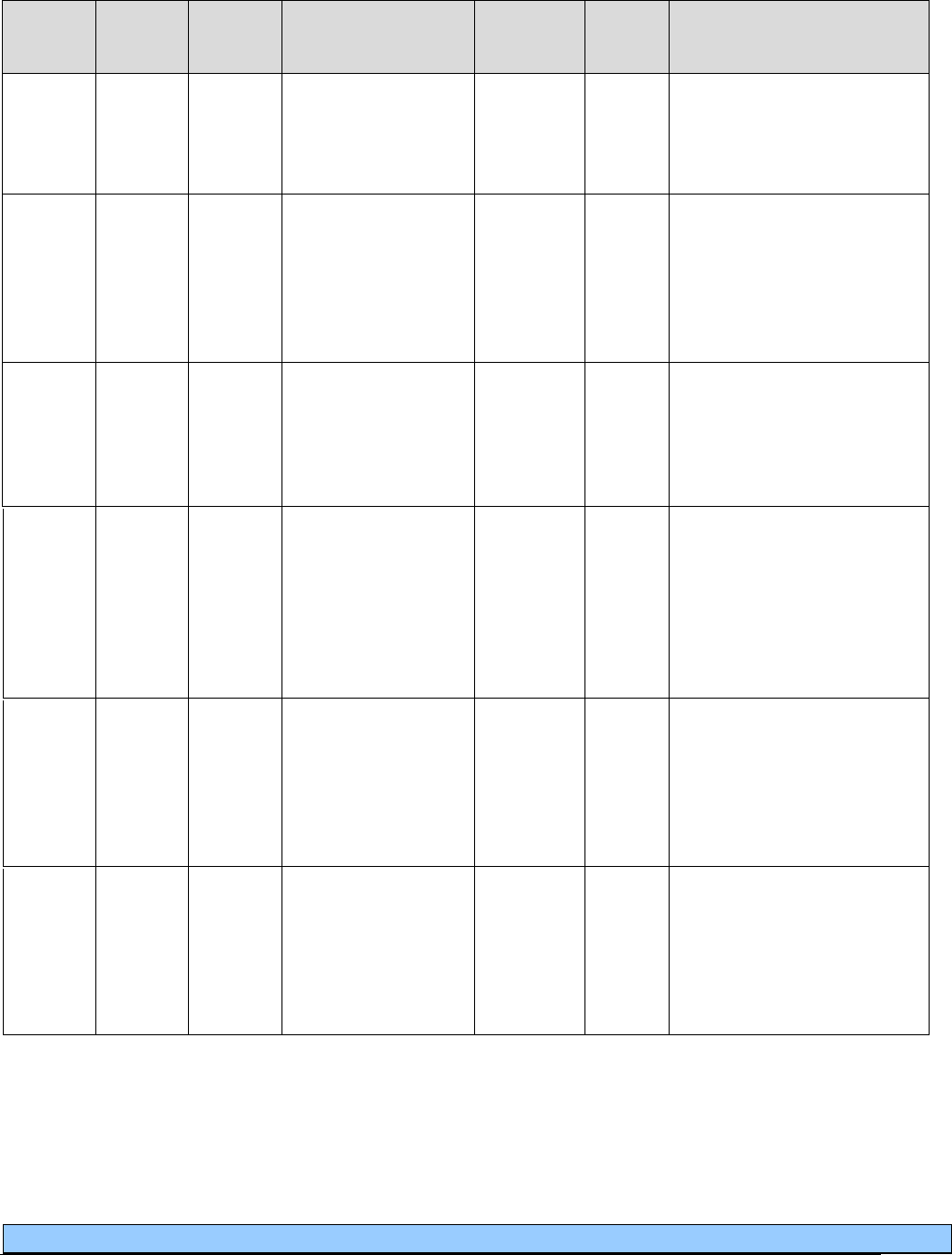
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
75
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not Bill
With
EPA/
PA?
Policy/
Comments
NC
A7502
Replacement
diaphragm/faceplate
for tracheostoma
valve, each
NC
A7503
Filter holder or filter
cap, reusable, for use
in a tracheostoma
heat and moisture
exchange system,
each
NC
A7504
Filter for use in a
tracheostoma heat
and moisture
exchange system,
each
NC
A7505
Housing, reusable
without adhesive, for
use in a heat and
moisture exchange
system or with a
tracheostoma valve,
each
A7520
NU
Tracheostomy/laryn
gectomy tube, non-
cuffed, polyvinyl-
chloride (PVC),
silicone or equal,
each
Limit per client, per 30 days:
1 if removable inner cannula
or 4 each per 30 days if no
removable inner cannula.
A7521
NU
Tracheostomy/laryn
gectomy tube,
cuffed,
polyvinylchloride
(PVC), silicone or
equal, each
Limit: 1 per client every 30
days if removable inner
cannula or 4 per client every
30 days if no removable
inner cannula.
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
76
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not Bill
With
EPA/
PA?
Policy/
Comments
NC
A7506
Adhesive disc for
use in a heat and
moisture exchange
system or with
tracheostoma valve,
any type, each
NC
A7507
Filter holder and
integrated filter
without adhesive, for
use in a
tracheostoma heat
and moisture
exchange system,
each
NC
A7508
Housing and
integrated adhesive,
for use in a
tracheostoma heat
and moisture
exchange system or
with a tracheostoma
valve, each
A7509
NU
Filter holder and
integrated filter
housing, and
adhesive, for use as
tracheostoma heat
and moisture
exchange system
(condenser,
disposable e.g.,
artificial nose), each
Limit: 1 each day for clients
age 8 and older.
Limit: 3 each day for clients
under age 8.
Purchase only.
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
77
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not Bill
With
EPA/
PA?
Policy/
Comments
A7522
NU
Tracheostomy/laryn
gectomy tube,
stainless steel or
equal (sterilizable
and reusable), each
Limit: 1 per client every 30
days if removable inner
cannula or 4 per client every
30 days if no removable
inner cannula.
NC
A7523
Tracheostomy
shower protector,
each
NC
A7524
Tracheostoma
stent/stud/button,
each
A7525
NU
Tracheostomy mask,
each
Purchase only.
Limit: 4 per client, every 30
days.
A7526
NU
Tracheostomy tube
collar/holder, each
Limit: 1 per day, 30 per
month
NC
A7527
Tracheostomy/laryn
gectomy tube
plug/stop
E1399
RR
Heated humidifier
with temperature
modifier and alarms
for clients who have
a tracheostomy
PA
For clients with a
tracheostomy but are not
ventilator dependent.
Monthly rental only.
L8501
NU
Tracheostomy
speaking valve
Purchase only.
Limit: 1 every 6 months.
S8189
Tracheostomy
supply not otherwise
classified
PA
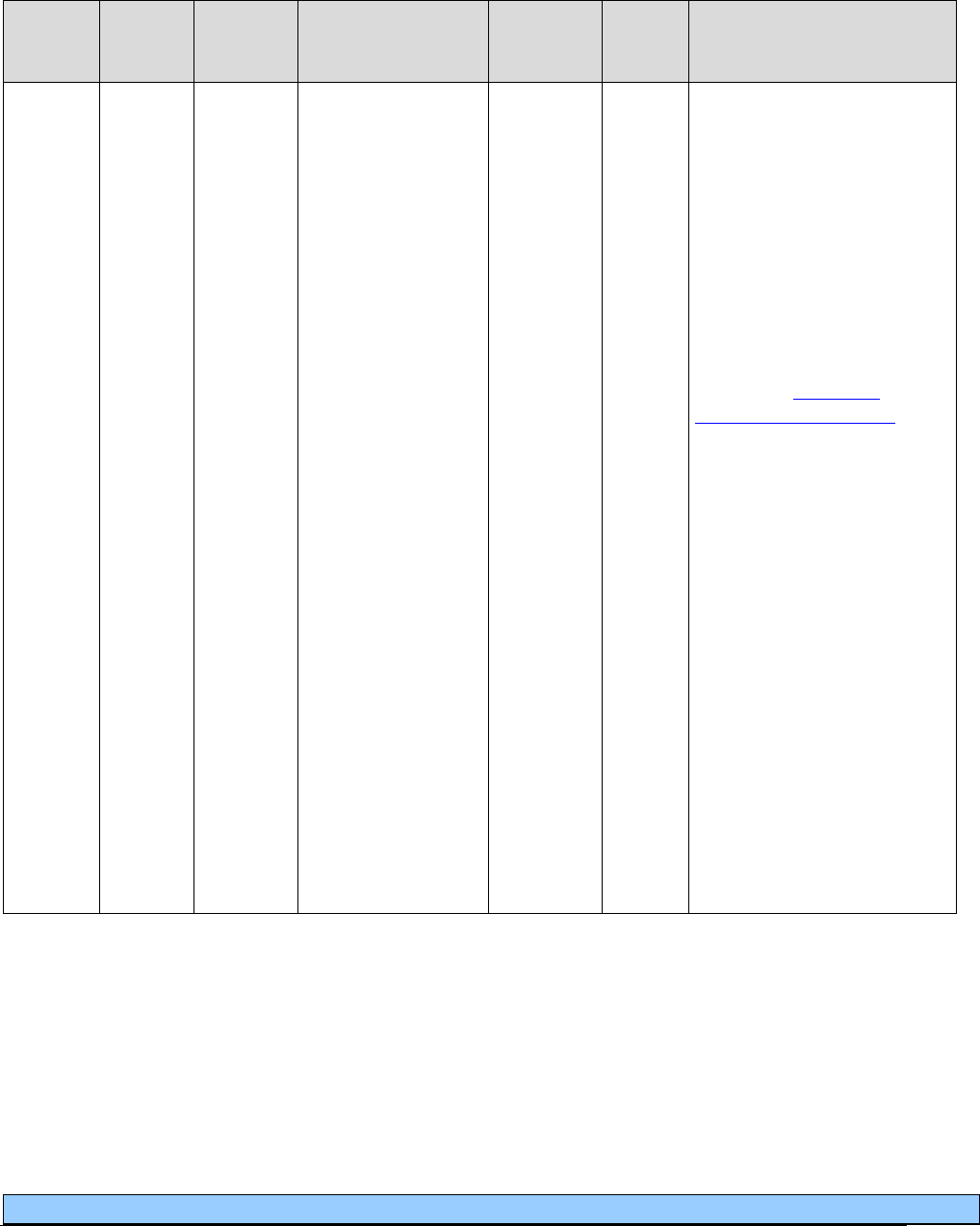
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
78
Ventilators and related respiratory equipment
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E0465
RR
NU
Home ventilator,
any type, used with
invasive interface,
(e.g., tracheostomy
tube)
EPA
Payment includes all
necessary accessories,
fittings, tubing, and
humidifier.
30-days equals 1 unit.
In addition to RR, U2
modifier is required when
claiming a secondary or
backup ventilator for the
same client. (For more
details, see Ventilator
equipment and supplies in
Coverage Criteria.)
Rental only.
For client-owned ventilators
only:
Bill with MS modifier - use
when claiming a 6-month
maintenance check. Limit of
1 per 6 months allowed for
client-owned equipment
beginning 1 year from date
of purchase.
Maintenance checks are
paid at 50% of the rental
rate for client-owned
equipment.
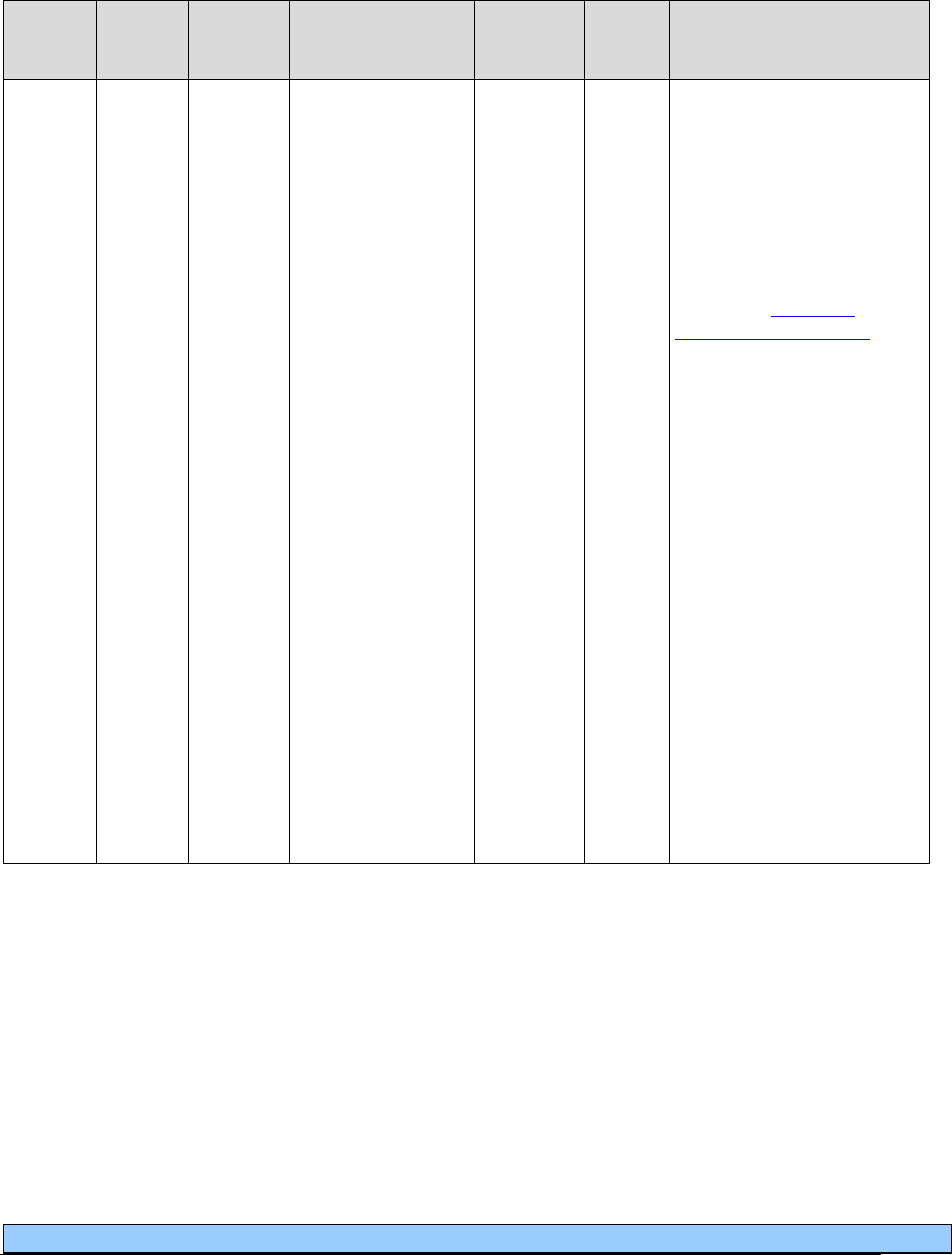
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
79
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E0466
RR
Home ventilator,
any type, used with
non-invasive
interface, (e.g.,
mask, chest shell)
EPA
Payment includes all
necessary accessories,
fittings, tubing, and
humidifier.
U2 modifier is required
when claiming a secondary
or backup ventilator for the
same client. (For more
details, see Ventilator
equipment and supplies in
Coverage Criteria.)
Rental only.
30-days equals 1 unit.
For client-owned ventilators
only:
Bill with MS modifier - use
when claiming a 6-month
maintenance check. Limit of
1 per 6 months allowed for
client-owned equipment
beginning 1 year from date
of purchase.
Maintenance checks are
paid at 50% of the rental
rate for client-owned
equipment.

Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
80
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E0471
RR
RA
Respiratory assist
device, bi-level
pressure capability,
with backup rate
feature, used with
noninvasive
interface, e.g., nasal
or facial mask
(intermittent assist
device with
continuous positive
airway pressure
device)
A4611-
A4613
A4616-
A4618
E0470
E0472
E0601
PA
PA is necessary only if a
CPAP machine (E0601), or
a BiPAP machine (E0470)
has been purchased within
the last 5 years, or if the
clinical criteria are not met.
(For more about criteria, see
Bi-level respiratory assist
devices in Coverage
Criteria.)
Monthly Rental only.
Deemed purchased after 13
months of rental.
Purchase Limit: 1 per client
every 5 years.
Use of RA modifier – the
RA modifier allows for the
replacement of E0471 at the
end of the 5-year limit when
the machine is no longer
functional or cost effective
to repair. This eliminates the
13 month rental
requirement.
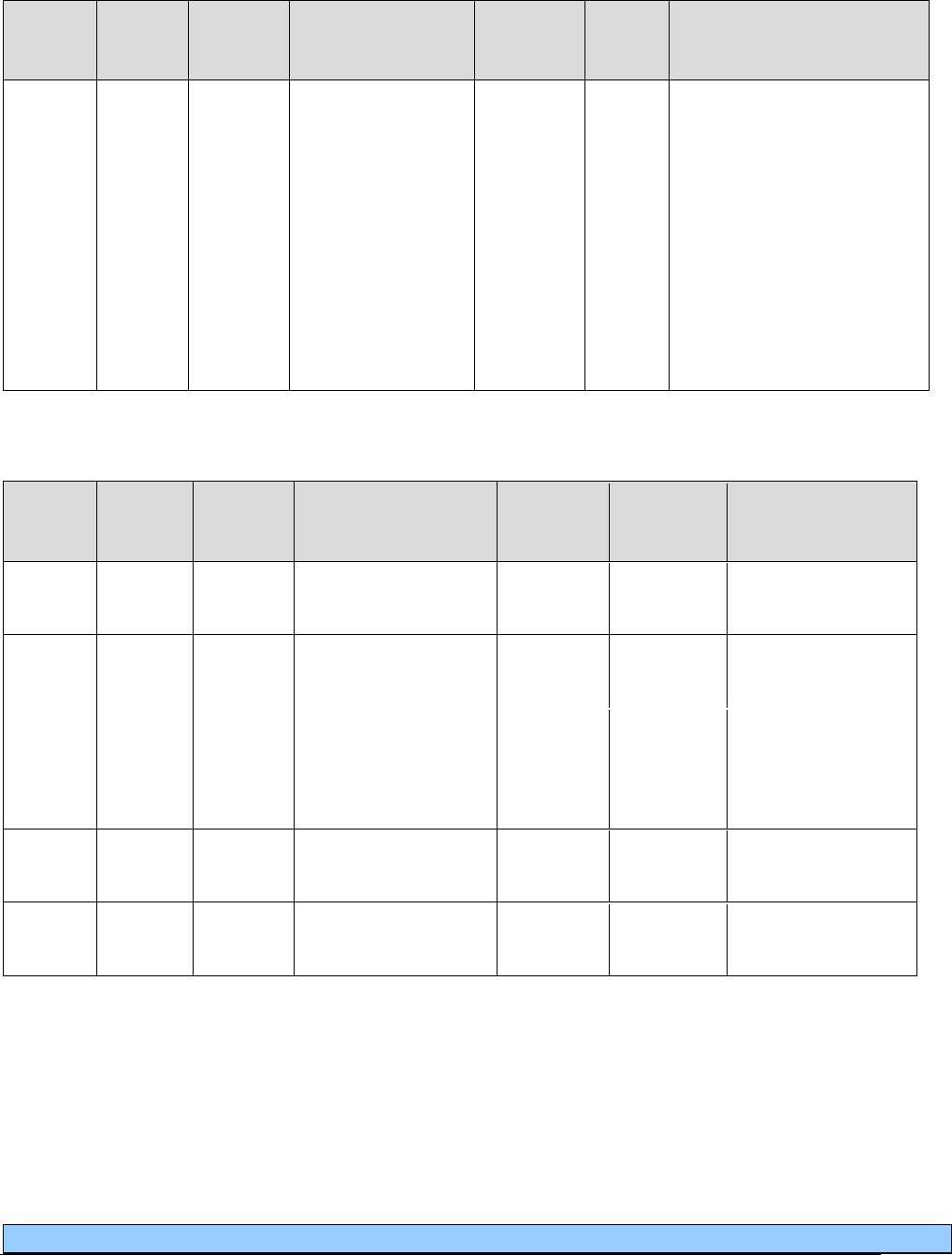
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
81
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E0472
RR
Respiratory assist
device, bi-level
pressure capability,
with backup rate
feature, used with
invasive interface,
e.g., tracheostomy
tube (intermittent
assist device with
continuous positive
airway pressure
device)
A4611-
A4613
A4616-
A4618
E0470
E0471
E0601
Payment includes all
necessary accessories,
fittings, tubing, and
humidifier.
Rental only.
30-days equals 1 unit.
Miscellaneous
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
A4216
Sterile saline or
(sterile) water, 10 ml
Limit: 100 units
every thirty days.
A4217
Sterile saline or
(sterile) water, 500 ml
A7018
E0570
Limit: 50 units every
thirty days.
NC
A4218
Sterile saline or
(sterile) water,
metered dose
dispenser, 10ml
A4450
AU
Tape, non-waterproof,
per 18 square inches
A4452
AU
Tape, waterproof, per
18 square inches
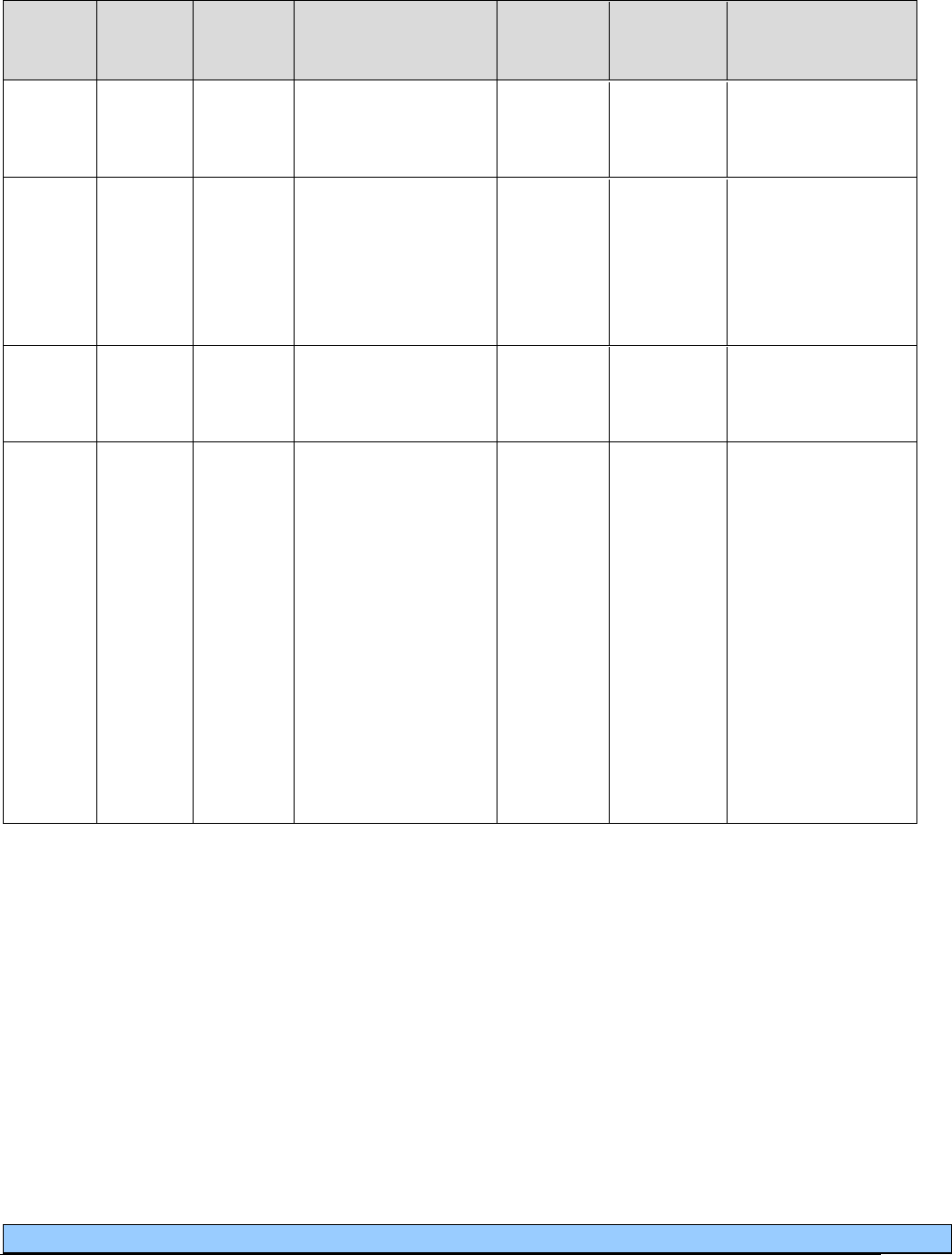
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
82
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
A4614
NU
Peak expiratory flow
rate meter, hand held
Purchase only.
Limit: 3 per client,
every 12 months.
A4627
NU
Spacer, bag or
reservoir, with or
without mask, for use
with metered dose
inhaler (e.g.,
Aerovent)
Limit: 6 per child
(17 and younger),
every 12 months; 3
per adult, (18 and
older) every 12
months.
NC
A9284
Spirometer, non-
electronic, includes
all accessories
E0445
NU
Oximeter device for
measuring blood
oxygen levels non-
invasively
E0445 SC
PA
Standard oximeter.
PA required for
clients age 18 and
older.
PA not required for
clients age 17 and
younger who meet
clinical criteria.
Purchase limit - 1 in
a 24-month period
per client, regardless
of age.
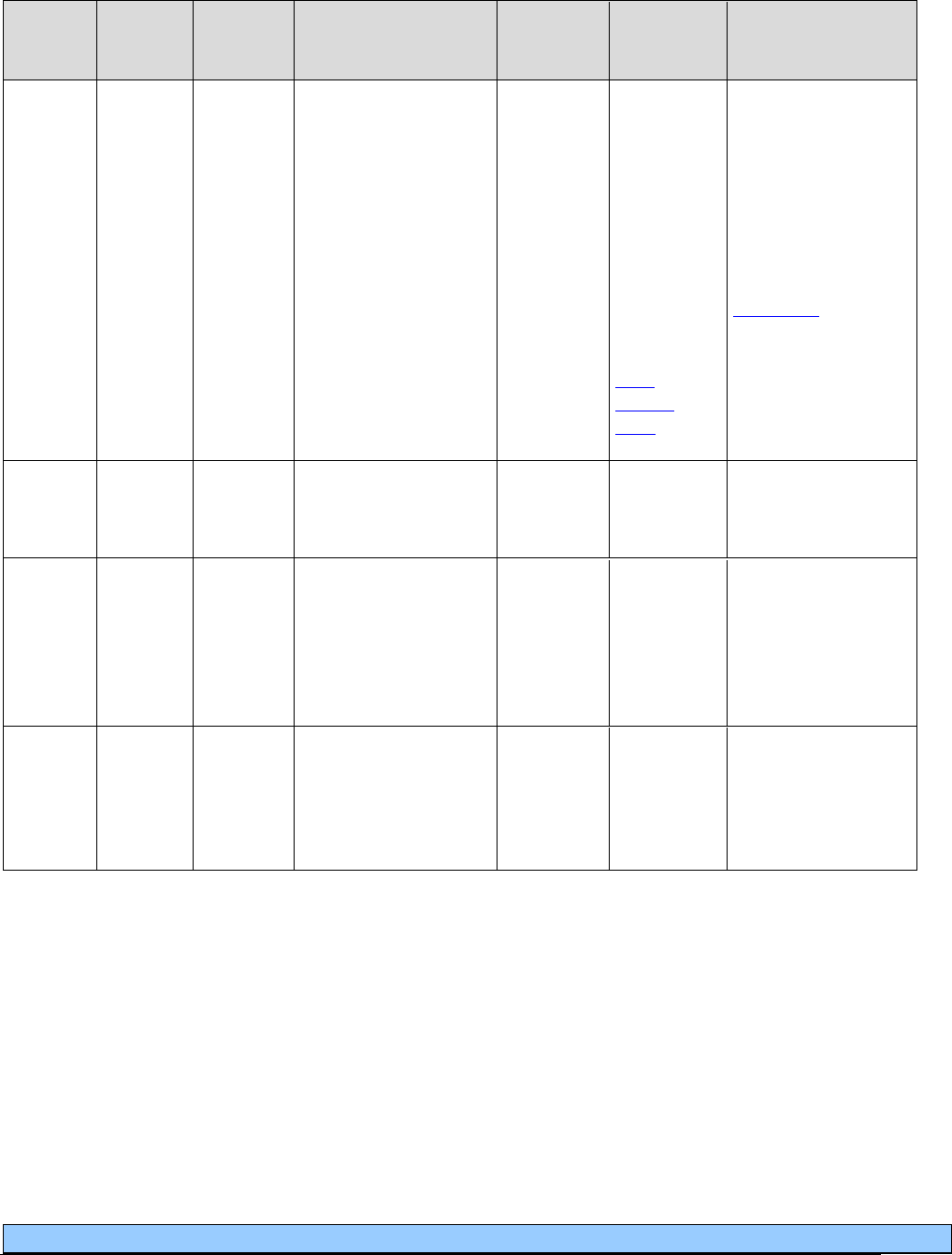
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
83
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E0445
SC
Oximeter device for
measuring blood
oxygen levels non-
invasively
E0445 NU
PA/EPA
EPA
required for
clients who
are 17 years
and
younger
and meet
clinical
criteria.
(See the
EPA
criteria
table.)
Enhanced oximeter.
PA required for
clients 18 years and
older; or for clients
under 18 who do not
meet clinical
criteria. (For more
details, see
Oximeters
in
Coverage Criteria.)
Limit = 1 per client
every 36 months.
E1399
Replacement cable
for enhanced
oximeter
PA
Limit= 2 per client
per year.
A4606
NU
Oxygen probe for use
with oximeter device,
replacement
A4606 RA
NU =
Nondisposable
probe.
Limit = 1 per client
every 180 days.
A4606
RA
Oxygen probe for use
with oximeter device,
replacement
A4606 NU
RA = Disposable
probe.
Limit = 4 per client
every 30 days.
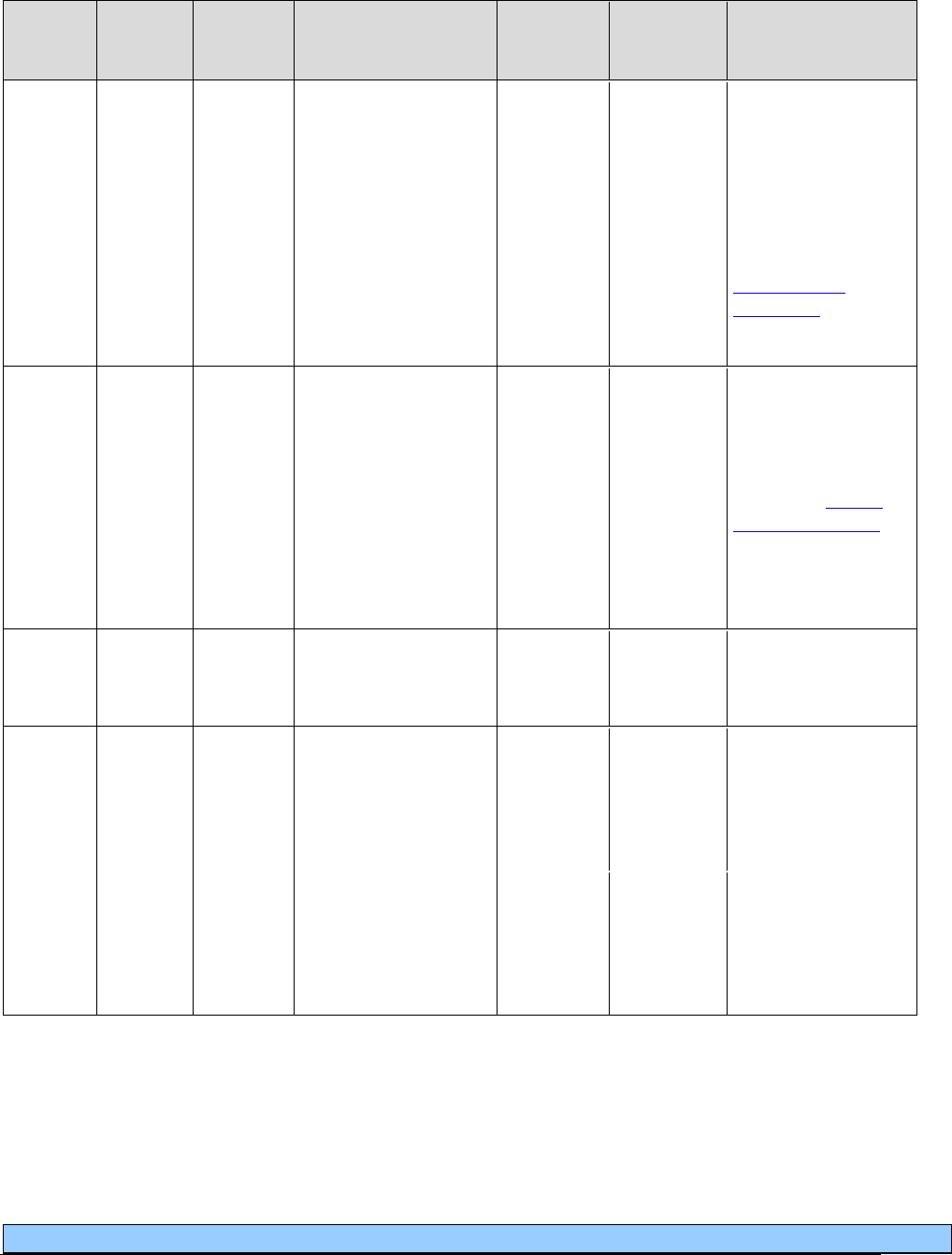
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
84
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E1399
RB
Durable medical
equipment,
miscellaneous
PA
For equipment
without an assigned
HCPCS code.
RB = Only for parts
used in the repair of
client-owned
equipment. (See
Client-owned
equipment in
Reimbursement.)
K0740
Repair or nonroutine
service for oxygen
equipment requiring
the skill of a
technician, labor
component, per 15
minutes
PA
For client-owned
equipment only.
Must include
invoice with actual
labor time defined in
units. (See Client-
owned equipment in
Reimbursement.)
1 unit = 15 min.
E0480
NU
Percussor, electric or
pneumatic, home
model
Purchase only.
Limit: 1 per client,
per lifetime.
NC
E0481
Intrapulmonary
percussive
ventilations system
and related
accessories
E0482
RR
Cough stimulating
device, alternating
positive and negative
airway pressure
PA
Limit: 1 per client,
per lifetime.
Deemed purchased
after 12 months of
rental.
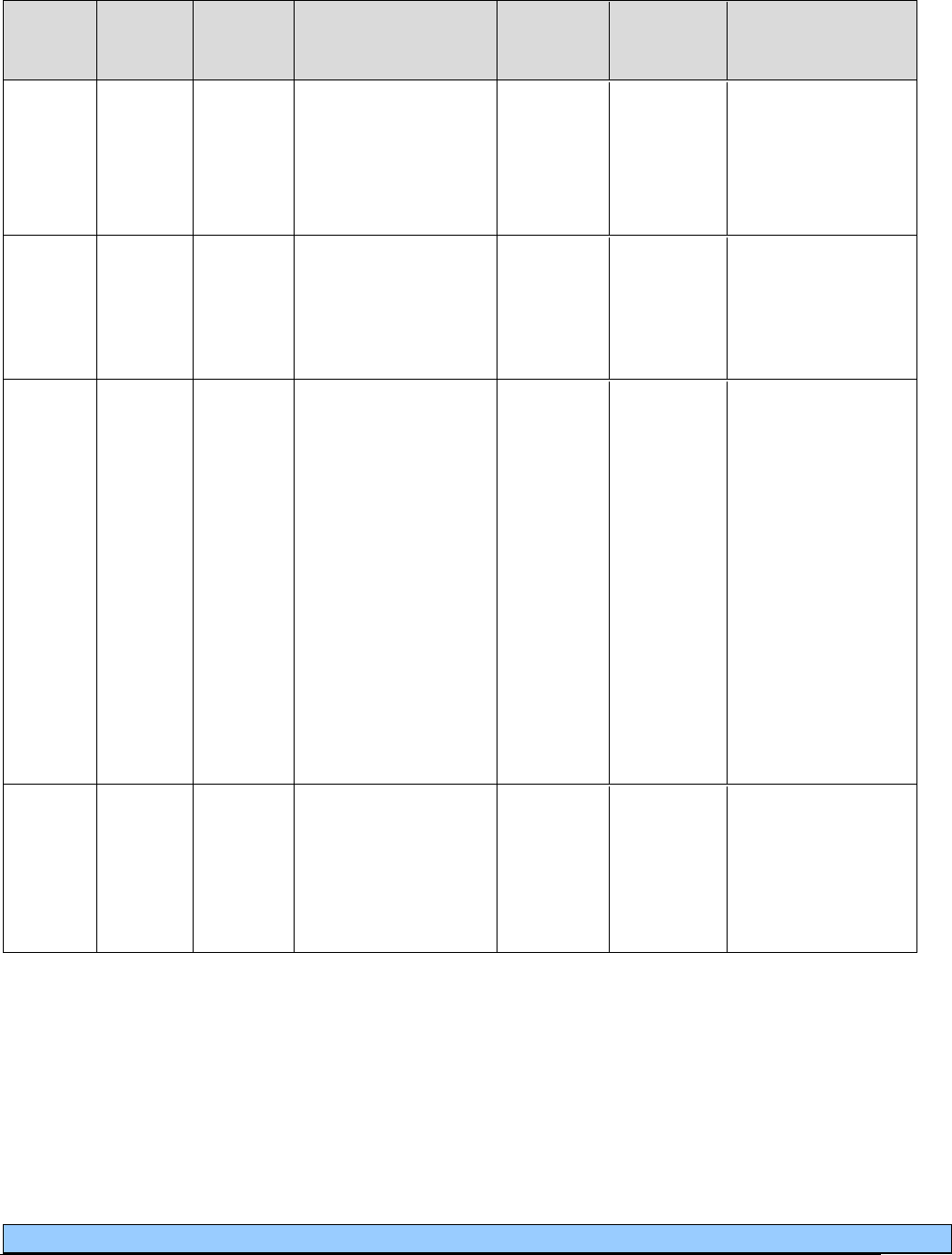
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
85
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
A4601
Lithium ion
rechargeable for
non-prosthetic
use, replacement
only
PA
Limit: 1 per client,
per every 5 years.
A7020
NU
Interface for cough
stimulating device,
includes all
components,
replacement only
PA
E0483
RR
High frequency chest
wall oscillation air-
pulse generator
system, (includes
hoses and vest), each
PA
Rental includes vest
and generator, all
repairs and
replacements.
Manufacturer will
replace vest (during
either rental or
purchase period) for
change in user’s
size.
Limit: 1 per client,
per lifetime.
Deemed purchased
after 12 months of
rental.
A7025
NU
High frequency chest
wall oscillation
system vest,
replacement for use
with client owned
equipment, each
PA
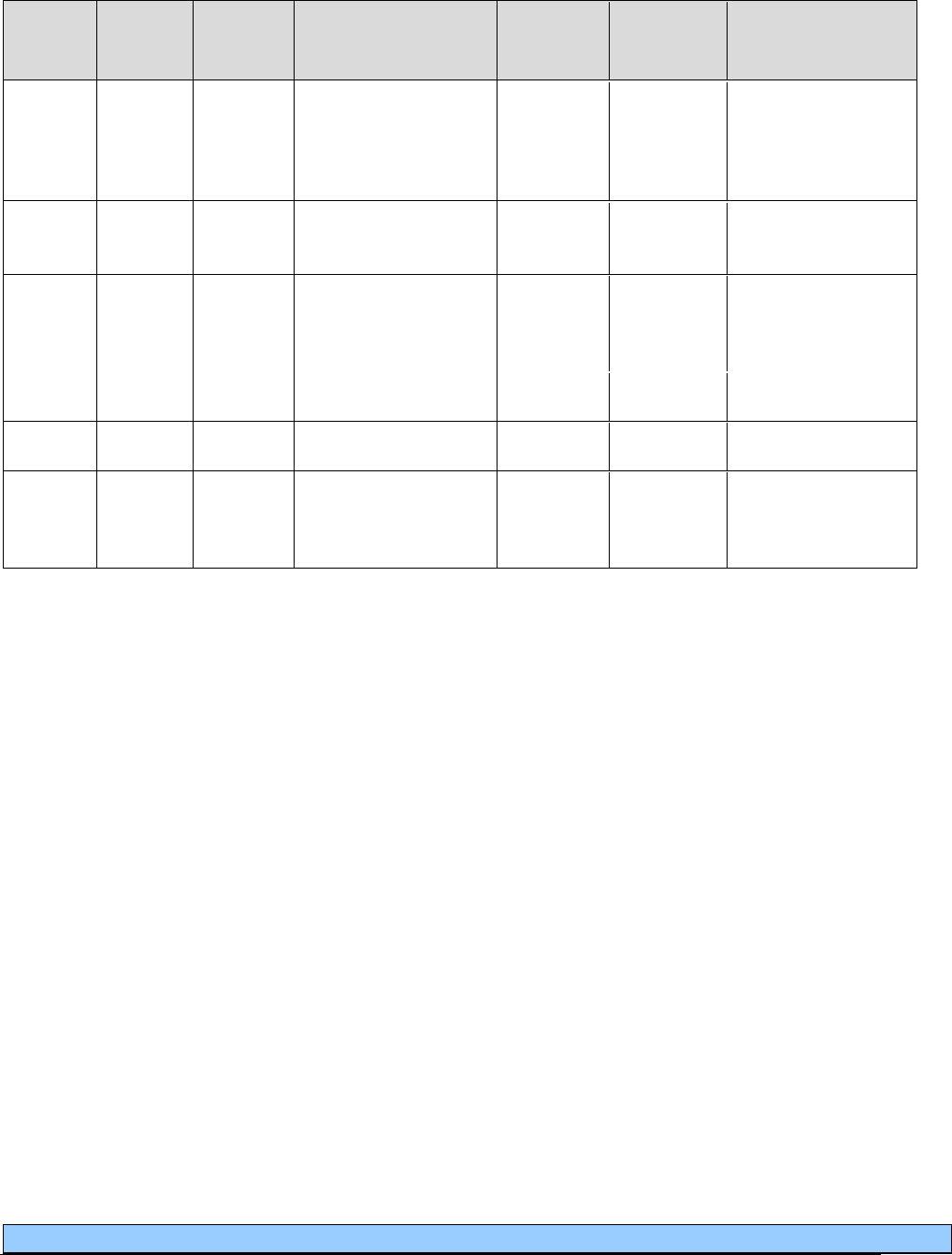
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
86
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill With
EPA/
PA?
Policy/
Comments
E0484
Oscillatory positive
expiratory pressure
device, non-electric,
any type, each
Limit: 1 per client
every 180 days.
S8185
NU
Flutter device
Purchase only.
Limit: 1 every 6
months.
NC
E0487
Spirometer,
electronic, includes
all accessories
NC
S8186
Swivel adaptor
NC
S8210
Mucus trap
S8999
NU
Resuscitation bag,
disposable,
adult/pediatric size
Purchase only.
Limit: 1 every 6
months.

Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
87
Miscellaneous equipment reimbursement
The following equipment is only reimbursed when a client owns the core equipment.
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
A4611
NU
Battery, heavy duty;
replacement for client-
owned ventilator
E0472
Gel cell only.
Purchase only.
Limit: 1 every 24
months.
A4612
NU
Battery cables;
replacement for client-
owned ventilator
E0472
Purchase only.
Limit of 1 every 24
months.
A4613
NU
Battery charger;
replacement for
client-owned
ventilator
E0472
Gel cell only.
Purchase only.
Limit of 1 every 24
months.
NC
A4617
NU
Mouthpiece
A4618
NU
Breathing circuits
E0424
E0431
E0434
E0439
E0472
E1390
E1392
K0738
Purchase only for client -
owned equipment.
Limit: 4 per client, every
30 days.
NC
E0550
Humidifier, durable
for extensive
supplemental
humidification during
IPPB treatments or
oxygen delivery
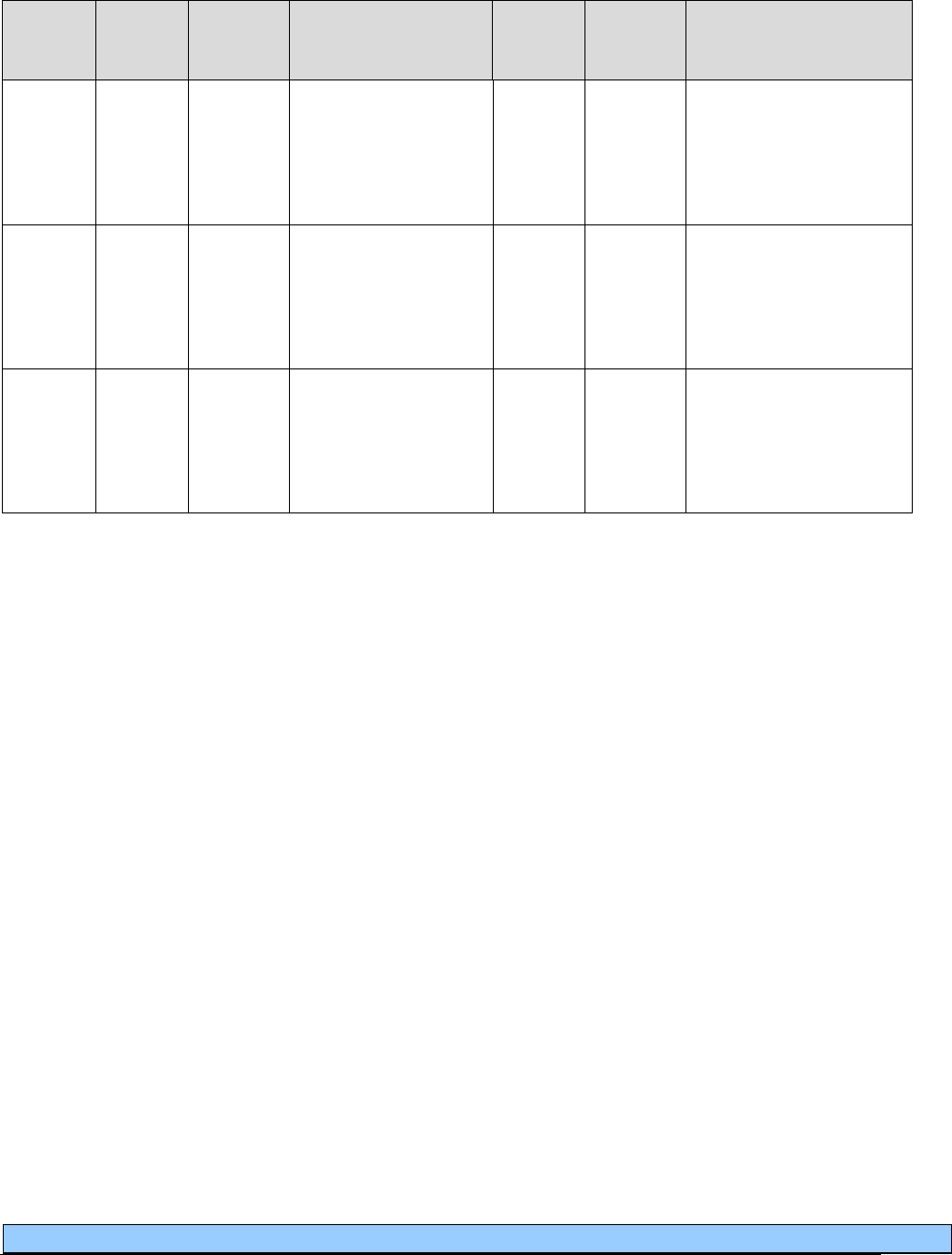
Respiratory Care
Legend
Modifier
RR= Rental equipment
RA = Replacement
MS= Maintenance/service
NU= New Equipment
TW= Backup equipment (not vent)
SC=Enhanced oximeter
NC= Not Covered
RB = Replacement of a part furnished as part of a repair
U2= Back up ventilator
AU = Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
88
Code
Status
Indicator
HCPCS
Code
Modifier
Description
Do Not
Bill
With
EPA/
PA?
Policy/
Comments
NC
E0555
Humidifier, durable,
glass or autoclavable
plastic bottle type, for
use with regulator or
flow meter
NC
E0560
Humidifier, durable
for supplemental
humidification during
IPPB treatment or
oxygen delivery
NC
K0462
RR
Temporary
replacement for client-
owned equipment
being repaired, any
type
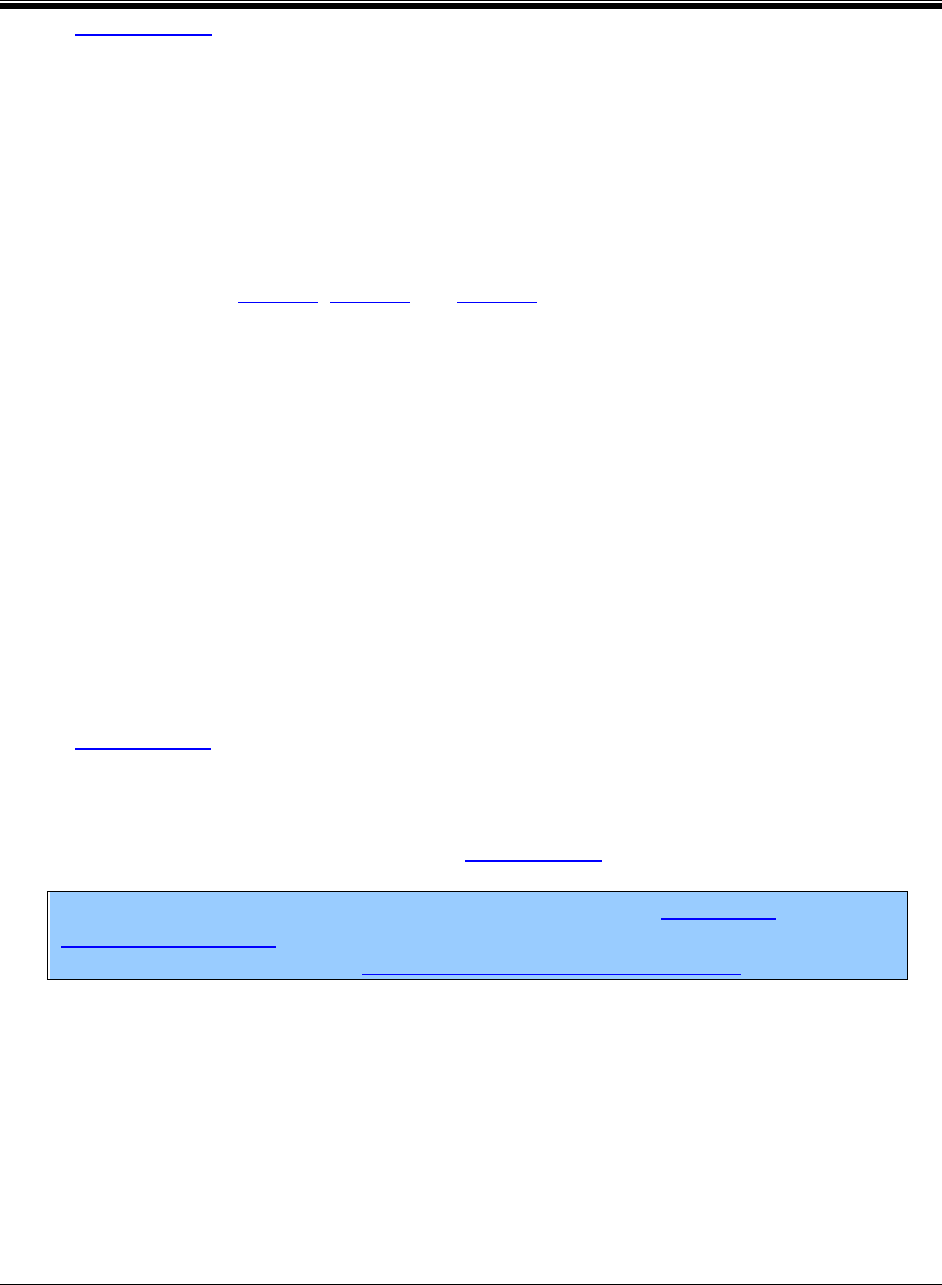
Respiratory Care
89
Authorization
(WAC 182-552-1300)
What are the general authorization
requirements?
• The agency requires providers to obtain authorization for covered respiratory care as
required in:
Chapters 182-552, 182-501 and 182-502 WAC.
Published agency billing guides.
Situations where the required clinical criteria are not met.
• When a service requires authorization, the provider must properly request authorization,
under the agency’s rules and billing guides.
When authorization is not properly requested, the agency rejects and returns the
request to the provider for further action.
The agency does not consider the rejection of a request to be a denial of service.
• The agency’s authorization of service(s) does not necessarily guarantee payment.
• The agency evaluates requests for authorization of covered respiratory care equipment
and supplies that exceed limitations in this chapter on a case-by-case basis under WAC
182-501-0169.
• The agency may recoup any payment made to a provider if the agency later determines
that the service was not properly authorized, or did not meet the expedited prior
authorization (EPA) criteria. (See WAC 182-502-0100(1)(c).
Notes: For submitting claims with authorization numbers, see Billing with
authorization numbers in this guide. For more detailed information on requesting
authorization, see the agency’s ProviderOne billing and resource guide.

Respiratory Care
90
What is prior authorization (PA)?
(WACs 182-552-1300 and 182-552-1325)
Prior authorization (PA) is the agency’s approval for certain medical services, equipment, or
supplies before being provided to clients (except when the items and services are covered by a
third-party payer.) PA is a precondition for provider reimbursement. The item or service must be
delivered to the client before the provider bills the agency.
What are the criteria for PA?
• With PA, the agency may consider covering new respiratory care items that do not have
assigned healthcare common procedure coding system (HCPCS) codes, and are not listed
in the agency’s published issuances.
For these, the provider must furnish all of the following information to the agency to
establish medical necessity:
A detailed description of the item(s) or service(s) to be provided.
The cost or charge for the item(s).
A copy of the manufacturer’s invoice, price list or catalog with the product
description for the item(s) being provided.
A detailed explanation of how the requested item(s) differs from an already
existing code description.
• In addition, for PA requests, the agency requires the prescribing provider to furnish
client-specific justification for respiratory care.
The agency does not accept general standards of care or industry standards for
generalized equipment as justification.
• When the agency receives the initial request for PA, the prescription(s) for those items or
services must not be older than 3 months from the date the agency receives the request.
• The agency does not pay for the purchase, rental, or repair of respiratory care equipment
that duplicates equipment clients already own or rent.
If providers believe the purchase, rental or repair of respiratory care equipment is not
duplicative, they may request PA by submitting the following to the agency:
Reasons the existing equipment no longer meets the client’s medical needs.
Reasons the existing equipment could not be repaired or modified to meet the
client’s medical needs.
Respiratory Care
91
Upon request, documentation showing how the client’s condition meets the
criteria for PA.
• A provider may resubmit a request for PA for an item or service that the agency has
denied. The agency requires the provider to include new documentation that is relevant to
the request.
What is the PA process?
Online direct data entry into Provider One
Providers may submit a PA request online through direct data entry into ProviderOne. See the
agency’s Prior authorization web page for details.
Written requests
Providers who chose to submit a written PA request to the agency must include:
• A completed General Information for Authorization (HCA 13-835) form.
• A completed Oxygen and Respiratory Authorization Request (HCA 15-298) form.
• A prescription.
• Any other required documentation.
(See Where can I download agency forms?)
Additional information required for PA
For purchase or rental of equipment, providers must also provide:
The manufacturer’s name.
The equipment model and serial number.
A detailed description of the item.
Any modifications required, including the product or accessory number as shown in the
manufacturer’s catalog.
(See WAC 182-501-0165.)
Respiratory Care
92
Is PA required for repairs to client-owned
equipment?
To be paid for a repair of client-owned equipment, the provider must submit a PA request to the
agency for repairs and must include:
• A manufacturer pricing sheet showing manufacturer’s list or suggested retail price
(MSRP); or a manufacturer invoice showing the acquisition cost (AC) of the repair,
identifying and itemizing the parts.
• A completed General Information for Authorization (HCA 13-835) form showing, by
line, the HCPCS codes being requested with corresponding billed charges. See Prior
authorization web page for details or Where can I download agency forms if submitting
written PA request.
• A statement on company letterhead indicating that the equipment or parts are no longer
covered by warranty.
• The serial number of the equipment being repaired.
If the equipment did not come with a serial number or the number is no longer legible or
on the equipment, the provider must:
Assign a new number.
Attach it to the equipment.
Include this information on company letterhead.
• Specific respiratory care labor code (K0740).
• Actual labor time used for repairs.
What is expedited prior authorization (EPA)?
(WACs 182-552-1300 and 182-552-1375)
The expedited prior authorization (EPA) process eliminates the need for written requests for PA
of selected respiratory care procedure codes. Services requiring EPA are identified in the EPA
criteria table.
Respiratory Care
93
What are the EPA criteria?
• For EPA, a provider must document how the EPA criteria are met and have supporting
medical documentation. The provider must include all documentation in the client’s file,
available to the agency on request.
• The provider must use the appropriate EPA number and process when billing the agency.
• When a situation does not meet the EPA criteria for selected respiratory care procedure
codes, a written request for PA is required.
• The agency may recoup any payment made to a provider if the provider did not follow
the EPA criteria and process.
What is the EPA process?
Providers must create a 9-digit EPA number for selected respiratory care procedure codes:
• The first five or six digits of the EPA number must be 870000.
• The last three or four digits must be the code assigned to the diagnostic condition,
procedure, or service that meets the EPA criteria. (See the EPA criteria table.)
Example: In billing E0570 for a Nebulizer when the client is 2 years old
and has been diagnosed with acute bronchiolitis, the EPA number would
be 870000900. (870000 = first six digits of all EPA numbers; 900 = last
three digits of an EPA number, indicating the clinical criteria and the
equipment you are billing.)
Note: When the client’s situation does not meet published criteria, authorization
is necessary.
What is a limitation extension (LE)?
(WAC 182-552-1300 and 182-552-1350)
A limitation extension (LE) is the agency’s method for the provider to furnish more units than are
typically allowed.
The agency limits the amount, frequency, or duration of certain covered respiratory care, and pays
up to the stated limit without requiring PA. (Limits are based on what is normally considered
medically necessary, for quantities sufficient for a 30-day supply for one client.)
Respiratory Care
94
What are the LE criteria?
• The provider must request PA for an LE to exceed the stated limits for respiratory care
equipment and supplies using the required process.
• The provider must provide justification that the additional units of service are medically
necessary.
• The agency evaluates LE requests on a case-by-case basis under WAC 182-501-0169.
Note: LEs do not override the client’s eligibility or program limitations. Not all
categories of eligibility can receive all services. For example: Kidney dialysis is
excluded under the Family Planning Only Program.
What is the LE process?
Online direct data entry into Provider One
Providers may submit a limitation extension request online through direct data entry into
ProviderOne. See the agency’s Prior authorization web page for details.
Written requests
Providers who request an LE using the agency’s written/fax authorization process must include
the following:
• A completed General Information for Authorization (HCA 13-835) form.
• A completed Oxygen and Respiratory Authorization Request (HCA 15-298) form.
• A prescription.
• Any other required documentation.
See Where can I download agency forms?
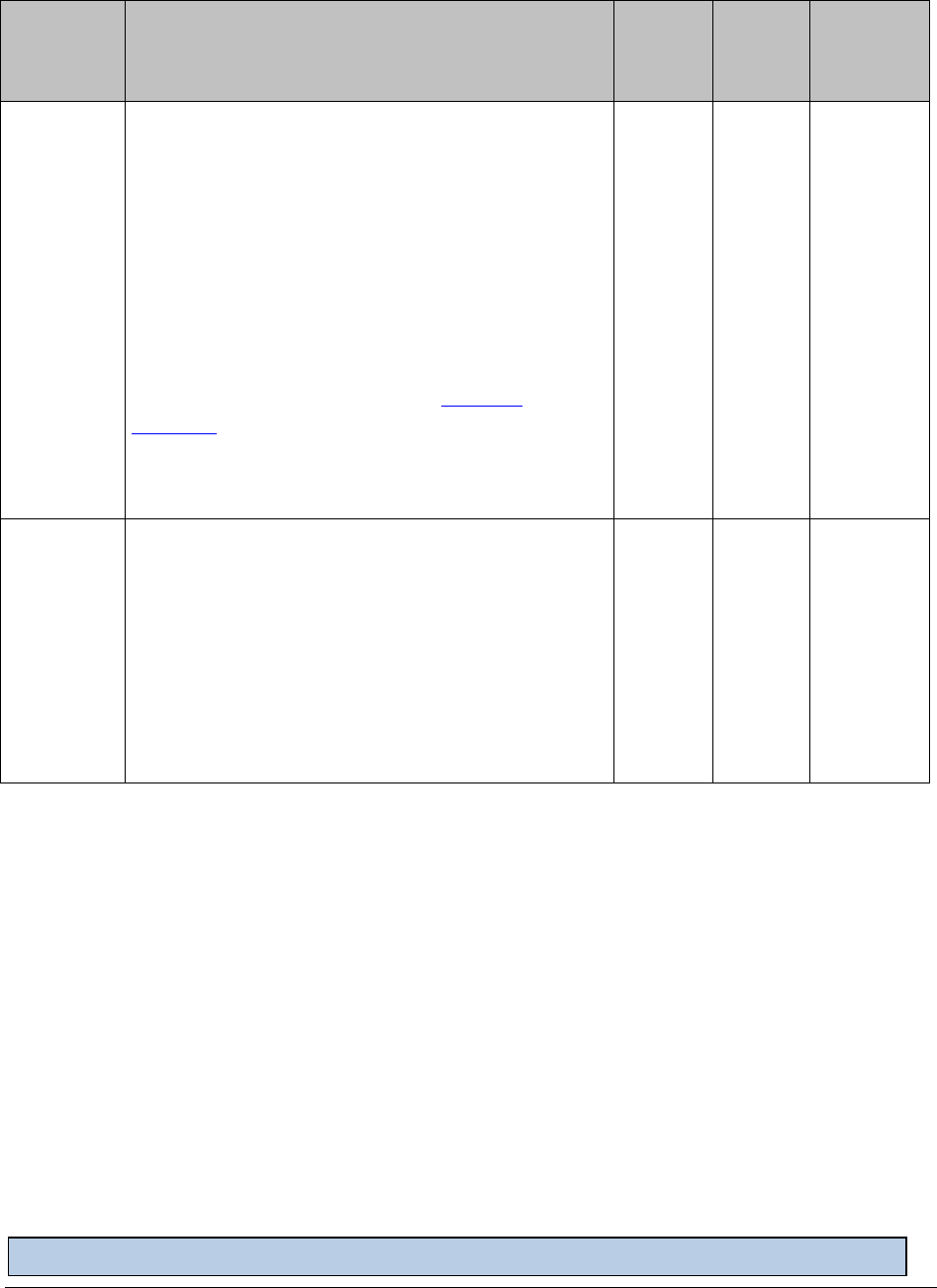
Respiratory Care
Legend
Modifier
RR=Rental Equipment
RA = Replacement
MS= Maintenance and servicing
NU= Equipment Purchase
TW= Backup Equipment(not vent)
SC = Enhanced Oximeter
NC= Not covered
RB = Replacement of a part
U2 = Back up Ventilator
AU= Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
95
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
Expedited prior authorization (EPA) criteria table
EPA
870000+
Last 3
digits
below
Criteria
HCPCS
Code
Modifier
Do Not
Bill With
006
Enhanced Oximeter
With all of the following features:
• Alarms for heart rate and oxygen saturation
• Adjustable alarm volume
• Memory for download
• Internal rechargeable battery
Client must be age 17 and younger, in the home,
and meet the clinical criteria for standard
oximeter.
Purchase limit of 1 per client, every 3 years.
E0445
SC
E0445
NU
000
Home Ventilator (invasive and non-invasive) –
Includes primary and secondary or backup
ventilator for chronic respiratory failure.
If the client has no clinical potential for weaning,
the EPA is valid for 12 months.
If the client has the potential to be weaned, then
the EPA is valid for 6 months.
E0465
E0466
RR
U2
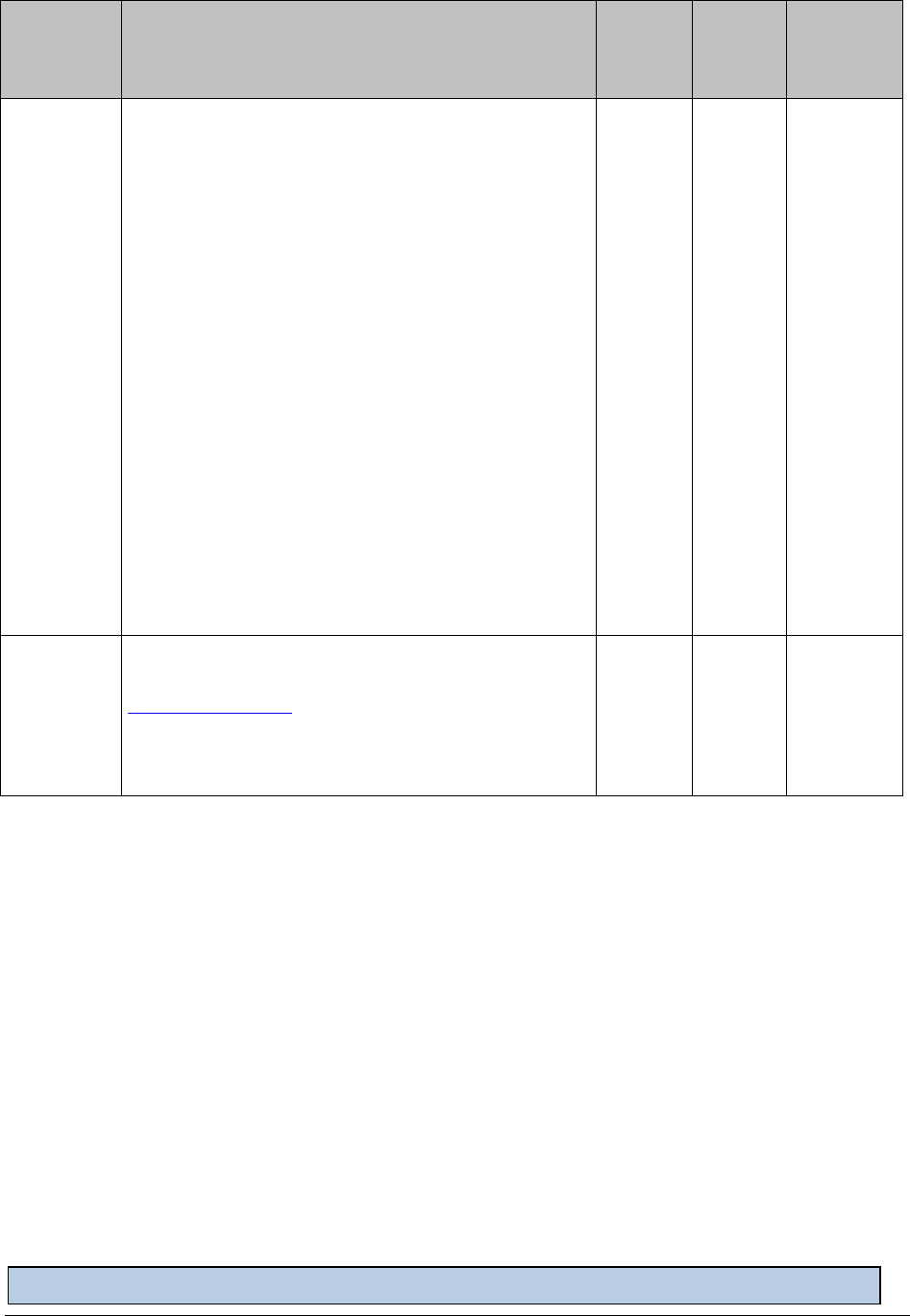
Respiratory Care
Legend
Modifier
RR=Rental Equipment
RA = Replacement
MS= Maintenance and servicing
NU= Equipment Purchase
TW= Backup Equipment(not vent)
SC = Enhanced Oximeter
NC= Not covered
RB = Replacement of a part
U2 = Back up Ventilator
AU= Item furnished in conjunction with a urological, ostomy or tracheostomy supply
**Requires specific modifier based on LPM. See instructions within Coverage Table.
96
Note: Billing provision limited to a 1-month supply. One month equals 30 days.
EPA
870000+
Last 3
digits
below
Criteria
HCPCS
Code
Modifier
Do Not
Bill With
052
Restart 36-month oxygen capped rental when
meeting one of the following criteria:
• The initial provider is no longer providing
oxygen equipment or services.
• The initial provider’s Core Provider
Agreement with the agency is terminated or
expires.
• The client moves to an area that is not part of
the provider’s service area. (This applies to
Medicaid-only clients.)
• The client moves into a permanent residential
setting.
• A pediatric client is transferred to an adult
provider.
RR
900
Nebulizer with compressor. Use this EPA for
clients who do not meet the clinical criteria (in
Coverage Criteria), but who have a diagnosis of
acute bronchiolitis, or acute bronchitis requiring
the administration of nebulized medications.
E0570
NU
E0500

Respiratory Care
97
Noncovered Services
(WAC 182-552-1200)
What types of services are not covered by the
agency?
• In addition to the noncovered services found in WAC 182-501-0070, the agency does not
cover:
Emergency or stand-by oxygen systems, including oxygen as needed.
Portable nebulizer.
Kits and concentrates for use in cleaning respiratory equipment.
Intrapulmonary percussive ventilation system and related accessories.
Battery for a CPAP.
An item or service which primarily serves as a convenience for the client or
caregiver.
Oximetry checks.
Loaner equipment.
• The agency evaluates a request for respiratory care that is listed as noncovered in this
guide under the provisions of WAC 182-501-0160.
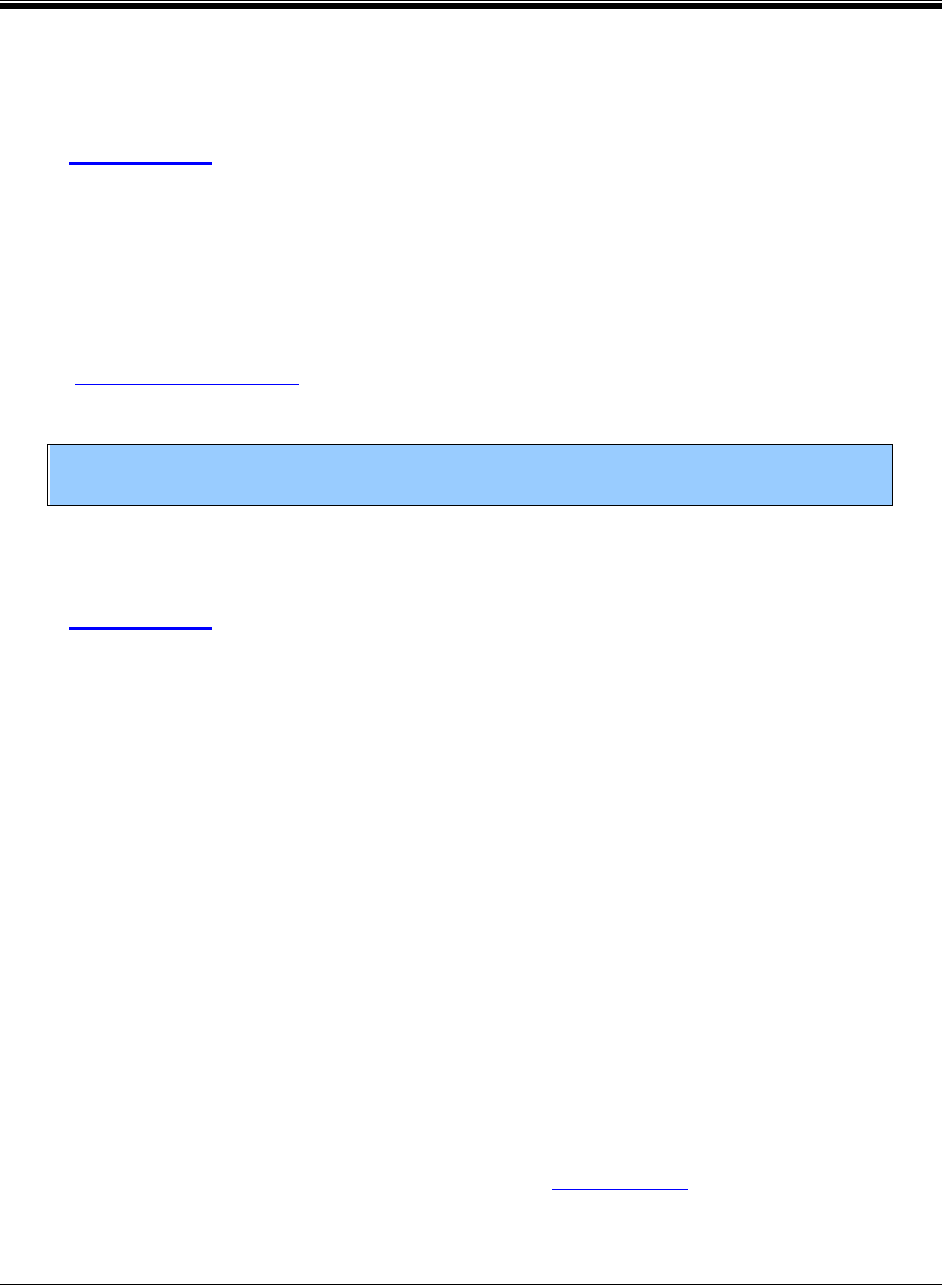
Respiratory Care
98
Reimbursement
What is the general payment for respiratory
care?
(WAC 182-552-1400)
The agency pays qualified providers for covered respiratory care services, equipment, and
supplies on a fee-for-service (FFS) basis.
Agency-enrolled durable medical equipment (DME) providers, pharmacies, and home health
agencies are paid under their national provider identifier (NPI) numbers according to:
• Chapter 182-552 WAC and this billing guide.
• Healthcare common procedure coding system (HCPCS) guidelines.
Note: The agency is the payor of last resort for clients with Medicare or third-party
insurance.
Maximum allowable fees
(WAC 182-552-1400)
The agency updates the maximum allowable fees at least once per year, unless otherwise
directed by the legislature or considered necessary by the agency.
The agency sets, evaluates, and updates the maximum allowable fees for respiratory care
services, equipment and supplies using available published information, including but not limited
to:
• Commercial databases
• Manufacturer’s catalogs
• Medicare fee schedules
• Wholesale prices
The agency may adopt policies, procedure codes, and/or rates that are inconsistent with those set
by Medicare if the agency determines that such actions are necessary.
The maximum payment is either of the following, whichever is less:
• Providers’ usual and customary charges.
• Established rates, except those provided in WAC 182-502-0110(3).

Respiratory Care
99
Reimbursement rates
(WAC 182-552-1400(8))
The agency’s reimbursement rates for respiratory care include:
• Any adjustments or modifications to the equipment that are either required within 3
months of the delivery date; or are covered under the manufacturer’s warranty.
• Pick-up, delivery, or associated costs such as mileage, travel time, or gas.
• Telephone calls.
• Shipping, handling, and postage.
• Fitting and setting up.
• Instructions to the client or client’s caregiver about the use of the oxygen or respiratory
care equipment and supplies.
What does the agency not pay for?
(WAC 182-552-1400)
• The dispensing provider who furnishes respiratory care equipment or supplies to a client
is responsible for any costs incurred to have a different provider repair the equipment
when all of the following apply:
Any equipment or supply that the agency considers purchased requires repair
during the applicable warranty period.
The provider refuses or is unable to fulfill the warranty.
The respiratory care equipment or supply continues to be medically necessary.
• The agency does not pay for respiratory care equipment and supplies, or related repairs
and labor charges under fee-for-service (FFS) when the client is:
An inpatient hospital client.
Terminally ill and receiving hospice care.
An enrollee in a risk-based MCO that includes coverage for such items or
services.

Respiratory Care
100
• The agency rescinds any purchase order for a prescribed item if the equipment or supply
was not provided to the client before the client:
Dies.
Loses medical eligibility.
Becomes covered by a hospice agency.
Becomes covered by an MCO.
How does the agency decide to rent or purchase
equipment?
(WAC 182-552-1500)
• The agency bases its decision to rent or purchase respiratory care equipment and supplies
on the cost and length of time the client needs the equipment.
• A provider must not bill the agency for the rental or purchase of equipment supplied to
the provider at no cost by suppliers or manufacturers.
• The agency purchases new respiratory equipment only.
A new respiratory item that is placed with a client initially as a rental item is
considered a new item by the agency at the time of purchase.
A used respiratory item that is placed with a client initially as a rental item must
be replaced by the supplier with a new item before purchase by the agency.
• The agency requires a dispensing provider to ensure that the respiratory equipment rented
to a client:
Is in good working order.
Is comparable to equipment the provider rents to clients with similar medical
equipment needs who are either private pay clients or who have other third-party
coverage.
• The agency’s minimum rental period for covered respiratory care equipment and supplies
is one day.
• The agency’s reimbursement for rented respiratory care equipment and supplies includes:
A full service warranty.
Cost of delivery to, or pick-up from, the client’s residence and, when appropriate,
to and from the room in which the equipment will be used.
Fitting, set-up, adjustments, and modifications.

Respiratory Care
101
Maintenance, repair and replacement, and cleaning of the equipment.
Instructions to the client and the client’s caregiver for safe and proper use of the
equipment.
All medically necessary accessories, contents, and disposable supplies, unless
separately billable according to these billing instructions.
• The agency considers some rented equipment to be purchased after 12 months’ rental,
unless the equipment is restricted as rental only, or is otherwise defined in this guide.
• Respiratory care equipment and related services purchased by the agency for a client are
the client’s property, unless identified as capped rental items by the agency. Capped
rental items are considered the property of the provider.
• In the event of a client’s ineligibility, death, or discontinued use of equipment, rental fees
end on the last day of eligibility, life, or medically necessary usage. Reimbursement will
be prorated in these cases.
• For a client who is eligible for both Medicare and Medicaid, the agency discontinues
paying the client’s coinsurance and deductible for rental equipment when either of the
following applies:
The reimbursement amount reaches Medicare’s reimbursement cap for the
equipment.
Medicare considers the equipment purchased.
What does the agency pay when replacement of
rental equipment and supplies is needed?
(WAC 182-552-1400(12))
If rental respiratory equipment or supplies must be replaced during the warranty period, the
agency recoups 50% of the total amount previously paid toward the rental costs and eventual
purchase of the equipment or supplies if:
• The provider is unwilling or unable to fulfill the warranty.
• The respiratory care equipment or supply continues to be medically necessary.
Respiratory Care
102
What rental equipment does the agency not pay
for?
(WAC 182-552-1500(11) and (12))
The agency does not pay for:
• Insurance coverage against liability, loss or damage to rental equipment that a provider
supplies to a client.
• Defective equipment.
• The cost of materials covered under the manufacturer’s warranty or administrative fees
charged by the manufacturer to perform warranty or repair work.
• Repair or replacement of equipment as a result of the client’s carelessness, negligence,
recklessness, or misuse in accordance with WAC 182-501-0050(7). (The agency may
request documentation, such as a police report, for equipment repair or replacement at its
discretion.)
Does the agency pay for only new equipment?
(WAC 182-552-1500)
The agency pays for equipment that is new at the time of purchase. This may be the same
equipment that is provided to the client during the initial rental.
Note: If the equipment was not new at the time of the initial rental, the
supplier must replace it with new equipment before the agency purchases it.
• Purchased equipment becomes the property of the client, unless identified as capped
rental items by the agency. Capped rental items are considered the property of the
provider.
• The provider must make warranty information, including date of purchase, applicable
serial number, model number or other unique equipment identifier, and warranty period
and warranty period, available to the agency upon request.
• The agency does not pay for:
Defective equipment.
The cost of materials (and associated labor) covered under the manufacturer’s
warranty.
Respiratory Care
103
When does the agency pay for new equipment on
capped-rental items?
(WAC 182-552-1500 (13))
Capped rental equipment is considered to have a reasonable useful lifetime of 5 years. The
agency will pay for new equipment on capped rental items for eligible clients after 5 years of
continuous use, at which point the capped rental period of 36 months will start again.
When does the agency pay for repairs on client-
owned equipment?
(WAC 182-552-1500 (13))
• Equipment is considered to be client-owned if:
It is not identified as a capped rental item in this billing guide.
The agency has reached the maximum reimbursement for the item.
• The agency pays for the repair (parts and labor) of client-owned respiratory equipment
with PA.
The agency’s bases the decision to pay for repairs to client-owned equipment on
cost and length of time the client needs the equipment.
The agency considers the age of the equipment.
In addition, all these criteria must be met:
All warranties are expired.
The cost of the repair is less than 50% of the cost of a new item and the
provider has supporting documentation.
The repair has a warranty for a minimum of 90 days.
Note: If a provider does not obtain PA, the agency will deny the billing, and the
client must not be held financially responsible for the service.
• The reimbursement rate for client-owned equipment includes, but is not limited to:
A manufacturer’s warranty for a minimum warranty period of 1 year for medical
equipment, not including disposable/nonreusable supplies.
Instructions to the client and the client’s caregiver for safe and proper usage of the
equipment.
Respiratory Care
104
The cost of delivery to the client’s residence or skilled nursing facility and, when
appropriate, to the room in which the equipment will be used.
Does the agency require PA for repairs of client-
owned equipment?
(WAC 182-552-1600(6))
For reimbursement, the agency requires providers to submit PA for repairs of client-owned
equipment.
The provider must use assigned HCPCS codes for parts in the repair. For parts without an
assigned HCPCS code, the agency evaluates those parts as By-Report items. The provider must
submit a manufacturer pricing sheet or manufacturer invoice to the agency for reimbursement.
• The reimbursement for by-report parts used in a repair is either:
Eighty percent of the manufacturer’s list or suggested retail price as of October 31
of the base year.
The cost from the manufacturer’s invoice.
• Reimbursement for actual labor charges are made according to the agency’s current fee
schedule.
The provider must follow HCPCS coding guidelines and submit an authorization request
with actual labor units identified and supported by documentation.
Note: Base labor charges or other administrative-like fees will not be reimbursed.
The agency does not cover:
• Repairs (parts or labor) to equipment under warranty.
This includes equipment that was rented and subsequently considered client-owned by
the agency, but still under warranty.
• A base or minimum labor fee that is added to the charges for the actual labor in doing the
repair.
• Equipment, when there is evidence of malicious damage, culpable neglect, or wrongful
disposition.
The agency does not reimburse separately for troubleshooting, telephone calls, delivery
or mileage, or travel time. These services are included in the reimbursement for other
equipment and services. (See WAC 182-552-1400).

Respiratory Care
105
What payment methodology does the agency use
for the purchase of respiratory care equipment?
(See WAC 182-552-1600(1)-(3))
The agency sets, evaluates and updates the maximum allowable fees for purchased respiratory
care equipment at least once yearly using one or more of the following:
• The current Medicare rate, as established by the federal Centers for Medicare and
Medicaid Services (CMS), for a new purchase if a Medicare rate is available.
• A pricing cluster.
• On a by-report basis.
Establishing payment rates for purchased respiratory care equipment based on pricing clusters.
• A pricing cluster is based on specific HCPCS code.
• The agency’s pricing cluster is made up of all the brands/models for which the agency
obtains pricing information. However, the agency may limit the number of brands/models
included in the pricing cluster. The agency considers all of the following when
establishing the pricing cluster:
A client’s medical needs
Product quality
Introduction, substitution or discontinuation of certain brands/models
Cost
• When establishing the fee for respiratory care equipment items in a pricing cluster, the
maximum allowable fee is the median amount of available manufacturers’ list prices for
all brands/models as noted in the pricing cluster.
The agency evaluates a by- report (BR) item, procedure, or service for its medical necessity,
appropriateness and payment value on a case-by-case basis. The agency calculates the payment
rate for these items at 80% of the manufacturer’s list price.

Respiratory Care
106
How does the agency establish monthly rental
reimbursement rates for respiratory care
equipment?
(WAC 182-552-1600(4))
The agency’s maximum allowable fee for monthly rental is established using one of the
following:
• For items with a monthly rental rate on the current Medicare fee schedule, as established
by the federal Centers for Medicare and Medicaid Services (CMS), the agency equates its
maximum allowable fee for monthly rental to the current Medicare monthly rental rate.
• For items that have a new purchase rate but no monthly rental rate on the current
Medicare fee schedule, as established CMS, the agency sets the maximum allowable fee
for monthly rental at 1/10 of the new purchase price of the current Medicare rate.
• For items not included in the current Medicare fee schedule, as established by CMS, the
agency considers the maximum allowable monthly payment rate as By Report. The
agency calculates the monthly payment rate for these items at 1/10 of 80% of the
manufacturer’s list price.
How does the agency establish daily rental
payment rates for respiratory care equipment?
(WAC 182-552-1600(5))
The agency’s maximum allowable fee for daily rental is established using one of the following:
• For items with a daily rental rate on the current Medicare fee schedule, as established by
the federal Centers for Medicare and Medicaid Services (CMS), the agency equates its
maximum allowable fee for daily rental to the current Medicare daily rental rate.
• For items that have a new purchase rate but no daily rental rate on the current Medicare
fee schedule, as established CMS, the agency sets the maximum allowable fee for daily
rental at 1/300 of the new purchase price of the current Medicare rate.
• For items not included in the current Medicare fee schedule, as established by CMS, the
agency considers the maximum allowable daily payment rate as By Report. The agency
calculates the daily payment rate for these items at 1/300 of 80% of the manufacturer’s
list price.
Where is the program fee schedule?
See the agency’s Respiratory care fee schedule web page.
Respiratory Care
107
Billing
All claims must be submitted electronically to the agency, except under limited circumstances.
For more information about this policy change, see Paperless billing at HCA.
For providers approved to bill paper claims, see the agency’s Paper claim billing resource.
What are the general billing requirements?
Providers must follow the agency’s ProviderOne billing and resource guide. These billing
requirements include:
• Time limits for submitting and resubmitting claims and adjustments.
• When providers may bill a client.
• How to bill for services provided to primary care case management (PCCM) clients.
• How to bill for clients eligible for both Medicare and Medicaid.
• How to handle third-party liability claims.
• Standards for record keeping.
Billing with authorization numbers
• Refer to the ProviderOne billing and resource guide for instructions on how to add
authorization numbers to electronic claims.
• With HIPAA implementation, multiple authorization (prior or expedited) numbers may
be submitted on a claim when billing electronically. The authorization number must be
placed in the correct data field of the claim. Do not put authorization numbers in the
comment field, as they cannot be processed.
Is information available to bill for clients eligible
for both Medicare and Medicaid?
For more information on billing Medicare/Medicaid crossover claims, see the agency’s
ProviderOne billing and resource guidee.
Note: When Medicare has paid as primary insurance and you are billing the agency as the
secondary payer, the agency does not require PA for services.
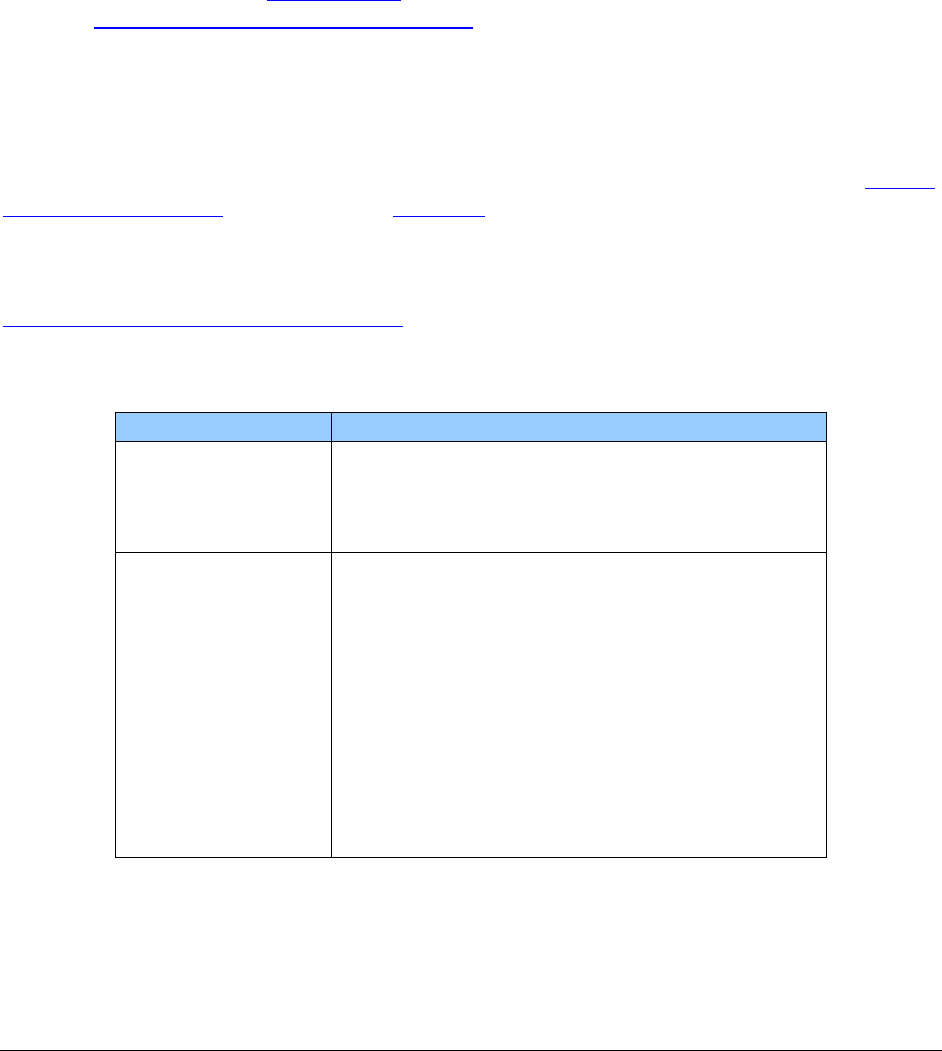
Respiratory Care
108
How does the agency handle third-party liability
coverage?
If the client has third-party liability (TPL) coverage for a service requiring authorization by the
agency, and the TPL payer denies payment for that service, authorization must be obtained
through the agency. A denial from the TPL payer must be submitted with the request.
If the TPL payer is paying for the service, no authorization through the agency is required.
(For more information, see Authorization. For more information on TPL coverage, see the
agency’s ProviderOne billing and resource guide.
How do I bill claims electronically?
Instructions on how to bill Direct Data Entry (DDE) claims can be found on the agency’s Billers,
providers, and partners web page, under Webinars.
For information about billing Health Insurance Portability and Accountability Act (HIPAA)
Electronic Data Interchange (EDI) claims, see the ProviderOne 5010 companion guides on the
HIPAA electronic data interchange (EDI) web page.
The following claim instructions relate to Respiratory Care:
Name
Entry
Prior Authorization
Number
When applicable. If the service or hardware
being billed requires prior authorization, enter
the assigned number.
Place of Service
These are the only appropriate codes for this
program:
Facility Type To Be Used For
12 Home (client’s residence)
13 Assisted living facility
14 Group home
31 Skilled nursing facility
32 Nursing facility
99 Other
Respiratory Care
109
Name
Entry
Units
For multiple quantities of supplies, enter the
number of items dispensed and all of the dates or
dates spanned that the supplies were used.
Unless the procedure code description
specifically indicates pack, cans, bottles, or other
quantity, the each is each single item.
How does a provider bill for supplies?
When a provider bills for supplies that are limited to a specific number per day, the provider
needs to bill a span of dates that matches the number of units billed. For example, if a supply has
a limit of three per day, and the provider wants to bill for a 10-day supply, the provider would
need to bill for a span of dates that covers 10 days and the units billed should be 30.
• When a provider bills for a monthly rental, the provider must bill 30 days at a time unless
any of these situations occur:
It is a short-term rental (less than a month).
There is a break in service or eligibility for the client.
It is the last month the provider supplies the equipment to the client, and the client
did not have the equipment for 30 days.
Examples of correcting billing are:
The first month and day the client gets service is February 1, and the
provider will be continuing to bill for the rental. The provider should bill
for February, 2/1/20XX – 3/2/20XX (non-leap year); and then for March,
3/3/20XX – 4/1/20XX; for April, 4/2/20XX – 5/1/20XX; and for May,
5/2/20XX – 5/31/20XX.
The first month and day the client gets service is October 15 and the
provider will be continuing to bill for the rental. The provider should bill
for October, 10/15/20XX – 11/13/11; and then for November,
11/14/20XX – 12/13/20XX.
• When a provider bills for supplies that have no limit or are limited to a specific number
of units in a month, the provider should bill using just the date the supplies were
provided.
